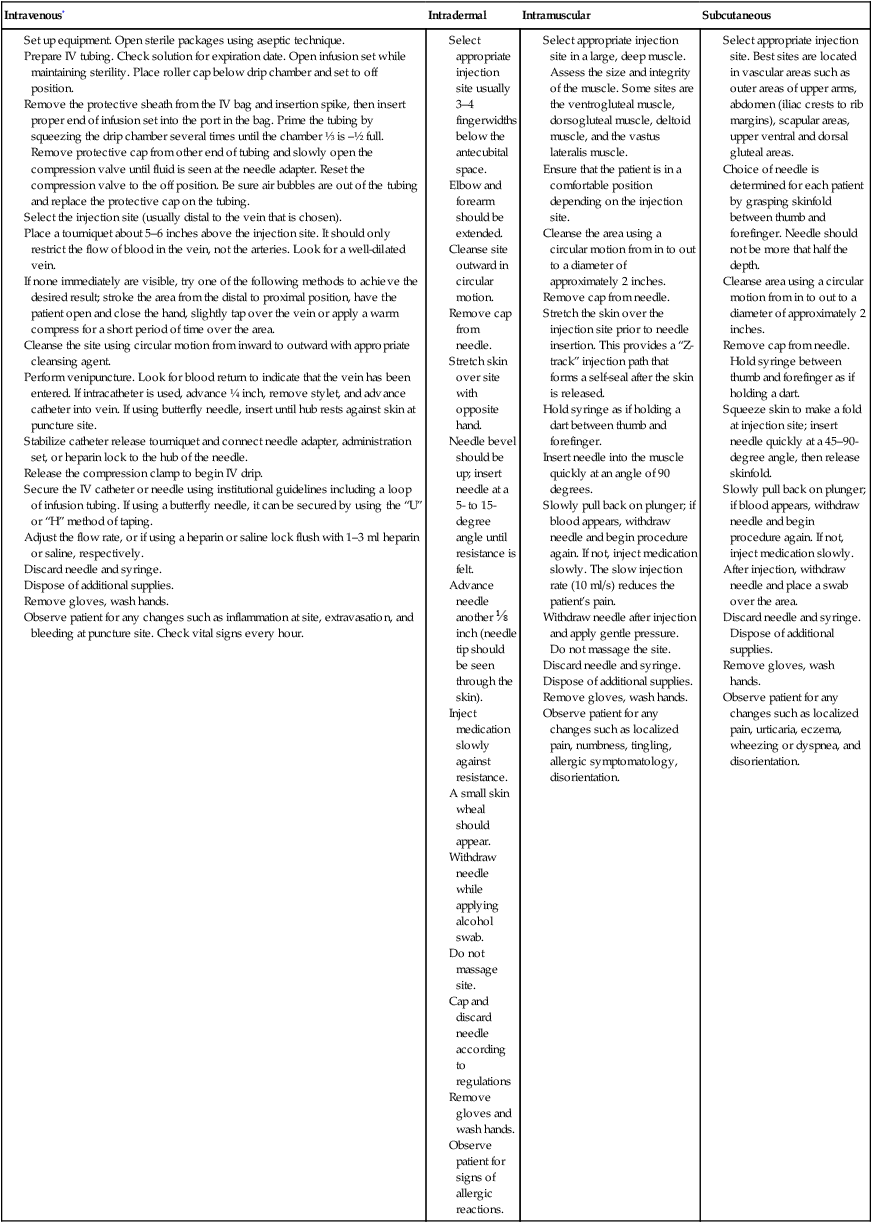
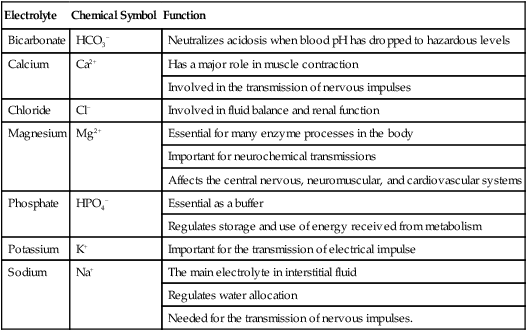
CHAPTER 5 After completing this chapter, the reader will be able to perform the following: The American Registry of Radiologic Technologists (ARRT) requires the candidate for the advanced level examinations to have some understanding regarding the types and administration routes, indications, contraindications, and complications of various drugs used in cardiac and vascular interventional radiography.1 Contrast agents represent a special category of materials; they will be discussed separately in Chapter 6. The local medications are usually administered at a specific site and are injected into the tissues only in that particular area. The route is by direct injection, and the purpose of the drug is the reduction of sensation (pain) in the tissues of the surrounding area. These drugs are used at the beginning of the procedure, and they have an anesthetic and analgesic effect at the puncture site. The anesthetic effect of the “local” medication is almost immediate and is well tolerated by most adult patients. Box 5-1 lists some local anesthetics. Occasionally, one of the amides will be added to the contrast agent to reduce the discomfort and pain associated with the injection. There are five subdivisions of parenteral administration of medication: intravenous, intramuscular, intrathecal, intradermal, and subcutaneous. Each of these methods requires the use of a needle and usually a syringe. Intravenous (IV) fluid therapy is the exception to the use of a syringe as a part of the process. Refer to Chapter 4 for the discussion regarding needles and syringes. Each of the parenteral routes of administration is similar in that the object of the procedure is to place a needle into a specific part of the body. Table 5-1 summarizes the locations for the injections as well as any specifics about the process. TABLE 5-1 Summary of Parenteral Routes of Injection In this section we will discuss the general guidelines for the administration of parenteral medication. Table 5-1 illustrates the major differences in the various parenteral routes of medication administration. As mentioned earlier, medications can be administered to the patient in a variety of different ways: oral, rectal, topical, inhalation, and parenteral. The parenteral route of drug administration is subdivided into five separate areas: intravenous, intradermal, intrathecal, subcutaneous, and intramuscular. When any medication is administered it is important to follow some basic principles, known as the “Six Rights.”2 These basic rules should be followed whenever any medication is dispensed to a patient. Many of the guidelines listed here are the same for routine patient care and communication. The difference is that all of the vascular and cardiac interventional procedures are invasive and have the potential to produce a number of different reactions. Extreme care should be exercised in adhering to these rules and guides. In almost every case some type of medication is administered to the patient before, during, or after a procedure. It is the responsibility of everyone on the team to practice a heightened level of care in order to ensure patient safety from medication reactions due to human error. The Institute for Safe Medication Practices (ISMP) has identified some common medications that have been known to cause an increased risk for patient injury when errors are made. The organization recommends that when any of these drugs are administered safety strategies are in place to prevent any errors. Box 5-2 summarizes the ISMP List of High Alert Medications.3 Table 5-2 lists the procedures for each of the parenteral routes of administration with the exception of the intrathecal route, which is discussed in detail in Chapter 21. TABLE 5-2 Generalized Guidelines for Parenteral Administration of Medication *A discussion of venipuncture and the use of heparin or normal saline locks is presented in the section, “Intravenous Therapy.” The main purpose of this type of therapy is the management of the fluids in the body. The body is composed of over 65% water, and fluid management is vitally important for the balance of electrolytes, blood volume, and other nutritional materials required for intra- and extracellular equilibrium. In the normal, healthy patient this is accomplished automatically even under situations in which there is a minor fluid loss. Extracellular fluids are the body fluids consisting of the interstitial fluid and blood plasma. Approximately one quarter of the body’s water is located outside the cells. Most of this water is found in the interstitial space. Interstitial fluid fills the spaces between most of the cells of the body. Less than 8% of the body’s fluid is located in the intravascular space. Three quarters of all the water is found within the cells of the body. These intracellular fluids are within cell membranes throughout the body and contain dissolved solutes essential to fluid and electrolyte balance and metabolism. Electrolytes are substances that ionize when dissolved in water and as such are able to conduct a current. Calcium is an electrolyte that is necessary for the conduction of nerve impulses responsible for the contraction of skeletal muscle. All of these substances are necessary for normal body metabolism. Table 5-3 lists the various electrolytes present in the body’s fluids. TABLE 5-3 Major Electrolytes and Their Function in the Body Intravenous therapy when used during advanced radiologic procedures serves several functions. Among these functions, the intravenous port provides a ready access to the vein for the rapid introduction of emergency medication; however, fluid management is the primary purpose, especially when contrast agents are administered. The patient should be well hydrated during contrast examinations to reduce the probability of an adverse reaction. The patient’s condition and the type and amount of contrast agent will govern the type and flow rate of the intravenous fluid. Box 5-3 summarizes the reasons that IV therapy is employed.
Introduction to Pharmacology
 Define common terms used in pharmacology
Define common terms used in pharmacology
 List the routes of administration of pharmacologic agents
List the routes of administration of pharmacologic agents
 Identify the general guidelines for drug administration
Identify the general guidelines for drug administration
 Identify the principles of intravenous (IV) therapy as well as the complications and equipment associated with it
Identify the principles of intravenous (IV) therapy as well as the complications and equipment associated with it
 Differentiate between osmolality and osmolarity
Differentiate between osmolality and osmolarity
 Define the principle of venipuncture
Define the principle of venipuncture
 Describe the calculations for intravenous flow rates
Describe the calculations for intravenous flow rates
 Identify the various types of pharmacologic agents used in conjunction with the advanced radiographic and interventional procedures
Identify the various types of pharmacologic agents used in conjunction with the advanced radiographic and interventional procedures
 List the medications that could be used in cases of cardiac or respiratory emergencies
List the medications that could be used in cases of cardiac or respiratory emergencies
ROUTES OF ADMINISTRATION
Parenteral Route
Description
Specific Criteria
Intravenous
Insertion of a needle into a vein
Needle held at 15–30-degree angle to patient’s arm with needle bevel up. Use the smallest needle size for the product to minimize tissue damage. Most common sizes are 16–18 gauge.
Intramuscular
Insertion of a needle into a muscle
Use a 21–23 gauge needle (1½ inches) to ensure passage into deep muscle tissue.
Needle is held at a 90-degree angle.
Intrathecal (intraspinal)
Insertion of a needle into the subdural, arachnoid, or lumbar areas.
Use a 16–25-gauge, 3½ inch long spinal needle.
Intradermal
Insertion of a needle into the dermis
A small syringe or needle combination is used, 26–27 gauge, ¼ to ½ inch needle. The angle of insertion is 5–15 degrees.
Subcutaneous
Insertion of a needle into the loose connective tissue directly under the dermis
Use a 25-gauge, ⅝ inch needle. An angle of 45–90 degrees can be used depending upon the body habitus of the patient. Larger, obese patients will require a 90-degree angle for insertion.
General Guidelines for Parenteral Medication Administration
Intravenous Therapy
Electrolyte
Chemical Symbol
Function
Bicarbonate
HCO3−
Neutralizes acidosis when blood pH has dropped to hazardous levels
Calcium
Ca2+
Has a major role in muscle contraction
Involved in the transmission of nervous impulses
Chloride
Cl−
Involved in fluid balance and renal function
Magnesium
Mg2+
Essential for many enzyme processes in the body
Important for neurochemical transmissions
Affects the central nervous, neuromuscular, and cardiovascular systems
Phosphate
HPO4−
Essential as a buffer
Regulates storage and use of energy received from metabolism
Potassium
K+
Important for the transmission of electrical impulse
Sodium
Na+
The main electrolyte in interstitial fluid
Regulates water allocation
Needed for the transmission of nervous impulses.
Osmolarity and Osmolality
Get Clinical Tree app for offline access




































 inch (needle tip should be seen through the skin).
inch (needle tip should be seen through the skin).