Key Points
- •
Detection of cardiac standstill with bedside ultrasound can guide decision making regarding whether to continue resuscitative efforts.
- •
Point-of-care ultrasound can identify patients with pseudo-pulseless electrical activity, which is one of the great benefits of integrating ultrasound into resuscitation of cardiac arrest.
- •
Drainage of pericardial effusions detected by point-of-care ultrasound during resuscitation of cardiac arrest can be lifesaving.
Background
Point-of-care ultrasound is in use across most acute care settings. In 2010, both the American Heart Association and the European Resuscitation Council published recommendations supporting the use of ultrasound in cardiac arrest. In cardiac arrest, acute care providers regularly use ultrasound to inform the delivery, scope, and limits of resuscitative efforts. Further, point-of-care ultrasound commonly provides important diagnostic and procedural guidance for these patients.
It is important to have a defined strategy to incorporate ultrasound into the flow of advanced cardiac life support (ACLS). Providers must strategically position themselves at the bedside, select an appropriate transducer, and apply a well-defined algorithm with minimal disruption to cardiopulmonary resuscitation (CPR). The strategy and heuristics of point-of-care ultrasound in cardiac arrest are reviewed here. For techniques and details of specific ultrasound exams, refer to the appropriate, organ-specific chapter in this textbook.
Diagnostic Approach
During resuscitation of patients with cardiac arrest, the patient’s electrical rhythm directs the care team along prescribed management pathways consistent with ACLS guidelines. A focused ultrasound examination allows providers to search for correctable causes of cardiac arrest while CPR is in progress. The role of point-of-care ultrasound in cardiac arrest should vary according to the underlying cardiac rhythm.
Ventricular Fibrillation
If the cardiac rhythm is ventricular fibrillation or pulseless ventricular tachycardia, immediate defibrillation is indicated, and defibrillation should not be delayed to perform an ultrasound exam. On occasion, fine ventricular fibrillation may be detected with focused cardiac ultrasound that had been mistaken for asystole due to its fine nature. Although this circumstance is rare, recognizing the cardiac ultrasound appearance of ventricular fibrillation may avert an undesirable delay or deferral of defibrillation ( ![]() ).
).
Pulseless Electrical Activity/Asystole
Ultrasound has a large role to play when a patient’s rhythm is pulseless electrical activity (PEA) or asystole. PEA/asystolic arrests have a broad differential diagnosis, commonly disseminated as the five “H’s” and “T’s” listed in Table 42.1 . Many of these clinical syndromes are rapidly identifiable by point-of-care ultrasound.
| H’s | T’s |
|---|---|
| Hypovolemia | Tension pneumothorax |
| Hypoxia | Tamponade (cardiac) |
| H + ion (acidosis) | Toxins |
| Hypo/hyperkalemia | Thrombosis (pulmonary embolism) |
| Hypothermia | Thrombosis (myocardial infarction) |
Hypovolemia
Hypovolemic arrest should be considered when point-of-care ultrasound reveals evidence of an underfilled or dynamic inferior vena cava (IVC), intra-abdominal or intrapelvic free fluid, or abdominal aortic aneurysm. Patients in cardiac arrest typically receive positive-pressure ventilation either by bag-valve mask (BVM), supraglottic airway, or endotracheal tube via BVM. It is important to understand that the variation in breath-to-breath dynamics from BVM ventilation does not allow for accurate assessment of the IVC collapsibility index to address fluid responsiveness (see Chapter 18, Inferior Vena Cava ). Thus, in the case of cardiac arrest, a cruder approach is used with any collapsed or dynamic vena cava warranting aggressive fluid resuscitation ( ![]() ). If hypovolemia is supported by IVC findings, a sonographic search for its cause can be easily carried out despite ongoing CPR (
). If hypovolemia is supported by IVC findings, a sonographic search for its cause can be easily carried out despite ongoing CPR ( ![]() ).
).
When abdominal free fluid, pelvic fluid, or abdominal aortic aneurysm is identified during cardiac arrest, surgical consultation and administration of blood products may be considered, but prognosis is poor when surgical intervention is indicated.
Tension Pneumothorax
Tension pneumothorax is more commonly seen in trauma patients but may occasionally occur in patients with asthma or chronic obstructive pulmonary disease. Although it may be possible to determine the presence of lung sliding while CPR is in progress, scanning the pleura for lung sliding should be rapidly performed during a rhythm check, synchronized with delivery of breaths by BVM or ventilator. Presence of lung sliding excludes pneumothorax reliably at the area of insonation, whereas a loss of lung sliding supports but is not diagnostic of pneumothorax (see Chapter 10, Pleural Ultrasound Interpretation ).
In the setting of cardiac arrest, when pneumothorax is either supported by ultrasound or strongly suspected clinically, needle decompression or thoracostomy is indicated.
Cardiac Tamponade
Pericardial effusion appears as anechoic or hypoechoic fluid surrounding the heart. In the arrested patient, with ongoing CPR, we can easily identify the presence or absence ( ![]() ) of a significant pericardial effusion.
) of a significant pericardial effusion.
The presence of any pericardial effusion during cardiac arrest implicates tamponade as the etiology of arrest until proven otherwise. Resuscitative efforts should focus on immediate drainage of the effusion through a pericardiocentesis.
Pulmonary Embolism
Evidence of pulmonary embolism (PE) resulting in arrest may be seen on point-of-care ultrasound performed during resuscitation. In a nonarrested patient with pulmonary embolism, signs of PE include acute right heart strain and a grossly enlarged right ventricle accompanied by an enlarged IVC. In cardiac arrest, however, these findings may be seen in the absence of PE and are not specific. Sudden reduction in cardiac output due to arrest and subsequent infusion of intravenous fluids during resuscitation can lead to a relatively enlarged right ventricle, a plethoric IVC, and an underfilled left ventricle. If a thrombus is seen in the atria or ventricles, or in the femoral or popliteal veins, PE may be strongly suspected as the cause of arrest. Scanning the lower extremity veins for thrombus can be accomplished in patients while they are receiving chest compressions ( ![]() ). If clinical suspicion for PE is high, then thrombolysis clinical should be considered.
). If clinical suspicion for PE is high, then thrombolysis clinical should be considered.
Prognosis
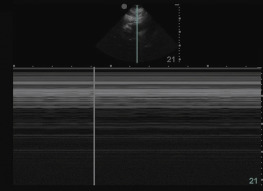
Although diagnostic and procedural ultrasound is critical to cardiac arrest survival, the most prevalent use of ultrasound in cardiac arrest is determining prognosis. Cardiac standstill seen on ultrasound ( Figure 42.1 ) has an exceedingly poor prognosis. Most studies have shown no survival when cardiac standstill is seen on an intra-arrest cardiac ultrasound. Of the few documented survivors of cardiac standstill, there have been no reports of survival to hospital discharge.
Technique
Probe Selection
Acquisition of ideal images during cardiac arrest would require the use of different transducer types with varying frequencies and designs. Because ultrasound imaging during cardiac arrest has several constraints yet must be efficient, a single, multifunctional transducer is required. With current ultrasound technology, a phased-array transducer with a small footprint is preferred, and a micro-convex or curvilinear transducer may be an acceptable alternative.
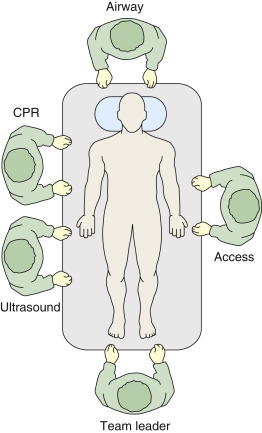
Positioning
In addition to selecting a single transducer, positioning of the sonographer and machine needs to be carefully considered. Resuscitation efforts run most efficiently when team members have designated positions and roles. Ideally, the sonographer should be a separate team member, not directly involved in the resuscitation, and this provider can independently acquire and interpret images to report back to the team leader. The best position for the sonographer is at the patient’s right hip, where the heart, lungs, abdomen, and lower extremity veins can be easily imaged ( Figure 42.2 ).