Presentation and Presenting Images
( ▶ Fig. 97.1, ▶ Fig. 97.2, ▶ Fig. 97.3, ▶ Fig. 97.4, ▶ Fig. 97.5, ▶ Fig. 97.6)
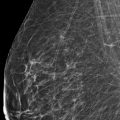
A 53-year-old female with a history of right breast cancer (invasive ductal carcinoma [IDC] and ductal carcinoma in situ [DCIS]) treated with a mastectomy and left breast reduction mammoplasty presents for diagnostic mammography.
97.2 Key Images
( ▶ Fig. 97.7, ▶ Fig. 97.8, ▶ Fig. 97.9)
97.2.1 Breast Tissue Density
There are scattered areas of fibroglandular density.
97.2.2 Imaging Findings
There is a 1.5-cm developing asymmetry in the posterior depth of the upper outer quadrant at the 2 o’clock location, 15 cm from the nipple (circle in ▶ Fig. 97.7, ▶ Fig. 97.8, and ▶ Fig. 97.9). An ultrasound was performed and did not reveal an imaging correlate (not shown). Because this developing asymmetry is seen mammographically, there is an option of biopsy with traditional stereotactic techniques or tomosynthesis-directed stereotactic techniques. Tomosynthesis-directed biopsy has additional advantages in localization of lesions, therefore this lesion was biopsied under tomosynthesis direction. Those images are presented next.
97.3 BI-RADS Classification and Action
Category 4A: Low suspicion for malignancy
97.4 Prebiopsy Images
97.4.1 Imaging Findings
Prebiopsy tomosynthesis confirms the developing asymmetry (circle) on slice 50 of 91 of the prebiopsy lateromedial (LM) digital breast tomosynthesis (DBT) movie ( ▶ Fig. 97.11). The developing asymmetry was targeted from the lateral projection.
97.5 Biopsy Images
97.5.1 Imaging Findings
These are the prefire tomosynthesis images in the -15 degree and +15 degree projections ( ▶ Fig. 97.12 and ▶ Fig. 97.13). There is a lidocaine effect in the area of the target. The biopsy was performed on an upright biopsy device located toward the anterior aspect of the breast, and the image was oriented as were the prebiopsy images ( ▶ Fig. 97.10 and ▶ Fig. 97.11).
97.6 Postbiopsy Images
( ▶ Fig. 97.14, ▶ Fig. 97.15, ▶ Fig. 97.16, ▶ Fig. 97.17, ▶ Fig. 97.18, ▶ Fig. 97.19)
97.6.1 Imaging Findings
Postbiopsy tomosynthesis confirms postbiopsy hematoma and adequate placement of the postbiopsy clip (circle) on slice 48 of 92 of the postbiopsy LM tomosynthesis movie ( ▶ Fig. 97.17) and slice 48 of 93 of the postbiopsy laterally exaggerated craniocaudal (XCCL) tomosynthesis movie ( ▶ Fig. 97.15). The postbiopsy mammogram ( ▶ Fig. 97.18 and ▶ Fig. 97.19) demonstrates the biopsy clip to be at the expected location of the developing asymmetry noted on the initial mammogram ( ▶ Fig. 97.7, ▶ Fig. 97.8, and ▶ Fig. 97.9).
97.7 Differential Diagnosis
Fibrocystic changes: Although the breast cancer risk was sufficient to recommend biopsy, not all developing asymmetries are malignancies. Leung and Sickles found that 8.5% of developing asymmetries found on screening mammograms were simple cysts.
Summation artifact: A summation artifact does not persist on imaging.
Breast cancer: Developing asymmetries warrant biopsies due to the increased risk of malignancy.
97.8 Essential Facts
A mammographic developing asymmetry is defined as a focal asymmetry that either is new or has increased in size or conspicuity compared with images from previous examinations.
A focal asymmetry is defined as a nonmass finding seen on at least two views and that occupies less than one quadrant.
Breast cancer risk in a developing asymmetry is sufficient to recommend biopsy even without a sonographic correlate, but not all developing asymmetries are malignancies.
Placement of a postbiopsy clip is important to demonstrate that the suspicious finding was adequately sampled. If the location of the postbiopsy clip does not correspond to the location of the prebiopsy finding, biopsy using mammographic guidance will need to be performed. It is important to alert the patient of this possibility.
97.9 Management and Digital Breast Tomosynthesis Principles
Although there are no current studies regarding DBT and developing asymmetries, tomosynthesis’s ability to eliminate superimposition of tissue and to visualize breast tissue in cross-section should allow for the identification and evaluation of developing asymmetries.
The purpose of sonography is to find a correlate for the mammographic finding and to guide biopsy. If ultrasound demonstrates no correlate, then stereotactic biopsy should be performed.
Leung and Sickles (2007) found that 25% of developing asymmetries have no sonographic correlate, so a negative ultrasound does not confer benignity.
97.10 Further Reading
[1] Leung JW, Sickles EA. Developing asymmetry identified on mammography: correlation with imaging outcome and pathologic findings. AJR Am J Roentgenol. 2007; 188(3): 667‐675 PubMed
[2] Price ER, Joe BN, Sickles EA. The developing asymmetry: revisiting a perceptual and diagnostic challenge. Radiology. 2015; 274(3): 642‐651 PubMed
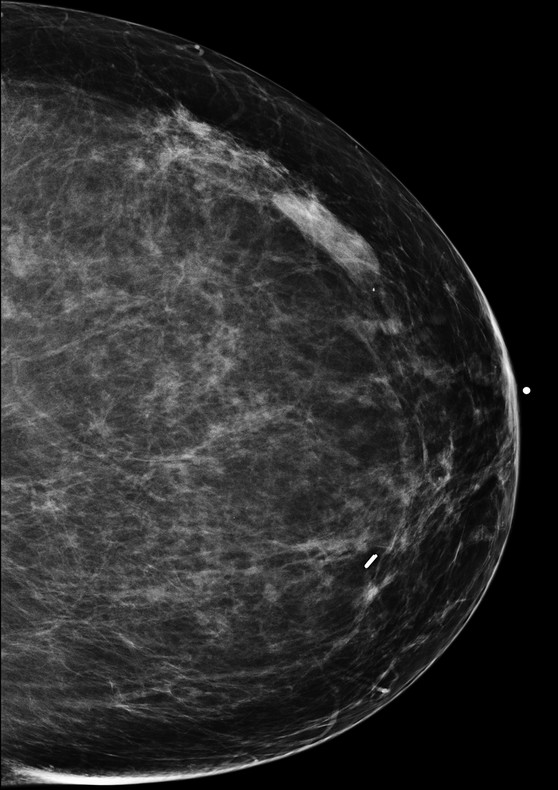
Fig. 97.1 Left craniocaudal (LCC) mammogram.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree