Film Interpretation and Report Writing
CRITERIA FOR ORDERING RADIOGRAPHS
Focus on Radiographs
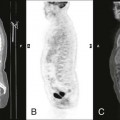
Since its inception, diagnostic imaging has played a fundamental role in patient evaluation. Diagnostic imaging began more than 100 years ago with the advent of plain film radiography, and has progressed to advanced modalities, such as digital radiography, magnetic resonance imaging (MRI), computed tomography (CT), and positron emission tomography (PET). Diagnostic imaging remains an essential tool to recognize, define, identify, and exclude many of the common and not-so-common pathologies encountered in a health care setting.
For most clinical assessments, the historically dominant plain film radiography continues to be the first step, with more sophisticated specialized imaging systems applied as follow-ups to negative, equivocal, or ambiguous results from the plain film study, or for clinical questions for which plain films are known to be insensitive. Plain film radiology is widely available, relatively inexpensive, and rapidly obtained, suggesting it will remain the most common imaging method for the near future.
Plain film radiology represents a common denominator between many health professions. Dentists, podiatrists, chiropractors, medical physicians, and many practitioners in the allied health professions routinely rely on information obtained from plain film radiographs to manage their patients. With this in mind, this chapter focuses on the interpretation and reporting of plain film radiographs. However, with little modification, the concepts presented here and targeted to plain film radiology equally relate to other specialized imaging modalities. Consequently, this chapter’s goal is to provide the reader with an understanding of issues related to when radiographs should be taken, methods to successfully search radiographs for abnormal findings, the ability to categorize these findings by appearance and location into common patterns, and steps to summarize and report on these findings successfully.
Common Uses of Radiographs
In 2009, an estimated $2.5 trillion was spent on personal health care in the United States.1 Health-care expenditure was 17.6% of the gross domestic product, representing a per capita expenditure of $8,086.1 Imaging is a growing portion of these costs. In 1990, an estimated 3.5% of health-care expenditures were for radiologic services.2,3 This percentage had grown to 9.1% in 2005, ranking it as the third largest health-care expenditure category after hospital care and physician services.4
Diagnostic imaging is common to clinical practice. Historically, more than 80% of chiropractors use radiographs as part of their clinical protocol and have the necessary equipment to produce radiographs in their offices.5 Although national data are not available, a survey of Minnesota medical physicians found that approximately 87% had onsite radiology equipment.6
Developing film interpretation skills is of obvious interest to radiologists, but developing these skills is also important to nonradiologist medical and chiropractic physicians, and other health-care providers who often take and interpret radiographs as part of patient evaluation and management. For instance, most chiropractors do not regularly consult with radiologists to assist their interpretations. In fact, fewer than 20% of hospitals have full-time onsite coverage by a board-certified radiologist.7 During these off hours, the initial interpretation and related decisions are often done by nonradiologist clinicians, most to be read by radiologists later. Moreover, of the radiologic services done in a private medical practice setting, 57%2,3 to 70%8,9 are performed and interpreted by nonradiologists.
Questions arise related to the appropriateness of the training of nonradiologists to interpret imaging and under what circumstance it is best to consult with a radiologist. The American College of Radiology (ACR) recommends that radiographs be interpreted by certified radiologists or physicians who have documented training in an approved residency, including radiographic training on all body areas. This indicates the basic need for formal training, but does not limit interpretations to radiologists.10 Literature within the chiropractic profession advocates for greater use of chiropractors who are certified with advanced training in radiology (Diplomates of the American Chiropractic Board of Radiology [DACBR]) as a method of limiting liability and enhancing accuracy of image interpretation.11
Taylor12 found that the degree of training positively influences the ability of medical and chiropractic clinicians and students to correctly identify selected bone and joint pathology. As one might expect, the concordance between the radiographic interpretation of radiologists and nonradiologists is best for extremity bone radiographs (approximately 95%) and lower for more complex studies, such as chest radiographs (generally ranging from 40% to 90%).*
Criteria for Ordering Radiographs
The most effective application of diagnostic imaging for common clinical presentations is widely debated. The multifaceted and unique clinical presentations of most patients make the formation of common criteria for ordering diagnostic imaging challenging. Everyone agrees that all radiographic examinations should follow clear historical and clinical indications because of examination costs and the potentially hazardous effect of ionizing radiation.13 Unfortunately, there is no general agreement on exactly what these historical and clinical indications should be to satisfy the competing needs of gaining information while limiting cost and radiation exposure.
To date, diverse opinion exists about what constitutes accepted clinical criteria for ordering radiographs for patients with musculoskeletal complaints. Although the literature contains many attempts to develop criteria for ordering radiographs for patients with complaints of the spine,† no system has been generally accepted. As a matter of observation, the use rates of plain film radiographs vary widely. Developing and embedding guidelines seem easier tasks for a narrow-scope presentation for something such as ankle14,15 or knee trauma,16,17 but are less successful for case presentations of increasing complexity and ambiguity (e.g., back pain) and applied management (e.g., pharmaceuticals versus manual adjustments or manipulation of the spine).†
Opinions vary widely about the use of radiographs in the evaluation of patients experiencing back pain. Multiple questions impact the issue. Should radiographs be taken for patients who are experiencing acute but not chronic back pain? What are the appropriate film-ordering criteria that maximize clinical information yet minimize patient cost and radiation exposure?
Despite the fact that these topics have garnered considerable attention over the past decade, evidence-based guidelines for the use of plain film radiology (or CT and MRI) are not widely used in the clinical setting. In 1987 the Quebec Task Force, and later the United States’ Agency for Health Care Policy and Research (AHCPR), developed guidelines for the use of plain film imaging related to patient presentation of acute low back pain. Similar efforts occurred in other countries.1,18,19 The premise is that guidelines effectively influence practitioners’ use of plain films, as has been shown to occur in some instances.20,21 However, guidelines prove less effective as the population and clinical problems become less homogeneous and more complex. Recent work by Bussierrès has advocated an evidence-based approach to developing radiography guidelines.22
Factors affecting whether radiographs are taken include clinical data, patient expectations, and clinicians’ attempts to reassure patients or themselves.23,24 Also the type of practitioner is very important: The use of radiographs for low back complaints varies from 2% to 48%, depending on the type of practitioner. Chiropractors—who employ a manual approach to patient care—and orthopedic specialists demonstrate increased use of plain film radiographs compared with medical physicians in family practice who manage patients with acute low back pain.25 This observation may result in part from a bias toward searching for a musculoskeletal derangement as the cause of the patient’s complaint; however, it also reflects varying therapeutic approaches to patient complaints and the need for structural information related to the delivery of care and patient management.
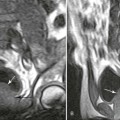
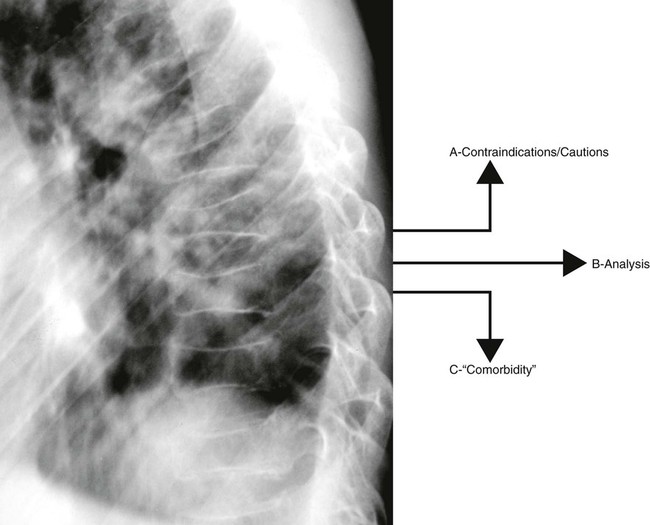
In chiropractic practice, radiographs are generally considered a standard first-step imaging protocol when evaluating degenerative and inflammatory joint disease, fractures, infections, and neoplasms.26 The hands-on management approach of chiropractors demands attention to biomechanical influences and potential structural contraindications for intended interventions (Fig. 5-1). Nonchiropractic clinicians, whose management of low back pain centers on exercise, patient education, pharmaceuticals, and other clinician-passive therapies, have less use for the biomechanical or structural information obtained from radiographs. Therefore, these practitioners can easily adopt a more conservative approach to taking radiographs for musculoskeletal spine complaints than can chiropractors or other practitioners, who apply manual intervention.
Many radiographs taken in a chiropractic setting are interpreted as normal for serious bone pathology,27 but may contain biomechanical or structural information allowing the chiropractor to be more successful with technical aspects of formulating and applying the patient’s management plan. However, more research into the reliability, validity, and clinical usefulness of biomechanical and structural information gleaned from radiographs is necessary. Also, evidence is needed to clearly justify the added costs, define criteria of patient selection, and facilitate advancements in care delivery.
All clinicians, regardless of therapeutic approach, are concerned with serious pathology appearing as routine low back pain. Clinical red flags suggesting the presence of serious pathology have been developed and are helpful for directing patient selection (Box 5-1). In the absence of these red flags, significant spinal pathology is estimated in only 1 of 2500 patients.28 Deyo and Diehl29 evaluated 1975 walk-in patients at a public hospital to estimate the prevalence of cancer as an underlying cause of patient back pain. Using an algorithm that generally reflects the questions listed in Box 5-1, only 22% of these patients would have received x-rays; this proportion includes all those who were later found to have cancer.
It should not be assumed that instituting guidelines, such as those listed in Box 5-1, will lead to less use. For example, Canadian researchers found that if the guidelines listed in Box 5-1 had been applied to their study population of 963 patients in a private medical family practice setting, 44% would have undergone radiography, increasing actual use by 238%. Considering patient follow-up, these researchers concluded that the sensitivity of the guidelines to detect fractures and tumors was higher than the physicians’ use patterns, but their specificity and positive predictive values were low.30
Parallel and similarly controversial issues surround the application of specialized imaging (e.g., whether MRI should be ordered for a patient in whom a disc herniation is clinically suspected yet neurologic findings are limited). This is especially true when approximately 25% of normal adults demonstrate acquired spinal stenosis and 33% have a disc herniation,31 two key MRI findings.
In the absence of clear guidelines, clinicians must adhere to a logical rule for the use of all diagnostic procedures: If the patient’s diagnosis or management is likely to significantly change from information routinely provided by the diagnostic procedure in question, then the study should be performed; if the necessary information is not routinely provided by the procedure or knowing the information obtained will not change the patient’s management, then the procedure should not be performed. This basic rule can be elaborated upon by an evidence-based approach to the decision. Similar to evidenced-based clinical practice generally, evidence-based radiology is an important approach to guide the practice of radiology. The clinician is encouraged to identify existing evidence in a systematic fashion, assimilate the information found in the context of the clinical question, and make a critical review of the strength of the evidence, and to recognize that the lack of evidence is not equivalent to negative evidence. Therefore, considerations of standards of practice and practitioner experience are important also.
Clinical decisions on radiology are then based on the best current evidence, clinical experience, and patient values.32 The information in Box 5-2 patterns the thought process behind an evidence-based approach through the presentation of a clinical decision rule.
Image Interpretation
Equipment and Resources
Before the skills and knowledge of the interpreter can be brought to task, the images should be clearly displayed and reference material should be close at hand. This is a digital age, but clearly the revolution has not permeated all segments of the population evenly. Although many clinics have moved to filmless methods for acquiring and displaying images, not all are as advanced. Much radiology, particularly plain film, is still accomplished traditionally; this produces radiographs that should be viewed on illuminated light boxes. These view boxes generally are available in two sizes, the standard 14 × 17-inch view box, and a larger 14 × 36-inch view box that accommodates a full spine radiograph, the type often used to assess scoliosis. Standard 14 ×17-inch view boxes are combined in various configurations to create a viewing station (Fig. 5-2).

High-volume centers may invest in a viewing system with rotating panels or belts that pass the films in front of a stationary bank of lights, because placing the films on and off the view box can consume a considerable amount of time. This system allows many cases to be stored and viewed quickly, without the need to shuffle through the films of each case as they are put on and off the view box.
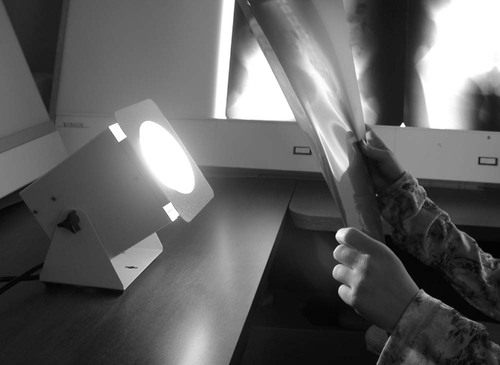
A “hot” or “bright” light is another important tool necessary for film interpretation (Fig. 5-3). The hot light produces a controllable high-intensity beam of light that helps the interpreter view the overexposed (dark or radiolucent) areas of the film. The intensity of the light can be controlled with a pedal that allows the interpreter to match the brightness of the light to the darkness of the radiograph. Even radiographs that are executed under the highest technical standard have regions of overexposed anatomy. Some of the more common and significant pathologies often hide in the overexposed areas of the film, making it difficult to recognize them when viewing the films only on a view box. Therefore, a hot light is an essential tool to a thorough film interpretation.
It has been said that “a radiologist without a ruler is a radiologist in trouble.”36 Although the sentiment underscores the importance of clinical intuition, observation, and training, the reality is that handy access to rulers, protractors, or other measuring devices allows more accurate quantification of structural abnormalities. For instance, the degree of spondylolisthesis is related to the likelihood of its further progression, the rate of growth of a pulmonary nodule predicts its malignant potential, the degree of scoliosis is central to the management of the case, and so on.
Reference texts should be close at hand. The usefulness of some radiology books transcend the typical, such as Keats’ Atlas of Normal Roentgen Variants That May Simulate Disease.37 A recent edition of Keats’ atlas should be close to the reading area. This book is a regional atlas of abnormal film findings that are normal variants of anatomy. It is comprehensive and includes both subtle and grossly abnormal cases. Recognizing that an abnormal finding is a normal variant saves time and examination costs related to erroneous additional evaluation. For example, view the case exhibited in Figure 5-4 of a 12-year-old with a history of trauma. The calcaneus clearly looks fractured, but the radiolucent defect actually represents an unfused secondary growth at the center of the calcaneal tuberosity. A similar case is noted in the third edition of Keats’ book.37 Recognizing that this is a normal variant and not a fracture ensures that time and expense are not wasted, nor that treatment is inappropriately provided.

Errors in Film Interpretation
Interpreter error may arise from a failure to see, recognize, or understand the significance of a lesion. Although error rates of 20% to 30% have been reported,38 the more contemporary literature indicates that approximately 1% to 3% of plain film interpretations done by nonradiologists contain important errors.‡ Most of these studies compare the film interpretations of attending emergency department physicians with planned overread interpretations of radiologists.39Seltzer40 estimates that 8% of interpretations by medical radiology residents contain potentially clinically important errors, which suggests that misinterpretation is increased in interpreters with fewer qualifications. Complex studies (e.g., CT)41 and studies on pediatric patients42 also increase misinterpretation. Fractures are the most often-missed lesions.43–45 Training is associated with more accurate interpretation,46,47 but radiologists are not immune to misinterpretation, as studied with various methods and imaging modalities.48–53 Most studies focus on false-negative readings; however, false-positive readings occur among radiologists43 and nonradiologists54 alike. False-positives promote continued patient evaluation, adding to cost, which is estimated to average $85 per false-positive reading.54 Unnecessary examinations also result in increased risk of complications associated with imaging.
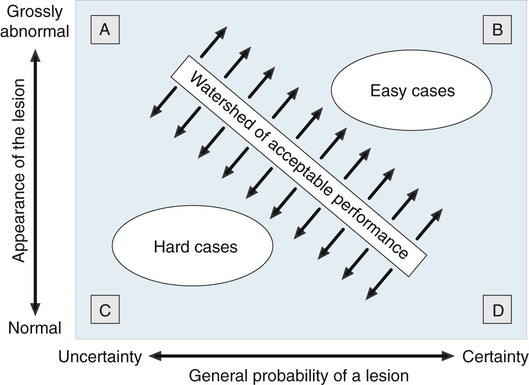
Alleged diagnostic errors account for the majority of legal cases related to radiology departments.55 However, not every missed lesion constitutes evidence of negligence. Statistics pointing to related rates of missed lesions, limitations of normal human visual perception, image quality, and many other factors influence image interpretation, and may be mitigating factors for image misinterpretation.55–62 The conceptual difference between errors in interpretation and those arising from perceptual variations is well described by Robinson.44 The former assumes the diagnosis is known and generally agreed upon as a lesion; the latter does not (Fig. 5-5).
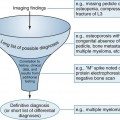
The goal of film interpretation is to eliminate as many misinterpretations as possible. There is a substantial literature addressing the topic of radiologic interpretation (Table 5-1). The literature and conventional wisdom indicate that although it is impossible to eliminate human error, and therefore mistakes of radiologic interpretation, attention to common principles should prove beneficial (Box 5-3).
TABLE 5-1
ANNOTATED BIBLIOGRAPHY OF SELECTED ARTICLES ADDRESSING RADIOLOGIC IMAGE INTERPRETATION
| Topic | Article | Summary |
| Ambient light | Alter AJ et al.65 | Employing low ambient room light, illuminating only films being viewed, and masking the radiograph around areas of interest improves visual performance; however, is cumbersome to implement completely in a clinical setting. |
| Appearance of the lesion | Krupinski EA et al.66 | This study found that physical features of pulmonary nodules do not attract attention as measured by “first-hit” fixation of the interpreter’s gaze; however, certain features do tend to hold the attention once the nodule has been fixated. The combination of all features influences whether or not it is detected. |
| Experience | Herman PG et al.48 | After having several interpreters view a series of chest radiographs, the authors found that, “Once an individual’s radiology education has progressed beyond a fundamental level, individual reader characteristics overshadow experience (and training) in the accuracy of chest film interpretation.” |
| Experience |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree