NASOPHARYNX: MALIGNANT TUMORS
KEY POINTS
- Computed tomography and magnetic resonance imaging are critical tools in the evaluation of known and suspected nasopharyngeal malignancies as well as in posttreatment surveillance.
- Imaging-guided biopsy can help in the diagnosis if endoscopic biopsy is not definitive.
- Fluorine-18 2-fluoro-2-deoxy-D-glucose positron emission tomography (FDG-PET) should be used judiciously rather that routinely in the evaluation of this and other head and neck–region cancers.
Nasopharynx cancer accounts for only a small percentage of all head and neck malignancies in the United States. Diagnosis is often delayed until the patient sees an otolaryngologist for a definitive examination of the nasopharynx. Even with such a skilled examination, sometimes entirely submucosal cancers can be difficult to diagnose until the strong clinical suspicion of the disease leads to a diagnostic computed tomography (CT) or magnetic resonance imaging (MRI) study.
About 85% of nasopharyngeal malignancies are carcinoma, while 10% are lymphoma. Remaining uncommon malignant tumors of the nasopharynx or adjacent sites include adenoid cystic carcinoma, adenocarcinoma, sarcoma (primarily rhabdomyosarcomas in children), plasmacytoma, and melanoma.
ANATOMIC AND DEVELOPMENTAL CONSIDERATIONS
Embryology
There is no direct link between nasopharynx malignancies and embryology except that adenoid cystic or other adenocarcinomas likely arise from submucosal rests of minor salivary glands remaining in the submucosa and parapharyngeal space during developmental migration of that tissue (Figs. 188.1 and 188.2). This can be a source of entirely submucosal nasopharyngeal carcinoma that will remain undiagnosed until imaging raises this as a possibility and then may be used to guide confirmatory tissue sampling since a mucosal site for biopsy will not be apparent on physical examination. This submucosal origin may also be due to mesenchymal-origin tumors or other cells that typically lie deep to the mucosa even within the adenoidal epithelial line crypts (Fig. 188.3)
Applied Anatomy
The critical anatomy in the nasopharynx that must be understood to adequately evaluate cancer in the region includes the following areas:
With regard to local mucosal and soft tissue extension:
- Complete understanding of the mucosal landmarks within the nasopharynx, including the eustachian tube, torus tubarius, and fossa of Rosenmüller and their relationship to the adjacent parapharyngeal space and pharyngeal musculature including the tensor and levator palatal muscles and the more lateral masticator space and infratemporal fossa and inferiorly the oropharynx. The relationships of the retropharyngeal space and prevertebral muscles must also be understood. The normal variations of its lining lymphoid tissue and the meaning of anatomic variants such as the Thornwaldt cyst are also required knowledge (Chapters 184 and 185).
- Relationship of the soft tissue boundaries of the nasopharynx and conduits to the skull base, posterior nasal cavity (Chapter 78), sphenoid sinus, and orbits (Chapter 44).
With regard to invasion of bony structures:
- Central skull base including the basisphenoid and basiocciput (upper and lower clivus) and pterygoid processes and plates; inferior petrous apex and petroclival fissure; and foramen lacerum (Chapter 78).
- Hard palate (Chapters 190 and 196), sinuses (Chapter 78), and orbit (Chapter 44).
With regard to possible routes of perineural and/or perivascular spread:
- Patterns of cancer spread to the carotid canal, sphenopalatine foramen, pterygopalatine fossa, vidian canal, foramen rotundum, and foramen ovale; the entire extracranial course of V2 and V3; superior and inferior orbital fissure, cavernous sinus, and courses of cranial nerves III, IV, and VI; greater and lesser palatine foramina and related nerves; and cranial (IX–VII) and sympathetic nerves within the retrostyloid parapharyngeal space (RSPS) (refer to Chapter 21 for perineural patterns and Chapter 184 for related anatomy).
With regard to regional lymph node involvement:
- Retropharyngeal nodes; cervical nodes, mainly levels 2 through and including 5; and the parotid nodes. Parotid-area lymph nodes are rarely involved (Chapter 149).
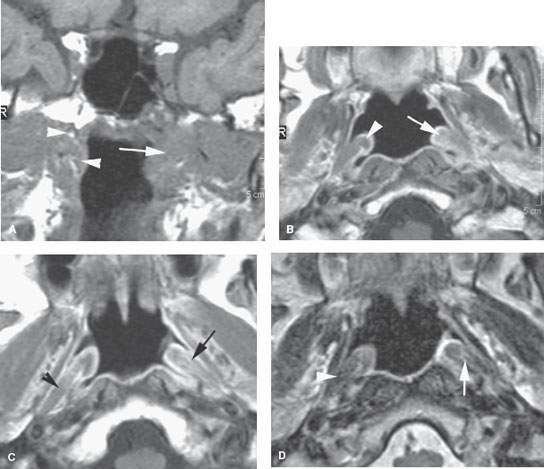
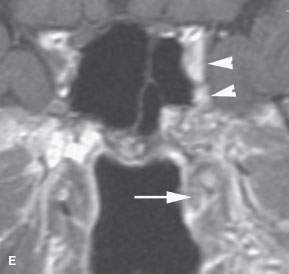
FIGURE 188.1. A patient presenting with serous otitis on the left side. Examination of the nasopharynx was normal. Magnetic resonance imaging was done. The non–contrast-enhanced T1-weighted (T1W) image in (A) shows an infiltrating mass on the left (arrow) compared to the normal anatomy on the right (arrowhead). In (B) and (C), the contrast-enhanced T1W images show subtle thickening of the torus tubarius and abnormal enhancement along the eustachian tube and palatal levator muscle on the left side (arrows) compared to the right. The T2-weighted image in (D) confirms the abnormal signal along the eustachian tube (arrow) compared to the normal anatomy on the left side. The contrast-enhanced T1W image in (E) shows subtle abnormal enhancement along the eustachian tube and deeper structures (arrows) as well as spread of tumor along trigeminal nerve divisions to involve the cavernous sinus region on the left side (arrowheads). Upon careful questioning, the patient also had a history of progressive left facial pain in addition to the serous otitis.
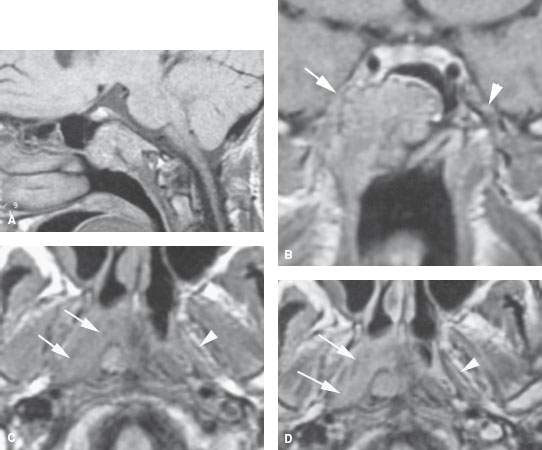
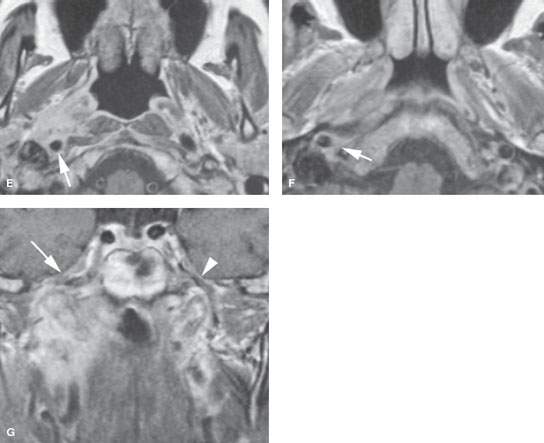
FIGURE 188.2. Two patients presenting with right facial pain and right serous otitis. Endoscopic examination of the nasopharynx showed only a submucosal bulge on the right. Both had adenoid cystic carcinoma arising from the submucosal minor salivary glands. A, B: Patient 1 had magnetic resonance imaging (MRI) showing that the adenoid cystic carcinoma infiltrates the clivus, as seen on the non–contrast-enhanced T1-weighted (T1W) image in the sagittal plane in (A). In (B), the tumor can be seen widely infiltrating the central skull base and extending along the third division of the trigeminal nerve into the paracavernous region on the right side, likely along the third division of the trigeminal nerve (arrow), compared to the normal on the left (arrowhead). C–G: Patient 2 also had an MRI study. In (C), the non–contrast-enhanced T1W image shows a mass infiltrating along the eustachian tube and obliterating the pharyngeal musculature compared to the normal side (arrowhead). In (D), the contrast-enhanced T1W image shows the mass to be enhancing (arrows) when compared to the normal noninfiltrated anatomy on the left (arrowhead). In (E), the contrast-enhanced T1W image shows the tumor in a fairly aggressive pattern spreading posteriorly to encase the internal carotid artery (arrow). That encasement continues to just below the vertical segment of the carotid canal (arrow in F). The T1W coronal image in (G) shows the tumor invading the central skull base near the foramen ovale with continued spread to encase the carotid artery within the carotid canal (arrow) as well as involvement of the trigeminal nerve ganglion region (arrow) compared to the normal left side (arrowhead).
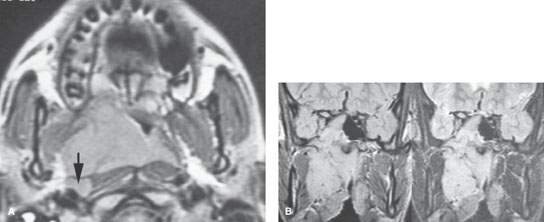
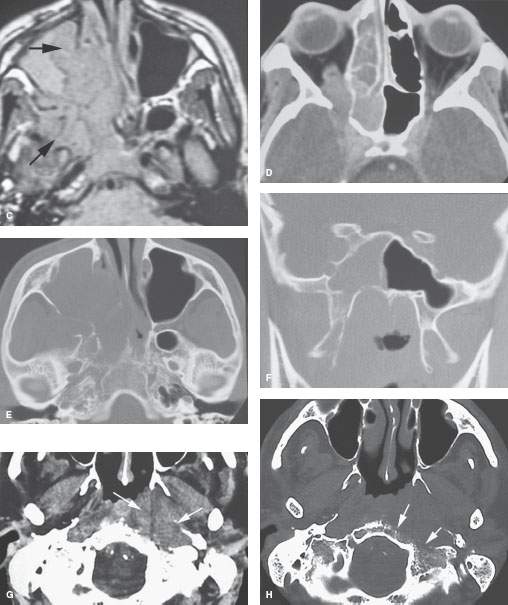
FIGURE 188.3. Two patients with submucosal-origin nasopharyngeal cancer. A–F: A child presenting with nasal stuffiness, trismus, and slight proptosis on the right in addition to serous otitis. In (A), the contrast-enhanced T1-weighted image shows the infiltrating mass within the nasopharynx, which was entirely submucosal on physical examination. There is a likely positive retropharyngeal node (arrow). In (B), the density and T2 weighted (T2W) pair show the extensive tumor deep to the mucosa of the nasopharynx involving the masticator space and spreading transcranially into the medial aspect of the cavernous sinus as well as involving the sphenoid sinus. The T2-weighted (T2W) image in (C) shows the mass extending well anterior into the nasal cavity and destroying the medial wall of the maxillary sinus. The interface between the tumor and the obstructive sinus contents is visible (arrow). In (D), the computed tomography (CT) study shows the tumor to be invading the superior orbital fissure, producing slight proptosis. Skull base erosion is shown in (E) and (F). G, H: Patient 2 presenting with serous otitis media on the left and a submucosal bulge in the nasopharynx as seen on physical examination. The CT study shows an infiltrating mass (arrows in G) growing deep to the nasopharyngeal mucosa and in the retrostyloid parapharyngeal space (arrows) with bone erosion along the cortical margin of the posterior skull base (arrows) seen in (H). This was subsequently proven to be an extramedullary plasmacytoma.
IMAGING APPROACH
Techniques and Relevant Aspects
For CT acquisitions, section thickness should be 0.5 to 1.0 mm through the area of main interest so that coronal reconstructions can be done to study areas suspicious for early bone erosion. Intravenous contrast is always used except when a CT is being done solely to look for skull base erosion. Specific protocol parameters are presented in Appendix A.
Magnetic resonance (MR) is normally done in three planes. A three-dimensional Fourier transform postcontrast image should be added to standard protocols in patients with known cancer. This usually aids treatment planning and allows for detection of subtle cavernous sinus involvement.
Fat-suppressed imaging can lose critical information at the skull base due to field distortion susceptibility artifacts (Chapters 1 and 3). Fat suppression should not be the sole T1-weighted postcontrast acquisition. The images without fat suppression are very sensitive to marrow space infiltration and should be done at least in the coronal plane. Specific MR protocol parameters are presented in Appendix B.
The neck is always included when CT is performed. It is considered optional for MR since it adds considerable time and expense to the examination, almost doubling the cost in some institutions. The yield of significant information from MR study of the neck compared with the costs may not be cost justified except under the limited circumstances described later.
Imaging for distant metastases includes a chest roentgenogram. A chest CT to include the liver and a bone scan are obtained only if the patient has a clinical picture suggesting the presence of distant metastases. The role of FDG-PET is not yet clearly established. It should be used with discernment with regard to its likelihood of contribution to medical decision making in any individual case.
Pros and Cons
General Approach
Imaging is required for staging and treatment planning in all nasopharyngeal malignancies. When nasopharyngeal malignancy is suspected but not confirmed, CT and/or MRI become an essential part of the diagnostic process, and preferably one of these studies is done before biopsy (Figs. 188.1, 188.2, and 188.4–188.6).
MR is preferred as the initial examination for most diseases involving the nasopharynx, parapharyngeal space, and infratemporal fossa. CT is also used in many cases. MR and CT may both be used at least initially for evaluating possibly primary skull base pathology. The precise ordering of studies depends on the suspected pathologic process, the need to assess bone detail, the likelihood of perineural and perivascular spread, and intracranial disease. Bone detail is the main reason for adding a CT to a primary MR examination.
The relative role of imaging studies for the diagnosis and management of juvenile nasopharyngeal angiofibroma and a paraganglioma of the parapharyngeal space is discussed in conjunction with those specific tumor types. (Chapters 33, 123, 144, and 189).
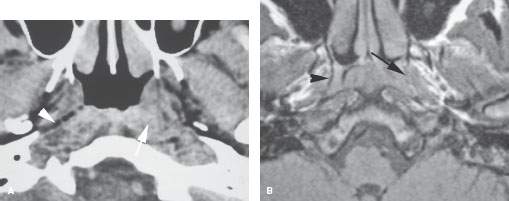

FIGURE 188.4. A patient presenting with a level 2 lymph node. Examination of the nasopharynx was negative. The computed tomography study in (A) shows an infiltrating mass around the upper fossa of Rosenmüller on the left side obliterating deep tissue planes (arrow) compared to the normal deep tissue planes on the right (arrowhead). In (B), the non–contrast-enhanced T1-weighted (T1W) image also shows subtle infiltrating tumor on the left obliterating the pharyngobasilar fascia (arrow) on that side compared to the normal on the right (arrowhead). C: A contrast-enhanced T1W coronal image shows a submucosal infiltrating mass (arrow) on the left side with subtle enhancement infiltrating the pharyngeal musculature (arrowhead). This was subsequently shown to be a clinically occult carcinoma of the nasopharynx.
Specific Indications for Study
Known Cancer: For Extent of the Primary Including Perineural and Perivascular Spread
In histologically confirmed nasopharyngeal cancer, MRI is preferred as the primary imaging study. Such imaging is very useful for showing the relationship of cancer to the skull base, cavernous sinus, brain, and orbits (Fig. 188.7) as well as the extent of regional adenopathy (Fig. 188.8). MR contrast resolution detects subtle spread in deep tissue planes, including the prestyloid parapharyngeal space (PSPS), RSPS, and masticator spaces (Figs. 188.9 and 188.10). Unanticipated posterior and inferior spread in the RSPS in particular can alter radiotherapy (RT) planning. MRI can also help to differentiate obstructive and reactive changes from tumoral pathology in the nasal cavity sinuses and temporal bone (Fig. 188.11).
MRI is the preferred study for showing perineural spread that most typically will be along V2 or V3 and perivascular spread that might grow along the carotid artery and canal into the cavernous sinus (Figs. 188.1A–E, 188.2, 188.5E–G, and 188.9). Spread along cranial nerves IX through XII and the sympathetics in the RSPS can also be assessed (Fig. 188.11). The rare cases of facial nerve involvement can be evaluated for full proximal and distal spread along the nerve.
CT may be necessary to detect or exclude early skull base erosion (Figs. 188.12 and 188.13), to evaluate advanced neck disease (Figs. 188.8–188.10), or in patients unable to have an MR study.
Staging Regional Nodes
Clinical nodal staging assisted by imaging is less critical for primary nasopharyngeal carcinoma than for carcinomas arising at other head and neck, skin, glandular, and mucosal sites, because the neck nodes are involved in at least 70% of cases and bilaterally 50% of the time. The neck almost always responds completely to radiation or chemoradiation protocols regardless of neck stage. The radiation dose to cervical nodes positive on physical examination or CT is 70 Gy, while those only positive on imaging studies (subclinical disease) will be 50 Gy; thus CT is done as well as MRI on patients with nasopharyngeal cancer to estimate whether the extent of neck disease present on imaging justifies such dose escalation in a neck that is negative on physical examination. Also, extensive node disease may on occasion lead to a planned postradiation neck dissection (Fig. 188.10D)
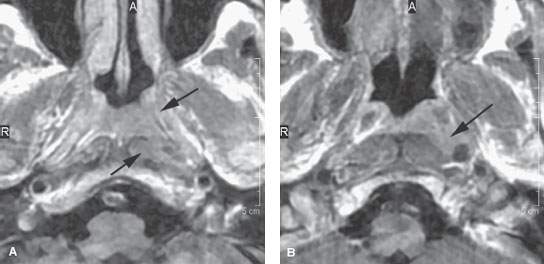
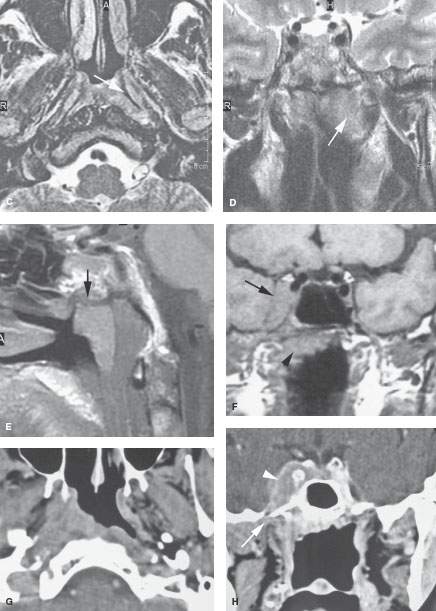
FIGURE 188.5. Two patients with early nasopharyngeal carcinoma. A–E: Patient 1 presenting with cervical adenopathy and left serous otitis. Examination of the nasopharynx showed no definite abnormality other than what was interpreted as a normal to somewhat prominent adenoidal pad. Biopsies were negative. Contrast-enhanced T1-weighted (T1W) images in (A) and (B) show an infiltrating mass on the left side compared to the right. The T2-weighted (T2W) image in (C) shows abnormal tumor on both sides of the pharyngobasilar fascia (arrow). The T2W coronal image in (D) shows the primarily submucosal mass (arrow) extending to the central skull base, which on the T1W sagittal image in (E) is either producing reactive sclerosis along the central skull base or shows evidence of early invasion (arrow). Computed tomography (CT) subsequently confirmed early skull base invasion, and CT-guided biopsy showed squamous cell carcinoma. F–H: Patient 2 presenting with a right-sided cavernous sinus syndrome. Magnetic resonance imaging seen in (F) was initially interpreted in another institution as showing a meningioma of the right cavernous sinus (arrow). The primary carcinoma along the roof of the nasopharynx went unnoticed (arrowhead). CT study done subsequently shows the infiltrating mass in the right side of the nasopharynx (G), which was entirely submucosal on physical examination. The coronal CT image in (H) following contrast injection shows the mass infiltrating the deep soft tissues to just below the foramen ovale (arrow), which is the likely conduit of the extensive spread within the right cavernous sinus.
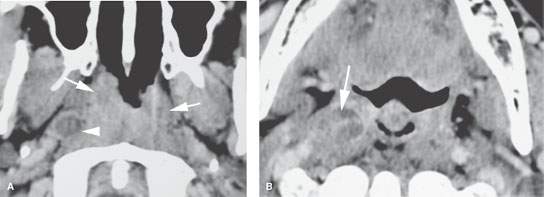
FIGURE 188.6. A patient presenting with cervical adenopathy and right serous otitis. The contrast-enhanced computed tomography in (A) shows a circumferential mass in the nasopharynx with invasion of deep soft tissue planes (arrow). There is an obviously positive bright retropharyngeal lymph node (arrowhead) seen again in (B) (arrow). This is an example of a relatively superficially spreading nasopharyngeal squamous cell carcinoma. The lesion was easily identifiable on physical examination.
Suspected Recurrence of Nasopharyngeal Cancer
MR is preferred over CT for patients with possible recurrent nasopharyngeal cancer. This is discussed more completely subsequently.
Suspected Nasopharyngeal Cancer or Nasopharyngeal Mass of Uncertain Etiology
Patients with cervical lymph node metastases from a mucosally unapparent primary, persistent unilateral serous otitis media despite adequate management, or those with cranial nerve deficits possibly attributable to nasopharyngeal cancer should have a definitive imaging study of the nasopharynx (Fig. 188.4).
Submucosal Nasopharyngeal and/or Parapharyngeal Mass
Patients presenting with submucosal nasopharyngeal (and/or oropharyngeal) “bulges” of uncertain etiology should always be studied before biopsy. These masses producing such “bulges” are often of parapharyngeal space origin rather than nasopharyngeal mucosal or submucosal origin. Imaging will often suggest a specific etiology for the mass, but when the diagnosis is not certain or near certain, imaging will always suggest the next best course of action. On occasion, it helps to avoid potential disaster such as biopsy of an abnormal vessel (e.g., a tortuous or aneurysmal carotid artery) or a vascular mass such as a paraganglioma or venolymphatic malformation (Fig. 189.1). Imaging obviates a potentially compromising transmucosal, incisional biopsy of a parapharyngeal benign mixed tumor (Figs. 188.1–188.3). Following the initial diagnostic MR or CT study, a patient with such a submucosal mass may be triaged to standard transmucosal biopsy, imaging-directed percutaneous biopsy, angiography, observation, or no action such as when the mass turns out to simply be a tortuous carotid or some odd benign condition of bone. The use of imaging in the diagnosis and further management of juvenile nasopharyngeal angiofibroma is discussed in conjunction with that particular tumor (Chapter 189).
Controversies
The standard or “routine” use of FDG-PET in head and neck cancer remains not yet clearly evidenced based, although its use in practice is common. FDG-PET should only be used with discernment, considering its likelihood of contributing to truly improve medical decision making and outcome in any individual case (Fig. 188.9).
SPECIFIC DISEASE/CONDITION
Nasopharyngeal Carcinoma
Etiology
The risk of nasopharyngeal squamous cell carcinoma (SCCA) in Chinese American males is much higher than that of any other ethnic group. Other Asian populations do not exhibit such a risk. The contributing factors are uncertain. A relationship to nitrosamines, genetic susceptibility, and Epstein-Barr virus (EBV) has been suggested.
Adenoid cystic carcinoma, adenocarcinoma, and sinonasal undifferentiated cancer primarily involving the nasopharynx occurs sporadically.
Prevalence and Epidemiology
The incidence of nasopharyngeal carcinoma is much higher in China than the United States, and U.S. immigrant Chinese have a greater risk of developing a malignancy of the nasopharynx than those born in the United States. There is a significant predominance of the disease in males, and the age distribution is much younger than for cancer of other head and neck sites. The disease has been seen in young children.
Screening programs related to EBV have been employed in areas where there is a high incidence of this malignancy. Positive screenings may then be referred for nasopharyngeal examination. More recently, MRI has been used to help screen similar at-risk Asian populations.
The World Health Organization (WHO) has classified nasopharyngeal squamous cell carcinomas (SCCa) as WHO-1, keratinizing; WHO-2, nonkeratinizing, and WHO-3, undifferentiated. Lymphoepithelioma is included in the WHO-3 category.
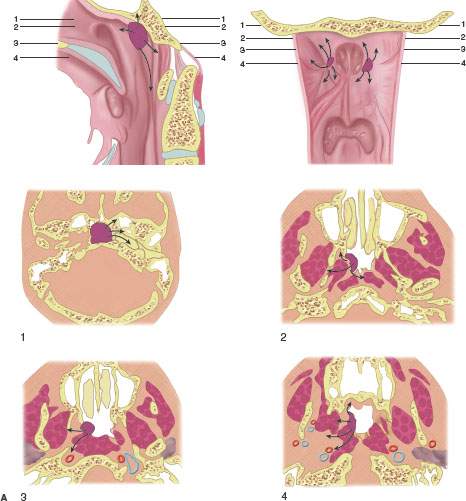
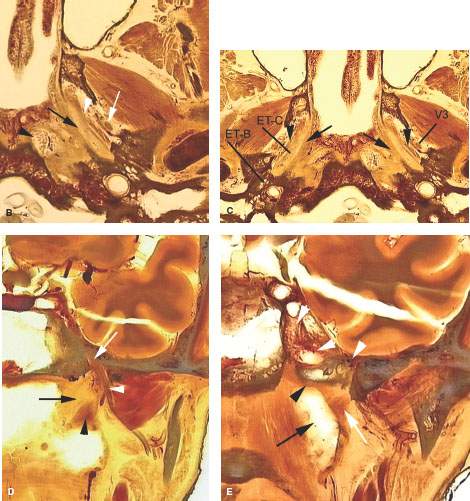
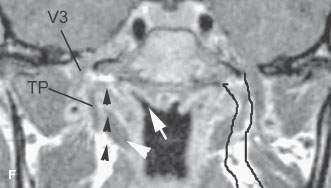
FIGURE 188.7. A: Spread patterns of nasopharyngeal carcinoma. B: Anatomic section showing the relationships between the pharyngobasilar fascia and eustachian tube (black arrow) and the fascia covering the pharyngeal musculature (white arrowhead) and the mandibular division of the trigeminal nerve, which lies just outside the fascia around the pharyngeal musculature (white arrow). The proximity of the fossa of Rosenmüller near the skull base (black arrowhead) to the area of the petroclival fissure is illustrated as well. C: Anatomic diagram showing the overall relationship of the eustachian tube to the skull base, nasopharynx, and temporal bone. The eustachian tube is intimately related to and travels through a defect between the skull base and the pharyngobasilar fascia (black arrows). The muscles of the pharyngeal wall (black arrowheads) and their fascia separate the nasopharynx and parapharyngeal space from the masticator space, which contains the third division of the trigeminal nerve (V3). The bony and cartilage parts of the eustachian tube (ETC-ETB) are shown on the right. (NOTE: From these relationships, it can be understood how the muscles, eustachian tube, or pharyngobasilar fascia could all be conduits directing the spread of cancer to the skull base along the clivus, inferior petrous apex, or central skull base.) D: Coronal anatomic section showing the relationship of the eustachian tube (black arrow) to the levator muscle of the palate and in turn the relationship of those two structures to the third division of the trigeminal nerve (white arrowhead) and its entry into the foramen ovale (white arrow). Also note the proximity of the mucosa along the roof of the nasopharynx to the base of the sphenoid bone. E: Coronal anatomic section somewhat more posterior to that in Figure 188.7D. This section shows the proximity of the uppermost aspect of the fossa of Rosenmüller (black arrow) to the skull base in the region of the petroclival junction. It also shows the levator muscle of the palate as it approaches its attachment to the skull base (white arrow). (NOTE: The proximity of these structures to the carotid canal and cavernous sinus and carotid artery (white arrowheads) explains the close anatomic relationships that allow nasopharyngeal carcinoma to spread to the skull base and intracranially along one or more of the potential conduits.) F: Contrast-enhanced T1-weighted coronal magnetic resonance to correlate with the anatomic sections seen in Figure 188.7D,F. The tensor muscle of the palate (TP) marks the boundary between the parapharyngeal space and masticator space. The third division of the trigeminal nerve (V3) lies outside of that boundary within the masticator space. Tumor spreading within the parapharyngeal space can spread along the levator muscle of the palate (white arrowhead) or within the parapharyngeal space and/or along pharyngeal musculature (black arrowheads) to gain access to the skull base and intracranial structures. (NOTE: The lymphoid tissue lining the fossa of Rosenmüller (white arrow) lies in very close proximity to the petroclival fissure and base of the sphenoid bone. On the left side, the parapharyngeal space is outlined by black lines, emphasizing its role in potentially directing the spread of tumor to the skull base and intracranially.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








