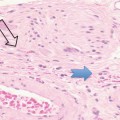
Fig. 2.1
Calculi (single arrows) cause dark acoustic shadow (double arrows)
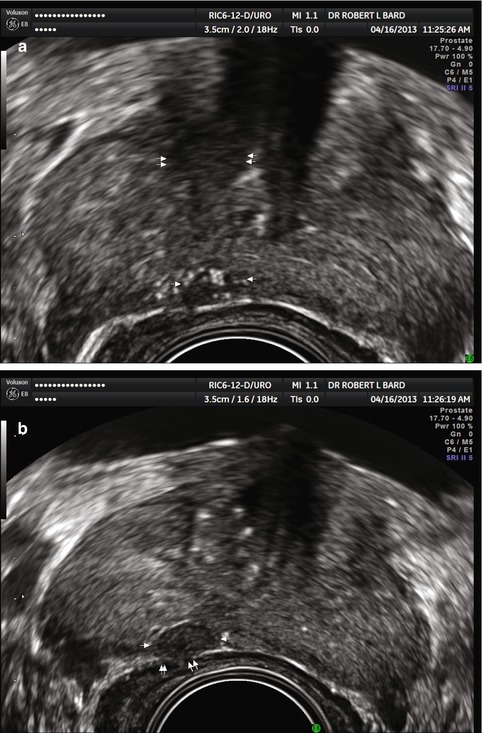
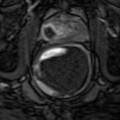
Fig. 2.2
(a) Presence of tumor microcalculi (arrows) scattered sound waves producing poor penetration and impaired resolution of anterior lesions (double arrows). (b) Shifting scan plane produces less attenuation and images posterior capsule erosion better (double arrows)
2.2.2 Attenuation
Attenuation is the loss of the energy as it undergoes continuous modification during its passage into and back from the tissues. This is a result of absorption, reflection, and scattering. Sound wave absorption is usually the dominant cause of decreased signal and occurs when the orderly particle movement characteristic of ultrasonic waveforms is converted to random vibration expressed as heat. Attenuation increases with increasing frequency and the ultrasound unit’s time gain compensation adjusts for this loss of echo intensity in accurate image reproduction. The use of ceramic composite elements led to the application of short acoustic pulses and increased bandwidth, called broadband transducers, which allowed for improved axial resolution without loss of signal penetration due to attenuation of sound energy as it passes through the tissues. This is accomplished by a spectrum of frequencies within a single probe, which allows the change of scanning parameters to adjust to the area under investigation. An example of this would be to scan the prostate at 18 MHz on a 10–16 broadband probe and then lower the frequency to 8 MHz to image the more distant bladder and seminal vesicles. While reducing the width of the US beam increases contrast and spatial resolution, focusing the beam is electronic and further adjusts and improves image quality. Spatial compounding and harmonic capabilities are standard on most new systems and further improve image quality.
2.2.3 Imaging Artifacts
If the sonic beam travels in a straight line going to a reflective interface and returning to the probe, at a constant velocity, and the beam width is uniform and extremely thin, then artifacts will not occur. While artifactual distortion may degrade the image, understanding of its true nature often serves as an alert and assists the experienced sonographer in refocusing on the area of pathology.
Specular echoes are faithfully and maximally returned when the interface is 90° to the insonating beam. This means that an interface at 0° or parallel to the beam may be not imaged. Most pelvic organ tissue interfaces are a mixture of specular and scattering surfaces so that diagnostic information will be returned at beam angles greater than 20° off the perpendicular axis.
Slice thickness artifacts occur when reflecting objects at the side of a beam profile appear as centrally positioned and may produce low-level echoes in cystic structures. These artifacts may cause trouble during biopsy and image-guided procedures if not recognized.
Reverberation artifacts from strong specular reflectors may be re-reflected and create a duplicate image or images at a deeper depth. This is common in cystic lesions where the ever-weakening signals are parallel to the initial surface and of a constant interval of distance with respect to each other. In the prostate, this occurs in the presence of metallic objects or gas bubbles and has the appearance of a bright streak of echoes. This descriptive picture has been referred to as the “comet tail sign” which often occurs when air-filled catheters are present in the urethra.
Velocity artifacts occur when the insonated region is different from normal tissues of fat, glands, cystic, or solid lesions. A specific case is the presence of silicone or similar filler used in augmentation that conducts sound waves half the speed of soft tissue. The returning images appear twice as deep as expected.
Shadowing and enhancement artifacts are commonly encountered in pelvic imaging. Acoustic shadowing occurs in three forms and is due to reduced or absent sound transmission through an overlying object. The most frequently encountered is reflective shadowing or sonic shadowing produced by an interface reflecting most or all of the transmitted beam and is produced by gas (air) or dense, extensive calcification which is often encountered following healed prostatitis. Microcalcifications, which occur in 5 % of prostate malignancies, often will be imaged without creating a sonic shadow artifact. Periurethral calcifications are centrally located and have an Eiffel Tower triangular appearance. These are usually readily distinguished as such and rarely cause diagnostic problems.
Absorptive shadowing (also called attenuative sonic shadowing) has a different mechanism due to the strong attenuation of sound by fibrotic tissue or desmoplastic tumor tissues. This is uncommon in prostate imaging but must be considered in postoperative glands or in the presence of highly malignant anaplastic tumors. Edge shadowing produces lateral shadowing around some solid masses but is not expected to occur in most prostate lesions.
Doppler artifacts, common in pulse wave spectral technologies, are not seen with the current formats of color, power, and angio Doppler in modern units. Pulse wave analysis may be used to interrogate postoperative arteriovenous fistulae, but will not be further discussed in the text. Color Doppler, which is directional (showing blood flow towards and away from the transducer), has largely been replaced by the nondirectional and more sensitive power and angio Doppler systems.
2.2.4 Scan Planes
Sonographic evaluation of the prostate and bladder may be performed via the transabdominal, transperineal, or transrectal approach. The transabdominal approach through distended urinary bladder gives an accurate measurement of the gland but lacks fine prostatic anatomic detail. Transperineal imaging may be applied when the transrectal approach is not feasible or when specific biopsy methods are entailed.
The transrectal approach is the most common today and transrectal US is commonly abbreviated as TRUS. This sonographic window allows for excellent imaging of the peripheral zone of the gland where 70 % of tumors occur as well as permitting ease of sonographically guided biopsy techniques. Before inserting the rectal probe, a visual inspection for hemorrhoids and a digital examination must be performed with a lubricated glove. Easier insertion of the covered transducer may be obtained when the patient is asked to either bear down or relax after a deep inhalation. There are biplane and end-fire probes available. The biplane probe allows imaging in both the transverse and sagittal planes, whereas the end-fire probe scans in one plane that is an oblique transverse plane between the true coronal and transverse planes. To obtain a sagittal view, the probe must be rotated 90°. The scan angle is important since a 180–195° opening will show the entire transverse or craniocaudal aspect of the gland. Many commercial units today have a 145° angle which may necessitate scanning both sides separately.
2.3 Gray-Scale Appearance of Prostate Cancer
Current prostate ultrasound imaging can accurately diagnose a large variety of common pathologies by using frequencies between 5 and 9 MHz with specially designed and focused end-fire one-plane or biplane (end-fire plus perpendicular fire) transducers. The prostate and adjacent structures are small and superficial in location and so are best examined with probes of high frequency. The higher the scanning frequency, the lower the sound penetration. For example, in measuring axial resolution, the discrimination between two points in the y-axis is 0.3 mm at 5 MHz, 0.15 mm at 10 MHz, 0.12 mm at 13 MHz, and 0.06 mm at 18 MHz. This results in improved resolution, but the loss of distal information may occur when scanning deeper structures such as the enlarged median lobe (central and transitional zone) or periprostatic lymph nodes.
Cysts or fluid-filled areas are without internal echoes and are called echo-free. Solid regions have internal echoes and are classified as echo poor or hypoechoic if there are few internal echoes. The term echogenic or hyperechoic is used if there are many internal echoes. Isoechoic means the lesion has the same echo pattern as the adjacent tissue. The colon mucosa appears highly echogenic as do the bony structures. Bone, air, foreign bodies, and calcification stop the transmission of sound waves producing a “sonic shadow” which is a dark region distal to the echogenic obstructing region. The term acoustical shadowing is also used to describe the low or absent echoes associated with these lesions. Acoustic window refers to an optimal placing of the transducers so that the areas of interest are clearly imaged and areas of artifact and shadowing (such as large areas of corpora amylacea, also known as prostatic microcalculi) are avoided. Acoustic windows are aided by the use of adequate gel inside and outside the prophylactic sheath covering the transducer and further maintained by water inflatable balloons designed to couple the rectal mucosa with the transducer.
Due to the presence of high anal tone, difficulty may occur in inserting the transducer. Insertion of the probe as the patient exhales is useful. If the insertion remains painful, instillation of lidocaine-permeated ultrasound gel by a specially designed syringe with blunt tip serves the dual purpose of adequately lubricating the mucosa and anesthetizing the adjacent tissues. If biopsy is considered or other image-guided treatment, 10 cc of lidocaine or Marcaine may be injected on both sides of the lateral pericapsular nerve bundles. Since the nerve bundles may be diffusely placed, moving the needle in an arc may be advantageous.
2.4 Color and Power Doppler Applications
Conventional pulsed and continuous wave Doppler exams are used to demonstrate and quantify blood flow velocities. However, these tests are extremely time consuming, highly operator dependent, and relatively insensitive. Color Doppler uses computer coding to demonstrate directional blood flows in a clinically useful manner. Power Doppler sonography (PDS), also called power Doppler imaging (PDI), is a new feature of blood flow analysis that is proportional to the total number of moving scatterers. This allows low flow states and minute vascular structures to be investigated. Advantages of PDS over color Doppler include:
(a)
Lack of aliasing artifact
(b)
Two to five times greater sensitivity to flow imaging
(c)
Information preservation with increasing perpendicularity of angle of beam incidence (Rizzato et al. 1995)
Current clinical PDS applications are the neovascular regions found in healing fractures, resolving hematomas, inflammatory tenosynovitis, and the detection of tumor vascularity that is associated with arteriovenous shunting, arterial malformations in size and caliber, increased vessel density, and various other vessel irregularities (Adler 1996; Campani 1997; Bard 1996). A 2002 major study on cancer imaging including sarcomas showed PDS to be useful in surgical planning decisions when a tumor was shown to be more or less aggressive than clinically suspected (Shulte 2000).
2.5 Prostate Cancer Diagnosis
Diagnosis of the most common cancer in the American male population has traditionally depended on digital rectal examination, PSA test, and TRUS (transrectal ultrasound) and, more recently, MRI. Digital rectal exam examines the periphery of the prostate, missing more centrally located lesions and extreme lateral tumors. Also, large areas of microcalculi, scars and fibrosis, or corpora amylacea may simulate a mass. PSA blood tests have been known to be falsely elevated in the presence of prostatitis and have been recently shown to be unable to definitively exclude prostate cancer. Indeed, the study of 3916 biopsies in 326 patients with PSA and TRUS showed that of the 127 patients with proven cancer, standard gray-scale TRUS correctly predicted cancer in 48 % of 326 patients studied while combined gray-scale TRUS with color Doppler imaging correctly predicted cancer in 64 %. A high PSA falsely predicted cancer in 30 % of men without malignancy. Using a threshold of 4 ng/ml, serum PSA correctly predicted cancer in 113 of 127 patients but falsely predicted cancer in 131 of 199 patients (Barish 1999).
These findings suggest the need for improved accuracy, which appears in the newer techniques of power Doppler imaging (PDS) and 3D TRUS imaging. A British study using 3D imaging to stage clinically localized prostate cancer where standard TRUS exams were 3 dimensionally reconstructed showed a 22 % increase in accuracy compared to standard TRUS when findings were compared with surgical and pathologic specimens. The technique was only useful in patients where the cancer was visible on conventional TRUS (Garg 1999) (Fig. 2.3).
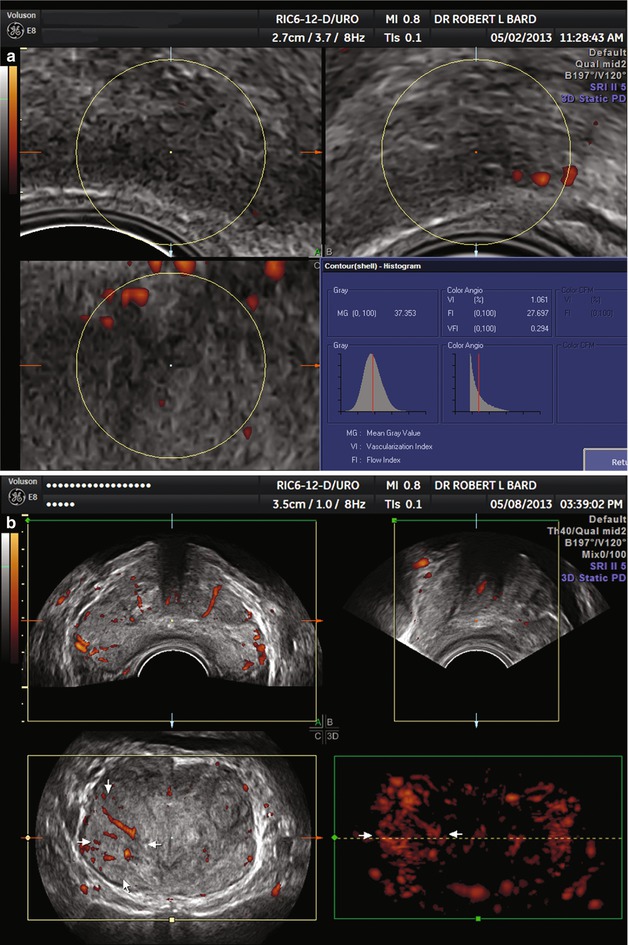
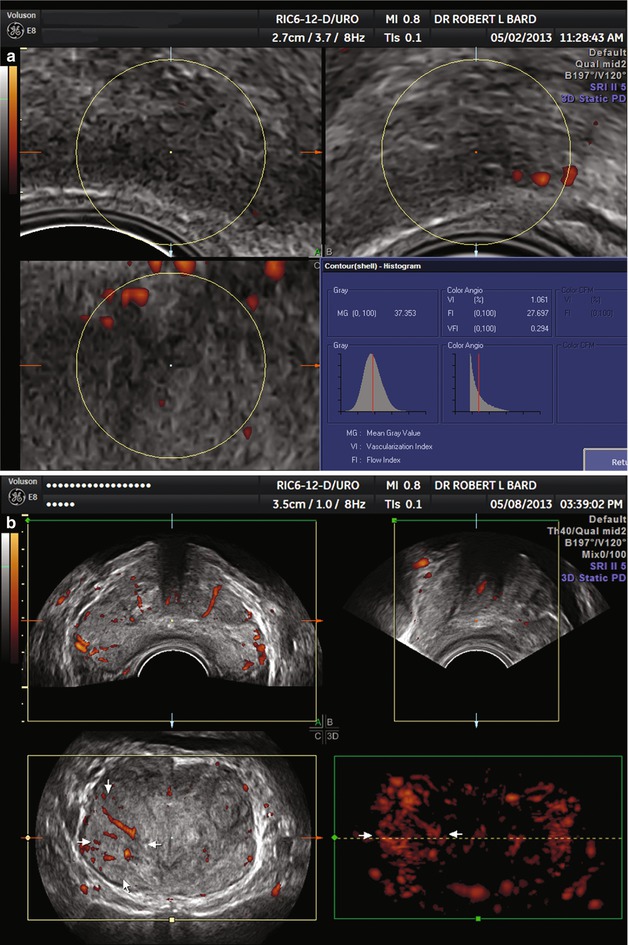
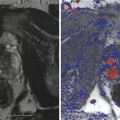
Fig. 2.3
(a) Low-grade cancer. Note absent flows and tumor is isoechoic. (b) High-grade cancer. Note high flows and tumor is isoechoic
Color Doppler imaging and power Doppler sonographic imaging are able to investigate cancers that do not appear clearly on standard gray-scale TRUS. Indeed, review of Doppler exams gives the physician a second look at areas initially determined to be unremarkable. Limitations of standard end-fire or biplane TRUS include misdiagnosis of cancers that are isoechoic and not imaged and false-positive diagnosis of hypoechoic areas. Approximately 25 % of malignancies are isoechoic (Alexander 1995).
A recent study showed that color Doppler imaging of 256 patients out of which 100 had biopsy-proven cancer showed tumors as the only modality in 16 %. These patients had Gleason scores of ranging between 5 and 8 with a mean of 6.4. However, it was found that 9 % of cancers (some of which were significant in size) were not discovered by either gray-scale TRUS or color Doppler imaging which used a low-velocity high-sensitivity color setting with a color filter optimized for low-velocity flow visualization of small vessels. The color window size was adjusted to cover the peripheral zone posteriorly allowing for a right and left comparison as well as deep enough to image most of the central and transitional zones (Lavoipierre et al. 1998).
Power Doppler sonography, with its higher sensitivity counterpart power angio Doppler, has been shown to differentiate between benign hypertrophy and malignant disease (Okihara et al. 1997). The sensitivity for malignancy diagnosis varies between 86 and 90 % (Cho et al. 1998). In a study of malignant disease, 22 patients with positive PDS findings were operated revealing 18 proven cancers and four false positives. Two cases were missed by PDS. The sensitivity was 90 % and the specificity was 75 % (Sakarya et al. 1998). This study underlines the necessity of proper imaging parameters so as not to be overly sensitive nor to be undersensitive in imaging blood flows.
The general consensus among imaging physicians is that a lack of blood flow in a suspicious area means the area is free of tumor or that the cancer is of low grade. A large study over 6 years using color Doppler imaging demonstrated that 24 out of 25 patients with cancer having low blood flows are free from biochemical relapse (rising PSA) after a mean of 31 months’ follow-up. Patients with high cancer blood vessel flow density were 10 times more likely to relapse following treatments (Ismail et al. 1997).
Benign tumor vessels usually start from a single vascular pedicle and have regular caliber arterial vessels with regular course and regular vascular distribution. Functional Doppler pressure flow parameters show one kind of flow in the tumor, that is, arterial blood flows with high to medium resistance. There is the absence of fresh small vessels. Malignant masses often have at least two or more feeding vascular pedicles that tend to penetrate the cancer at a more or less right angle. These arterial vessels have irregular caliber, course, and canalization. Fresh thin microvessels are noted. Arteriovenous shunts are demonstrable. Rapid changes of course with sharp angulations are present. A rich peripheral and slightly less dense internal vascularization is present unless there is central internal degeneration or necrosis. In this case peripheral neovascularization will be present and central vessels will be absent. This distinction is important for biopsy sampling, since a core from a necrotic area will not be diagnostically useful to the pathologist. Therefore, targeting the more vascular region will lead to more useful pathologic data analysis.
Functional Doppler shows vessels with variable resistance and variable velocity. Different types of flow are often noted within the same tumor (Campani 1995). The pathologist may use this same concept with the microscope. Microvessel tumor density is now being evaluated by immunohistochemical staining of blood vessels (Factor VIII-related antigen). Blood vessel density is an objective measurement of angiogenesis. Digital image analysis of the stained blood vessels may be quantified and put into an algorithm that predicts the probability of prostate cancer spread versus the probability of localized disease. This algorithm is called optimized microvessel tumor density, and it has now been used on over 10,000 patients nationwide on their biopsy specimens to provide appropriate patient management (Strum 1998).
Intense effort to discover new ways to demonstrate prostate cancer neovascularity is currently ongoing around the world. The use of contrast agents by injection has been shown in Europe to produce a 50 % increase in detection of abnormal blood vessels (Gajonova 1999). These agents are not yet approved by the FDA in the USA after a 10-year successful trial in European medical centers.
The normal prostate has thin arc-like vessels at the periphery (capsular region) and at the demarcation between the peripheral zone and the central zone. Central periurethral vessels are often noted and best imaged in longitudinal planes although these are rarely confused with tumor vessels. The vessels are symmetric and have regular course and slightly tapering caliber as it progresses distally along the urethra. Median lobe enlargement of benign nature and benign prostatic hypertrophy show enlargement of the vessels between the central zone and the peripheral zone. These vessels are symmetric and have regular course and caliber. Prostatitis has normal to slightly increased caliber vessels with high flow states. The vessels are widely separated by the edematous parenchyma. Cancers of low grade show increased number of vessels with some vessel caliber irregularity. There may be multiple feeding vessels of tortuous configuration in larger tumors. Cancers of high grade show increased vessel density, enlarged gross caliber, and course irregularity including sharp angulations of vessel trajectory. Malignancies with massive central internal necrosis caused by the tumor outgrowing its blood supply will show a rich peripheral neovascularization without vessels extending into or through the center of the mass. Cancers that have been treated successfully by radiation, cryosurgery, HIFU (high-intensity focused ultrasound), laser ablation, or certain nonsurgical methodologies may show an echogenic irregular region of fibrotic tissue conforming to the general region of the previously noted active malignancy. Extreme caution must be taken to avoid the brightly echogenic and color-producing regions of stones, corpora amylacea, or microcalculi. The gray-scale b scan must be checked before any region of abnormal blood flows is finally documented. Spectral PW (pulsed wave) Doppler in these regions will show the absence of arterial or venous flows and the presence of staccato-like reverberation artifacts distinctly different from true vessels and abnormal vessel configurations.
The blood supply to the prostate originates from the branch of the common iliac artery called the hypogastric artery. Branches from the anterior trunk give rise to the superior vesical, middle vesical, inferior vesical, middle hemorrhoidal, obturator, internal pudendal, and inferior gluteal arteries. The prostate is mainly supplied normally by the inferior vesical and middle hemorrhoidal arteries. These arteries surround the capsule and then travel linearly centrally to supply the interior of the gland in a central manner. The arteries have a specific functional component called pulsatility index (PI) related to the systolic and diastolic blood flows. It has been noted that breast cancer (the prostate and breast are both glands and have similar histologic features) local feeding blood vessels have greater flow volumes than the contralateral or normal vessels (Hollerweger 1997). A recent study showed the possibility of studying the regional prostatic vasculature by example of the breast cancer analogy demonstrating that the lateral thoracic artery in breast malignancies showed a significantly elevated PI difference in the cancerous breast (Obwegeser et al. 1999).
It is probable, in a similar manner, that new information evolving from the study of the major feeding prostatic blood vessels will lead to important diagnostic and prognostic possibilities. A further clinical application now being investigated is to selectively destroy the cancer by embolizing the feeding blood vessels via an arterial catheter or deliver high doses of chemotherapies via the same route. At this point a technical note of great importance must be introduced. As sensitive as PDS is to low flow states, excessive use of probe pressure will effectively reduce blood perfusion to undetectable states. This hemodynamic fact may be used in the case of significant post-biopsy hemorrhage. There are reports of uncontrolled rectal bleed post prostate biopsy being controlled and stopped by application of the biopsy probe to compress the ruptured vessels. Anecdotal reports and case studies cite the need to continue pressure for 60 min.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree