Key Points
- •
Point-of-care ultrasound is used to evaluate symptomatic pregnant patients in the first trimester to accurately exclude ectopic pregnancy using either a transabdominal or transvaginal approach.
- •
Combining clinical history, β-hCG level, and ultrasound findings can guide providers to the next most appropriate step in managing symptomatic first-trimester patients.
- •
Pregnancy failure, gestational trophoblastic disease, and placental disorders, such as placenta previa and placental abruption, may be detected with point-of-care ultrasound.
Background
Applications and Indications
Point-of-care pelvic ultrasound in the first trimester of pregnancy is most commonly performed in emergency departments (EDs) for symptomatic first-trimester patients. In this context, the most pressing application of point-of-care ultrasound is evaluation for possible ectopic pregnancy. This condition commonly presents with abdominal pain, pelvic pain, and vaginal bleeding in the first trimester. In some cases, patients may present in shock or after an episode of syncope. Ectopic pregnancy has been reported to occur in 2% of symptomatic first-trimester patients overall, but the prevalence is much higher in patients presenting to the ED, occurring in 8–10% of first-trimester patients. Ultrasound is used to indirectly exclude an ectopic pregnancy based on finding an intrauterine pregnancy (IUP) or, less commonly, to identify an ectopic pregnancy by visualization. Other first-trimester applications include detection of pregnancy failure, gestational trophoblastic disease, and in the later trimesters, placental disorders, such as placenta previa and placental abruption. Additionally, pelvic ultrasound can be used to evaluate potential causes of abdominal pain in the nonpregnant patient, such as ovarian cysts, tubo-ovarian abscess, ovarian torsion, and uterine fibroids.
Literature Review
Several studies have been performed to examine the diagnostic accuracy of point-of-care pelvic ultrasound and its utility for patients with suspected ectopic pregnancy. A meta-analysis combining ten studies of point-of-care pelvic ultrasound has been conducted and included a total of 2057 patients with an overall prevalence of ectopic pregnancy of 8%. The finding of IUP was considered a negative test for ectopic pregnancy, absence of IUP was considered a positive test, and the pooled estimate included a sensitivity of 99.3%, negative predictive value of 99.9%, and negative likelihood ratio of 0.08, suggesting that bedside ultrasound can be used as a screening test to exclude ectopic pregnancy. The specificity of ultrasound can vary depending on operator experience, ultrasound machine, and study protocol (i.e., transabdominal views alone or in combination with transvaginal views).
When an IUP is not visualized, experienced operators may be able to detect specific sonographic findings consistent with ectopic pregnancy. Examples include the identification of a tubal mass, sliding of the tubal mass away from the ovary, and free fluid in the right upper quadrant (RUQ). Experienced operators have shown the ability to detect ectopic pregnancy, as well as rupture, with a high degree of accuracy.
Point-of-care pelvic ultrasound has improved the care of pregnant patients in the first trimester. According to a recent national survey of ED ultrasound availability, patients with suspected ectopic pregnancy were 50% less likely to receive an ultrasound during off hours (evenings and weekends). Point-of-care ultrasound allows for around-the-clock access to pelvic ultrasound. Additionally, several studies have shown that finding an IUP on bedside ultrasound is associated with increased efficiency, as measured by decreased ED length of stay, especially during off hours.
Finally, point-of-care ultrasound allows physicians to evaluate unstable patients, rapidly identify patients with hemoperitoneum, and expedite care of those who require operative management for ectopic pregnancy.
Normal Anatomy
The uterus is a muscular organ that lies in the pelvis between the bladder and the rectum, measuring approximately 7 cm in length and 5 cm in width ( Figure 24.1 ). The cervix, or inferior portion of the uterus, protrudes into the vagina, and its long axis is generally angled anteriorly relative to the vagina. The part of the uterus superior to the cervix is known as the uterine body, which is normally anteflexed relative to the cervix. The fallopian tubes enter the body of the uterus laterally at the cornua, or uterine horns. The fundus is the portion of the uterus superior to the cornua.
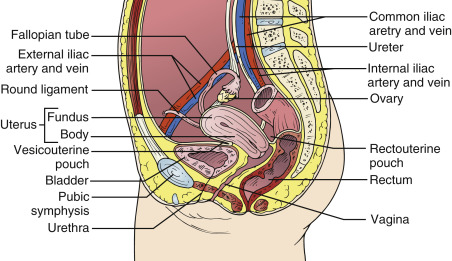
The vesicouterine pouch is the potential space bounded by the bladder and the anterior wall of the uterus. Between the rectum and the posterior wall of the uterus lies the rectouterine pouch, also known as the posterior cul-de-sac or pouch of Douglas. This space is usually filled by loops of small bowel. Intraperitoneal free fluid can be seen in either the vesicouterine or rectouterine pouches, although it accumulates first in the rectouterine pouch in supine patients.
In a nulliparous woman, each ovary is located near the lateral wall of the pelvis in the ovarian fossa. This space is bounded superiorly by the external iliac vessels, anteriorly by the broad ligament, and posteriorly by the internal iliac vessels and ureter. It is important to remember that the ovaries are displaced during pregnancy and their position can vary. The normal ovarian size ranges between 2 cm and 4 cm in its largest dimension. The central portion of the ovary, the medulla, contains vasculature, and the peripheral portion, the cortex, contains follicles and oocytes.
Image Acquisition
Transabdominal Technique
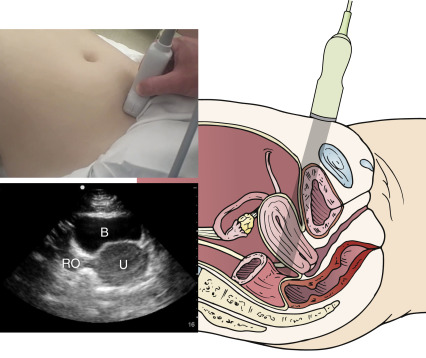
A curved-array transducer (2–5 MHz) is generally used for transabdominal pelvic scanning (TAS). Many machines have an obstetrical preset that can be selected for this exam. By convention, the screen indicator corresponding with the transducer marker should be located in the upper left side of the screen. Position the patient supine with the lower abdomen to the pubic symphysis exposed. A full bladder is preferred because it provides an acoustic window to visualize the uterus and adnexa. For a transverse view of the uterus, place the transducer immediately above the pubic symphysis with the transducer marker pointing to the patient’s right side ( Figure 24.2 ). A sagittal view is obtained in the same position by simply rotating the transducer 90 degrees clockwise with the transducer markernow pointing cephalad ( Figure 24.3 ).
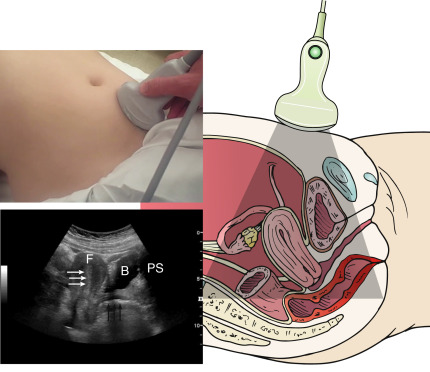
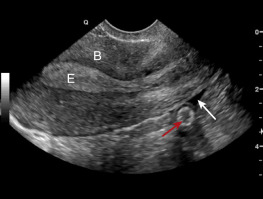
In a transverse orientation, a full bladder is seen in the near field with the uterus immediately posterior to it. The ovaries are seen to either side of the uterus, although it is not always possible to visualize both in a single image. Within the uterus, the myometrium surrounds the endometrium and is less echogenic by comparison. The thickness of the endometrium changes with the menstrual cycle. The endometrium develops a multilayered appearance following menstruation and gradually thickens during the proliferative phase. The endometrium reaches a maximum thickness of 16 mm in the late secretory phase, at which point it becomes hyperechoic throughout. It thins out again during menstruation, and fluid may be seen in the uterine cavity. The uterus may be interrogated from cervix to fundus by tilting the transducer superiorly and inferiorly with the ultrasound beam aimed into the pelvis.
In a sagittal orientation, the pubic bone may be seen on the top right of the screen casting a shadow into the far field (see Figure 24.3 ). The bladder is immediately posterior to the pubic symphysis and appears roughly triangular in shape. The body of the uterus lies posterior to the bladder and can be visualized along with the characteristic endometrial stripe, fundus, and cervix in a single image. The vaginal stripe is also seen in this view. The transducer can be fanned from left to right in order to obtain multiple oblique sections of the uterus. Sliding the transducer to either side and aiming the beam laterally also allows for identification of the ovaries.
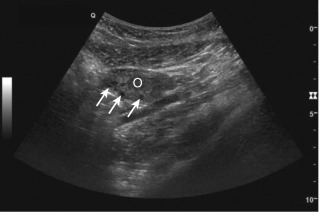
The normal ovaries appear spherical or elliptical and are relatively hypoechoic ( Figure 24.4 ). They are sometimes difficult to identify on TAS due to overlying bowel gas. The iliac vessels serve as useful landmarks, with the external iliac veins and artery coursing anterior and the internal iliacs posterior to the ovaries on either side. One may be able to visualize the anechoic follicles within the ovaries, although these are best appreciated on transvaginal imaging.
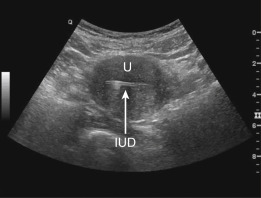
TAS suffices when the goal of the study is to exclude ectopic pregnancy by identifying an IUP. If the yolk sac can be visualized on TAS, it is unnecessary to proceed with transvaginal scanning. Furthermore, TAS provides a broad view of the pelvis and allows for visualization of structures in relation to the uterus; for example, the position of a gestational sac in the periphery of the uterus or outside of the uterus may be seen. An appropriately positioned intrauterine device (IUD) can be seen within the body of the uterus as a hyperechoic structure ( Figure 24.5 ). As discussed below, the TAS is usually the first approach to scanning the pelvis and is complementary to the transvaginal views.
Transvaginal Technique
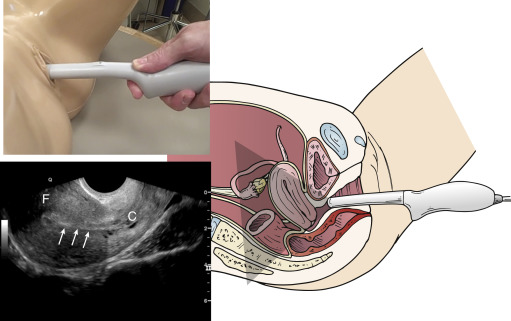
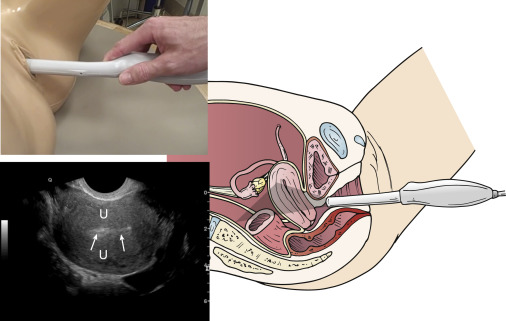
An intracavitary (5–8 MHz) probe is used for transvaginal scanning (TVS) of the pelvis. The patient should be placed in lithotomy position and with an empty bladder. Ultrasound gel is applied to the transducer, which is then covered with a sterile sheath before insertion in the vaginal canal.
Scanning starts with the transducer marker pointing toward the ceiling, resulting in a sagittal view of the uterus ( Figure 24.6 ). The decompressed bladder should be used as a landmark for probe insertion: the operator should insert the probe slowly until the bladder is visualized in the near field to the left on the screen. At this point, the uterine fundus should be seen in long axis, and the endometrial stripe can be seen toward the cervix ( ![]() ). Fanning the probe from side to side allows for interrogation of the entire uterus. Visualization of the cervix and the pouch of Douglas is accomplished by aiming the ultrasound beam posteriorly from a midline sagittal position. This area should be examined for the presence of free fluid, represented by an anechoic stripe posterior to the uterus ( Figure 24.7 ).
). Fanning the probe from side to side allows for interrogation of the entire uterus. Visualization of the cervix and the pouch of Douglas is accomplished by aiming the ultrasound beam posteriorly from a midline sagittal position. This area should be examined for the presence of free fluid, represented by an anechoic stripe posterior to the uterus ( Figure 24.7 ).
The ovaries can be found at either side of the uterus by fanning the probe laterally toward the pelvic wall. The external iliac vein will generally be seen adjacent to the ovary ( Figure 24.8 ). Within the ovary, follicles of varying sizes should be visible, reaching up to 25 mm in diameter.

Coronal views of the uterus and adnexa are obtained by returning to the midline sagittal position and rotating the transducer counterclockwise 90 degrees so the transducer marker is pointing toward the patient’s right side ( Figure 24.9 ). The uterus can be seen occupying the center of the screen with the ovaries present on either side. More commonly, only the uterus will be visible and the provider will have to direct the beam laterally to visualize each ovary ( ![]() ). The hand holding the transducer should be used to fan the ultrasound beam gradually through the uterus in an anteroposterior direction. Scanning the ovaries follows in a similar fashion, but the ultrasound beam is directed laterally instead of midline.
). The hand holding the transducer should be used to fan the ultrasound beam gradually through the uterus in an anteroposterior direction. Scanning the ovaries follows in a similar fashion, but the ultrasound beam is directed laterally instead of midline.
The utility of TVS lies in the ability to visualize intrauterine contents with high resolution. For example, transvaginal scanning allows identification of the yolk sac within a gestational sac earlier in pregnancy compared to TAS. Thus, the two techniques are complementary, with TAS providing a broad overview of pelvic contents and TVS providing a focused, high-resolution view of uterine contents.
Image Interpretation
Normal Findings
The appearance of a normal pregnancy on ultrasound follows a predictable course corresponding with the embryo’s gestational age. Thickening of the endometrium (>17 mm) is the first sonographic feature of pregnancy. It is, however, a nonspecific finding that can be seen in the late secretory phase as well as with ectopic pregnancy.
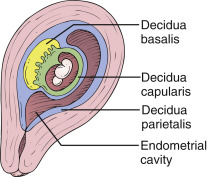
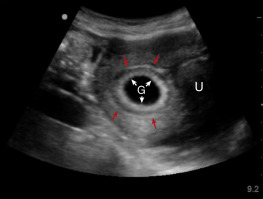
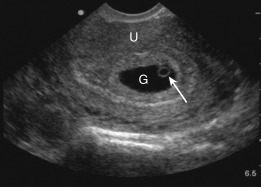
The next structure to be visualized is a gestational sac containing the chorionic cavity ( Figure 24.10 ). Early in pregnancy, it is challenging to differentiate a true gestational sac of an IUP from other structures of similar appearance, such as an endometrial cyst, hematoma, or pseudogestational sac. A pseudogestational sac contains fluid in the endometrial cavity and can been seen in the presence of an ectopic pregnancy. The gestational sac appears as a hypoechoic oval structure surrounded by an echogenic ring, the decidua capsularis. The following criteria have been suggested to help identify a true gestational sac: location in the uterine fundus, elliptical shape, eccentric to the endometrial canal, presence of a decidual reaction >2 mm, and diameter >4 mm.

Another finding that is suggestive of an IUP is the intradecidual sign. This is first seen at approximately 4.5 weeks and is composed of a small gestational sac embedded in the endometrium with uterine stripe passing unaltered on one side of the sac ( Figure 24.11 ). Although it was initially proposed as a diagnostic criterion for IUP, the intradecidual sign has been found in cases of ectopic pregnancy and is now considered to be unreliable.

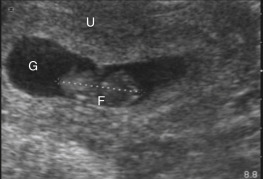
A more dependable finding is the double decidual sac sign. This is first seen on transvaginal ultrasound at a gestational age of approximately 5 weeks and is strongly suggestive of an IUP. The double decidual sac sign is present when the decidua capsularis (inner echogenic ring) is separated by a hypoechoic stripe (the endometrial cavity) from the decidua parietalis (outer echogenic ring) ( Figures 24.12 and 24.13 ). Although, when seen, it is considered by some as diagnostic of IUP, the double decidual sac sign is not always present even in normal pregnancies.
The next structure to appear is the yolk sac. It appears as an echogenic ring with an anechoic center located inside the gestational sac ( Figure 24.14 and ![]() ). Identification of a yolk sac is important because a gestational sac containing a yolk sac is the first definitive evidence of an IUP. The yolk sac diameter increases in size to a maximum of 6 mm at week 10 and subsequently involutes, disappearing completely by week 12. One should be able to visualize a yolk sac when the gestational sac is greater than 8 mm in diameter.
). Identification of a yolk sac is important because a gestational sac containing a yolk sac is the first definitive evidence of an IUP. The yolk sac diameter increases in size to a maximum of 6 mm at week 10 and subsequently involutes, disappearing completely by week 12. One should be able to visualize a yolk sac when the gestational sac is greater than 8 mm in diameter.
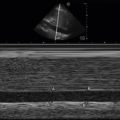
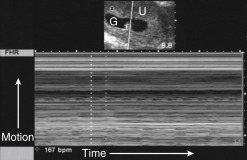
The fetal pole, or embryo, can usually be seen as a 2-mm small discoid mass adjacent to the yolk sac shortly after the fifth week of gestation. Once the gestational sac reaches a diameter of 18 mm, it should always contain a visible fetal pole. At approximately 6 weeks, cardiac activity is seen within the embryo. The crown–rump length (CRL) represents the longest dimension of the embryo and is used to estimate gestational age in the first trimester ( Figure 24.15 ). When CRL >5 mm, a living embryo will always have identifiable cardiac activity. M-mode is used to determine fetal heart rate, which should be between 110 and 175 beats per minute (bpm) in the first trimester ( Figure 24.16 ). A fetal heart rate within normal range predicts a greater than 90% chance of progression to term. Indeed, even in cases of threatened abortion some studies have found a greater than 90% chance of successful pregnancy once fetal cardiac activity was demonstrated.
The amnion, seen as a separate anechoic space within the gestational sac, is initially difficult to visualize but is usually apparent by week 7. It should not be confused with a yolk sac ( Figure 24.17 ). The amnion contains the embryo, and identifying an amniotic sac without an embryo is diagnostic of a failed pregnancy. This is known as “empty amnion sign.” The chorionic cavity within the gestational sac is eventually obliterated as the amnion expands and fuses with the chorionic margin, a process that is usually completed by week 12.
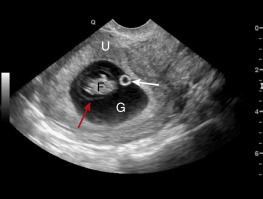
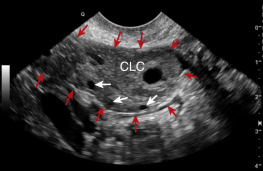
Finally, the corpus luteum, or a corpus luteum cyst, may be visualized within one of the ovaries ( Figure 24.18 and ![]() ). The corpus luteum forms from the ruptured follicle after ovulation and functions to support the pregnancy during the first trimester. When the corpus luteum becomes cystic, it may be confused with an ectopic pregnancy. Additionally, pelvic pain may be experienced if the corpus luteum ruptures or enlarges enough to cause ovarian torsion.
). The corpus luteum forms from the ruptured follicle after ovulation and functions to support the pregnancy during the first trimester. When the corpus luteum becomes cystic, it may be confused with an ectopic pregnancy. Additionally, pelvic pain may be experienced if the corpus luteum ruptures or enlarges enough to cause ovarian torsion.