Abstract
Syphilis remains a significant infectious agent in pregnancy with the potential to cause fetal manifestations with maternal infection. Cases of congenital syphilis infection have recently increased, consistent with a resurgence of syphilis infections in the United States. All pregnant women should be screened for syphilis infection; many cases of congenital infection continue in women with scant or no prenatal care. Treatment with penicillin is highly effective in treating maternal cases, although some cases persist with incomplete or inadequate maternal treatment. High-resolution ultrasound (US) has the ability to prenatally diagnose many fetal signs of syphilis infection. The most common signs of fetal syphilis infection noted on prenatal US include fetal hepatomegaly, elevated middle cerebral artery peak systolic velocity, and placental thickening. Maternal treatment with penicillin therapy has the potential to resolve abnormal fetal US findings. Screening for maternal infection and sonographic screening for fetal sequelae are fundamental to provide appropriate maternal and fetal management to optimize pregnancy outcomes.
Keywords
syphilis, congenital, ultrasound, hepatomegaly
Introduction
A number of maternal perinatal infections result in congenital malformations. Traditionally these diseases were delineated by the acronym TORCH ( t oxoplasmosis, o ther, r ubella, c ytomegalovirus, and h erpes simplex virus). Syphilis has dominated the “other” category, although several other infections have increased over time, including coxsackievirus, human immunodeficiency virus (HIV), parvovirus B19, and varicella zoster virus. Syphilis is the quintessential bacterial infection that may cause observable pathology in the fetus and neonate following maternal infection; importantly, this pathology often resolves with adequate treatment of the mother. The use of ultrasound (US) for the identification of congenital syphilis in utero has come to the forefront in recent years with the introduction of US equipment with high resolution. This modality has helped to better define the pathophysiology of congenital syphilis and the fetal response to treatment. With the recent resurgence of primary and secondary syphilis in women in the United States and the resultant increase in congenital syphilis, the need for maternal syphilis screening and prenatal identification of congenital disease is paramount for appropriate management of both the mother and the fetus.
Disease
Definition
Syphilis is an infection caused by Treponema pallidum subsp . pallidum, a spirochete transmitted via either direct oral-genital or genital-genital contact through mucosal surfaces or by transplacental passage to a fetus. Congenital infection may occur as early as 9 to 10 weeks of gestation, though most of the clinical manifestations identifiable on US occur after 18 to 20 weeks’ gestation when the fetus starts to become immunocompetent. Maternal primary and secondary syphilis are associated with congenital syphilis transmission rates of up to 23% and 60%, respectively.
Prevalence and Epidemiology
According to the Centers for Disease Control and Prevention, there was a 28% increase in congenital syphilis in the United States from 2013 to 2014 (11.6 cases per 100,000 live births). This correlated with a 23% increase in the rate of primary and secondary infection during the same period. Twenty-two percent of infants diagnosed with congenital syphilis were born to mothers with no prenatal care. More worrisome is the fact that 59% of women who had prenatal care and yet delivered an infant with congenital syphilis were either not tested or did not receive appropriate treatment.
The highest rate of syphilis in women is in the reproductive age groups, 15 to 44 years of age. The greatest risk factors for syphilis in pregnancy include African American race, Hispanic ethnicity, young age, substance abuse, limited access to health care, poverty, prostitution, and inadequate prenatal care.
Etiology and Pathophysiology
Treponema pallidum subsp. pallidum is a macroaerophilic gram-negative motile spirochete 5–15 µm long and 0.1–0.15 µm in diameter. There are over 55 subtypes, only a few causing clinical disease in humans. Syphilis is able to avoid systemic immune detection and eradication by encoding multiple antigenic variants of its TprK outer membrane protein. This effectively evades humoral and cell-mediated responses. Eradication may occur when T cells activate CD68 + macrophages that phagocytose the antibody-coated treponemes.
Sexual transmission occurs when the spirochetes gain access through a break in a mucosal surface through genital-genital or oral-genital contact with an infected partner. The spirochete replicates locally in the primary stage (chancre) and then disseminates causing secondary infection. Transmission may also occur transplacentally or at the time of delivery to infect a fetus/neonate, causing congenital or neonatal syphilis infection.
Manifestations of Disease
Clinical Presentation
Although congenital syphilis may be detected prenatally, the findings are often nonspecific and may be seen with other TORCH infections. Postnatal examination and testing of the neonate and the placenta/umbilical cord is critical for accurate diagnosis.
Prenatal.
The consequences of congenital syphilis include premature delivery, low birth weight, nonimmune hydrops fetalis, and intrauterine demise. Suggestive US findings are discussed in the subsequent section on imaging.
Neonatal.
Two-thirds of live-born infants with congenital syphilis are asymptomatic; however, two-thirds of all untreated neonates exhibit symptoms by 3 to 8 weeks of life. Clinical manifestations may occur either within the first 2 years of life, with signs and symptoms similar to the inflammatory-driven manifestations of adult secondary syphilis or up to the first two decades of life, similar to gumma formation in bone, cardiac, and the central nervous system consistent with the chronic granulomatous inflammation typical of tertiary syphilis.
Early-stage congenital syphilis manifestations include hepatomegaly (51%–71%), maculopapular rash (41%–68%), fever (42%), neurosyphilis or cerebrospinal fluid abnormalities (23%–28%), pneumonitis (17%), rhinitis and snuffles (14%–23%), lymphadenopathy (14%–32%), and ascites (9%). Leukocytosis (72%), hemolytic anemia (34%–58%), thrombocytopenia (40%), jaundice (30%), pseudoparalysis (28%), renal disease (16%), and periostitis or osteochondritis (78%) may also be found. Skeletal findings are usually symmetric and multifocal and resolve spontaneously in the first 6 months of life. Hepatitis or pancreatitis may develop, with other possible gastrointestinal abnormalities such as ileitis or malabsorptive intestinal fibrosis. Skin may manifest pemphigus, with vesiculobullous lesions or condyloma lata. Mucous ulcers or fissures may also be seen. Neurosyphilis may develop later with acute leptomeningitis in the first few months or chronic meningosyphilis, causing progressive hydrocephalus, seizures, and neurodevelopmental regression later in neonatal life. Glomerulonephritis may result in nephrotic syndrome. Ophthalmologic findings may include chorioretinitis, glaucoma, or uveitis. Myocarditis, testicular masses, alopecia, and nail exfoliation are also seen.
Late-stage congenital syphilis occurs in 40% of untreated or incompletely treated survivors. These manifestations include saddle-nose deformity from rhinitis-related cartilage destruction (10%–30%); bowing and thickening of the brow, clavicle, midtibia, and/or scapula from prolonged periostitis (30%–95%); perforation of the hard palate (76%); peg-shaped, notched central incisors, and multicuspid first molars from vasculitis injury to tooth buds (55%); corneal scarring and glaucoma; interstitial keratitis (20%–50%); eighth cranial nerve deafness with high-frequency hearing loss between ages 8 and 10 years (3%–4%); and Clutton joints (hydrarthrosis of knees and elbows) (1%–5%). Asymptomatic neurosyphilis affects 25% to 33% of survivors of untreated congenital syphilis older than 2 years of age. Tabes dorsalis and cerebrovascular lesions develop in 1%–5% of children or adolescents.
Imaging Technique and Findings
Ultrasound.
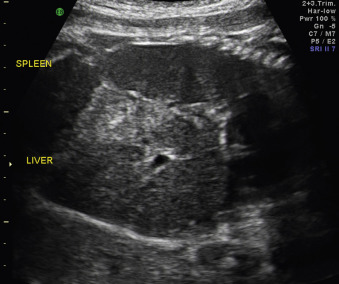
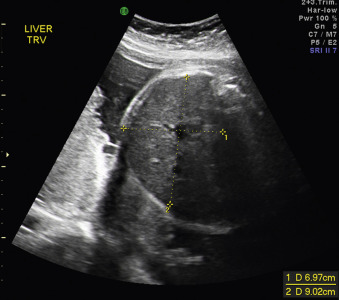
Although congenital syphilis can occur at any gestational age, US findings, if present, are noted after 18–20 weeks’ gestation. This is secondary to the required fetal inflammatory response necessary for the development of the characteristic abnormalities. Advancing maternal stage correlates with the US abnormalities seen. US findings of congenital syphilis most commonly include hepatomegaly ( Figs. 168.1 and 168.2 ) and placental thickening ( Figs. 168.3 and 168.4 ). Other findings such as ascites, skin edema, and polyhydramnios occur less frequently ( Figs. 168.5 and 168.6 ). Unusual findings include small bowel dilatation or hyperechogenicity. Long bones may be lagging in growth, irregularly shaped, bowed in multiple locations, or thickened ( Figs. 168.7 and 168.8 ). Doppler evaluation of the middle cerebral artery has been used to assess fetal anemia, a finding known to occur later in the progression of congenital syphilis. Elevated middle cerebral artery (MCA) peak systolic velocity (PSV) was found in almost one-third of infants with congenital syphilis.