Pelvis
Case 4.1 Chordoma
CLINICAL HISTORY A 50-year-old man with back pain for several months.
FINDINGS
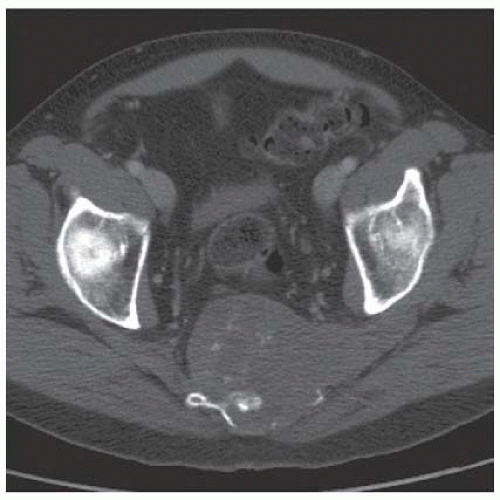
Axial computed tomography (CT) shows a midline mass causing lytic destruction of inferior sacrum with presacral soft tissue extension. There are small foci of calcifications within the mass.
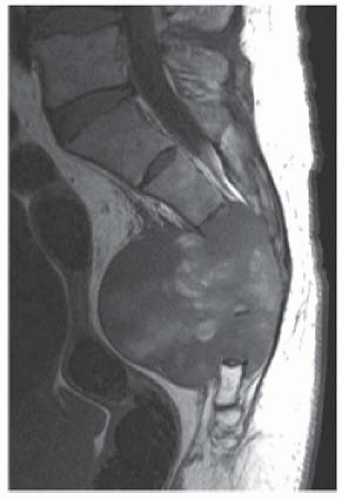
Sagittal T1-weighted magnetic resonance image (MRI) demonstrates a heterogeneously low signal intensity mass replacing the distal sacrum and extending anteriorly into the pelvis.
Sagittal postcontrast T1-weighted fat-saturated MRI shows diffuse enhancement within the mass.
DIFFERENTIAL DIAGNOSIS Chordoma, metastasis, plasmacytoma, lymphoma, sarcoma.
DIAGNOSIS Chordoma.
DISCUSSION The diagnosis is suggested by the characteristic location in the midline of the sacrococcygeal region, with asymmetric expansion from the bone into the anterior soft tissues. The radiologic features typical of chordoma in this location are irregular osteolysis and expansion with an associated anterior soft tissue mass. Fifty percent to seventy percent of cases may show amorphous calcification, usually in the periphery of the tumor; some lesions present with sclerosis instead of osteolysis. On T2-weighted MRI, the lesions are typically as bright as hydrated intervertebral discs [1,2]. Chordoma is a locally aggressive lesion of notochordal origin [3]. Chordomas are most common in the sacrococcygeal region (50% to 60% of lesions), in men (2:1 predilection), and between the ages of 40 and 70. Sphenooccipital lesions account for almost all of the remainder of lesions (25% to 40%). Sacrococcygeal lesions typically present with pain and perineal numbness. The lesions usually arise from the vertebral body, but they can extend into the posterior elements.
Case 4.2 Radiation Change
CLINICAL HISTORY A 50-year-old man after treatment for prostate carcinoma.
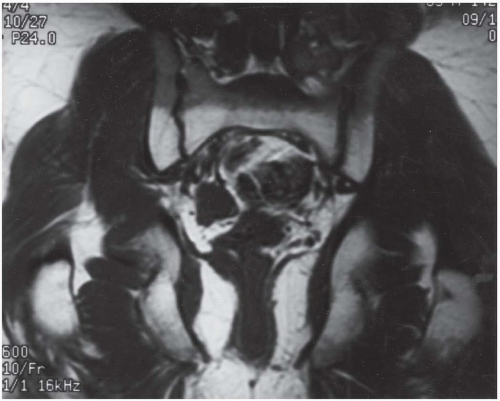
FINDINGS Coronal T1-weighted MRI of the pelvis demonstrates a band of increased signal in the inferior sacrum, with a well-defined horizontal border.
DIFFERENTIAL DIAGNOSIS Radiation change, insufficiency fracture, imaging artifact.
DIAGNOSIS Radiation change.
DISCUSSION Therapeutic irradiation has direct effects on the cellular components of bone as well as indirect effects that result from vascular injury. Deleterious effects on bone include growth. MRI is commonly used to study the spine or pelvis after therapeutic irradiation. On T1-weighted MRI, there is an increased signal in the involved bone due to replacement of the hematopoietic marrow with fat. This alteration can be seen 3 months after initiation of therapy, and may remain indefinitely [5,6]. Radiation can also give rise to marrow fibrosis. Fibrosis should have low signal intensity on both T1-weighted and T2-weighted MRI, whereas tumor typically has increased signal on T2-weighted MRI due to the increased water content. Other effects of radiation therapy include avascular necrosis, insufficiency fractures, and radiation-induced neoplasms. In the growing skeleton, deleterious effects of radiation include inhibition of bone growth, slipped capital epiphyses, and scoliosis.
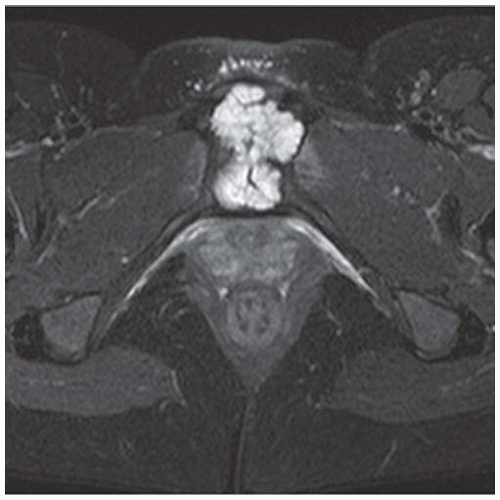
Case 4.3 Ewing’s Sarcoma
CLINICAL HISTORY A 24-year-old woman with low back pain for several months.
FINDINGS
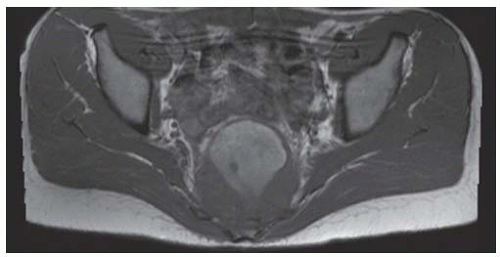
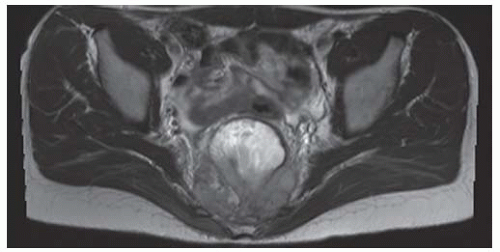
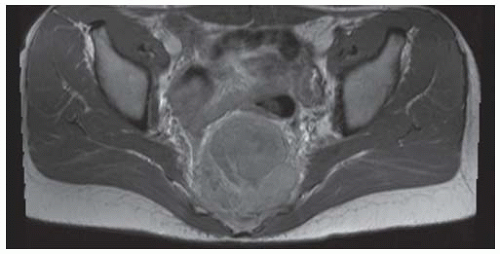
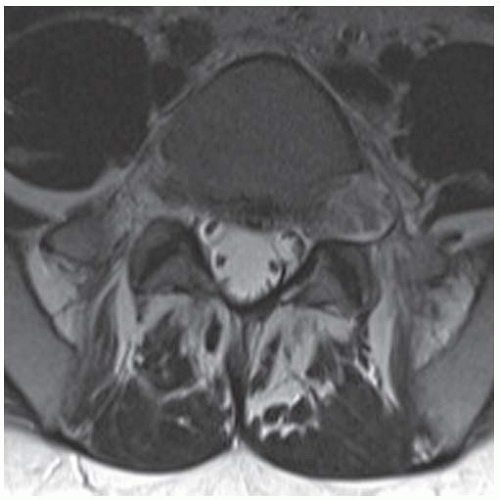
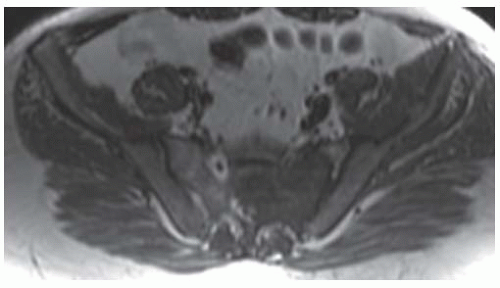
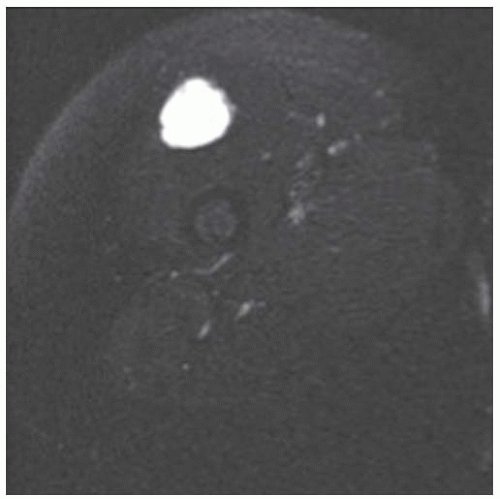
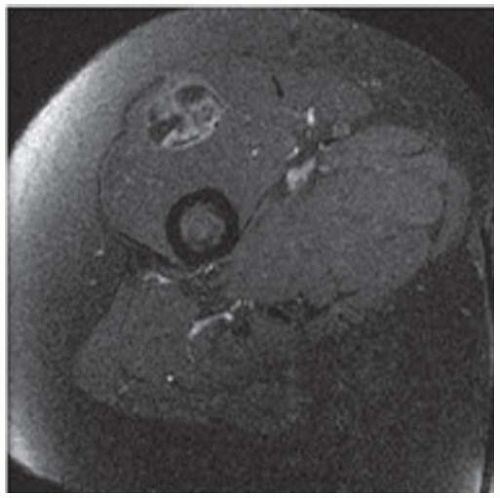
Axial T1-weighted MRI shows a round mass in the pelvis arising from the lower sacrum in the midline and extending anteriorly into the pelvic cavity. The mass has a large central region of heterogeneous high signal with surrounding rim of low-to-intermediate signal.
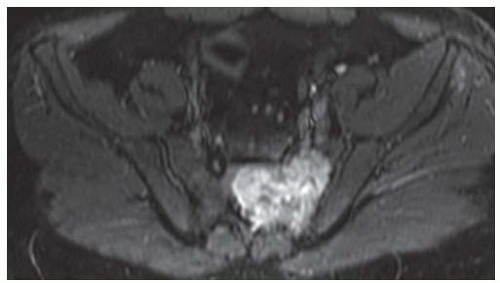
Axial T2-weighted fat-suppressed MRI at the same level shows heterogeneous high signal in the central region of the mass with posterior and surrounding regions of low-to-intermediate signal.
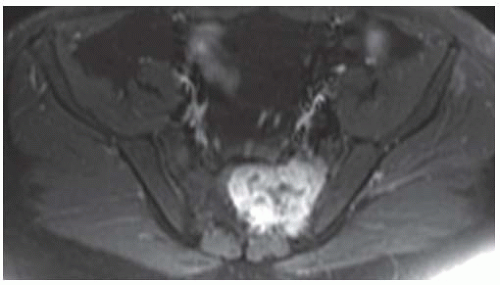
Axial postcontrast T1-weighted fat-suppressed MRI shows peripheral enhancement around the mass.
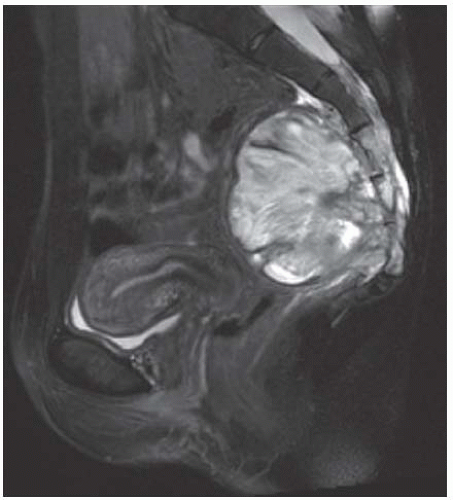
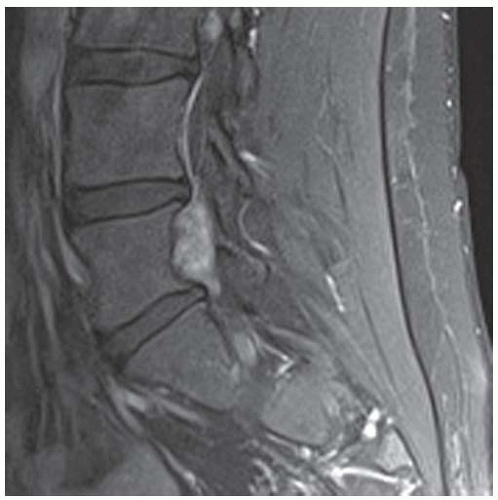
Sagittal T2-weighted fat-suppressed MRI shows the mass protruding into the presacral soft tissues, displacing the visceral structures. The lower sacrum and upper coccyx are enveloped by the lesion.
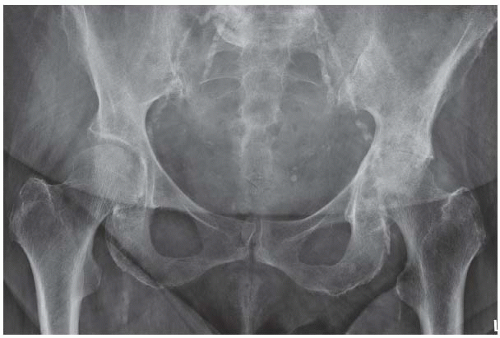
Anteroposterior (AP) radiograph of the pelvis shows bony destruction of the lower sacrum, largely obscured by bowel contents.
DIFFERENTIAL DIAGNOSIS Giant cell tumor, aneurysmal bone cyst, lymphoma, sarcoma, chordoma, metastasis, plasmacytoma/myeloma.
DIAGNOSIS Ewing’s sarcoma.
DISCUSSION An expansile, destructive mass arising in the sacrococcygeal region of a young adult raises a somewhat different differential diagnosis than the same in an older adult. Giant cell tumor of bone and aneurysmal bone cyst are possible diagnoses in young adults that would be much less likely after age 50. Chordoma, metastasis, and plasmacytoma/myeloma are unlikely possibilities in a young adult, but these lesions are more likely after age 50. The aggressive imaging features of the case here are not specific for Ewing’s sarcoma, but do indicate the need for a tissue diagnosis. Ewing’s sarcoma may occur in virtually any bone, with about 6% in the sacrum and 4% in other regions of the spine [4]. Of primary malignant bone tumors found in the sacrum in the Mayo Clinic series, 45% were chordoma, 12% were myeloma, 11% were lymphoma, 9% were osteosarcoma, 8% were Ewing’s sarcoma, and 14% were others [4].
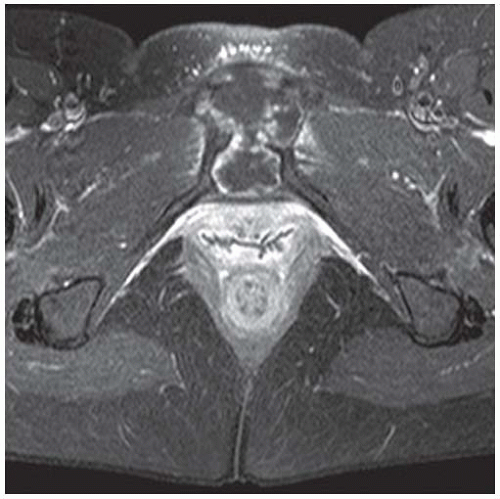
Case 4.4 Radiation Changes with Insufficiency Fracture
CLINICAL HISTORY An 81-year-old woman with left hip pain after left pelvic radiation therapy for non-Hodgkin’s lymphoma 2 years earlier.
FINDINGS
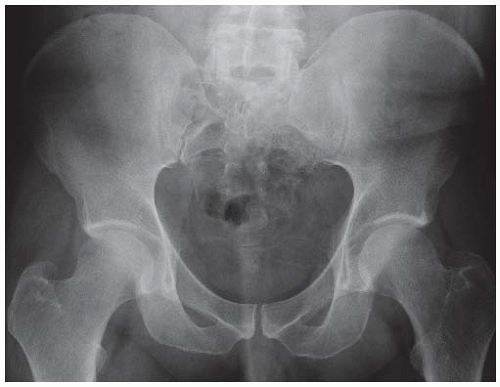
AP radiograph shows increased radiodensity over the left hemipelvis and axial joint space narrowing of the left hip.
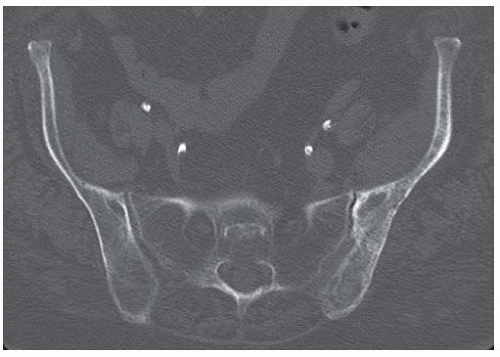
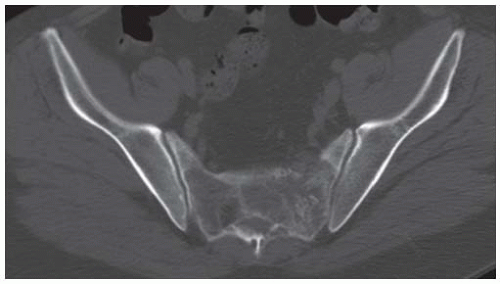
Axial CT scan through the iliac wings shows irregularly marginated marrow calcifications on the left.
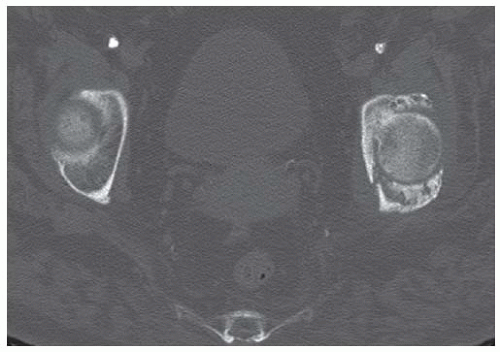
Axial CT scan through the hips shows sclerosis of the left acetabulum and a posterior acetabular wall detached subchondral fracture fragment.
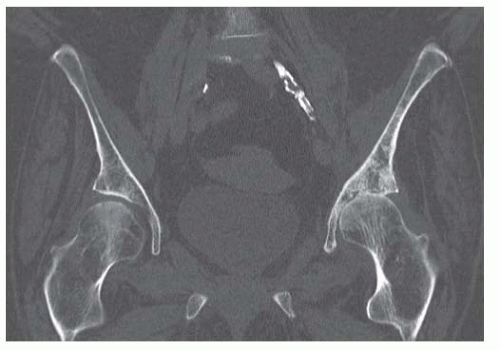
Coronal reformatted CT scan through the hips shows diffuse marrow calcification within the left iliac wing and diffuse loss of cartilage at the left hip. There are no osteophytes. The right hip is normal.
Coronal reformatted CT through the posterior acetabula shows a densely calcified sequestrum on the left.
DIFFERENTIAL DIAGNOSIS Radiation changes, insufficiency fracture, Paget disease
DIAGNOSIS Radiation changes with insufficiency fracture.
DISCUSSION The irregular marrow sclerosis in this case raises the possibility of Paget disease, but the cortex is not thickened and the bone is not enlarged. The subchondral fracture with detached but nondisplaced fragment is characteristic of fractures that occur in osteonecrosis. As bone remodeling occurs around a region of osteonecrosis, trabeculae are removed and then replaced by creeping substitution, leaving the site vulnerable to fracture. In adults, unintended effects of radiation therapy on bone include radiation osteitis and insufficiency fractures. In one study of pelvic bone complications following radiation therapy for uterine cancer, the authors found that the prevalence of insufficiency fractures, as detected by MRI, increased with time after radiation, from approximately 15% after 1 year to 45% after 5 years [6]. The majority of fractures were located in the sacrum, and most of these involved the sacral ala. Radiation may also have a toxic effect on chondrocytes.
Case 4.5 Neurofibroma
CLINICAL HISTORY A 24-year-old man with posterior left thigh pain.
FINDINGS (A, B) Axial T2-weighted magnetic resonance imaging (MRI) shows a large exiting left L5 nerve root with bony remodeling of the left L5-S1 neural foramen. Pre (C) and post (D) contrast sagittal T1 fat-saturated MRI images on left parasagittal plane show large enhancing mass in the L5-S1 neural foramen. In addition, there is another smaller enhancing focus seen in the L3-L4 foramen.
DIFFERENTIAL DIAGNOSIS Neurofibroma, schwannoma, metastasis.
DIAGNOSIS Neurofibroma.
DISCUSSION The particular location and morphology of this lesion suggests the diagnosis of a nerve sheath tumor. The remodeling of the bone around the enlarging tumor indicates very slow growth. Neurofibromas are benign fibroblastic neoplasms of peripheral nerves, whose consistency and histologic appearance vary from myxoid to fibrous according to the differentiation of the neoplastic elements [7]. The bulk of the tumor volume consists of intercellular collagen fibrils in an unorganized myxoid matrix. Their imaging characteristics depend on the relative balance of fibrous and myxoid material. On MRI, neurofibromas tend to be isointense to muscle on T1-weighted images and hyperintense on T2-weighted images, and can be inhomogeneous [8]. Neurofibromas in the extremities are a feature of neurofibromatosis type I.
Case 4.6 Lymphoma (Richter’s Syndrome)
CLINICAL HISTORY A 75-year-old man with back pain and history of chronic lymphocytic leukemia (CLL).
FINDINGS
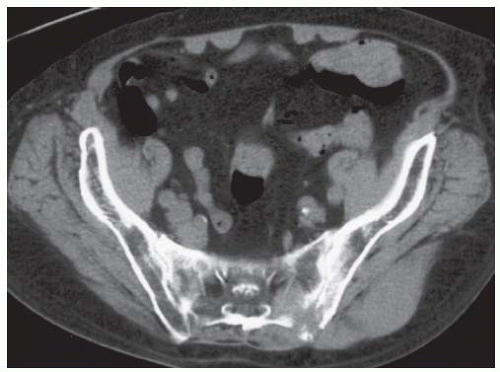
Axial CT scan shows lytic bone destruction of the sacrum and ilium. The soft tissue masses have no calcification, and there is no reactive bone formation.
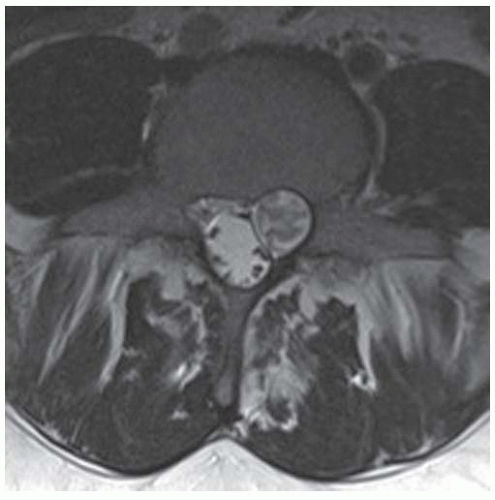
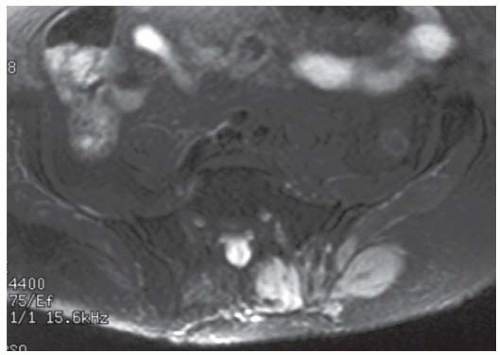
Axial T2-weighted MRI with fat saturation at the level of S1 shows masses in the paraspinal musculature and superficial to the gluteus maximus. The lesions have homogeneous high signal, and there is contiguous involvement of the ilium and sacrum.
DIFFERENTIAL DIAGNOSIS Lymphoma, leukemia, metastases, infection.
DIAGNOSIS Lymphoma (Richter’s syndrome).
DISCUSSION The images show soft tissue masses involving the paraspinal and gluteus musculature, an appearance that raises the differential diagnosis of lymphoma, leukemia, metastases, and infection. The presence of bone destruction eliminates hematoma as a possibility, and the lack of a single dominant mass lesion is very uncharacteristic of a connective tissue sarcoma.
The specific diagnosis depends on the clinical situation and must be confirmed by biopsy. Secondary malignancies develop in approximately 5% of patients with CLL, the most common of which is non-Hodgkin’s lymphoma, followed by Hodgkin’s lymphoma and multiple myeloma [9,10]. The development of non-Hodgkin’s lymphoma in CLL is called Richter’s syndrome. These lymphomas are high-grade malignancies of B-cell origin, associated with abrupt onset of constitutional symptoms, rapidly progressive lymphadenopathy, and rapid clinical deterioration to a fatal outcome. They are resistant to current therapies and may develop while the CLL is in remission. In approximately 60% of cases, the lymphoma evolves from the original leukemic cell clone, but in the remainder it has a different clonal evolution.
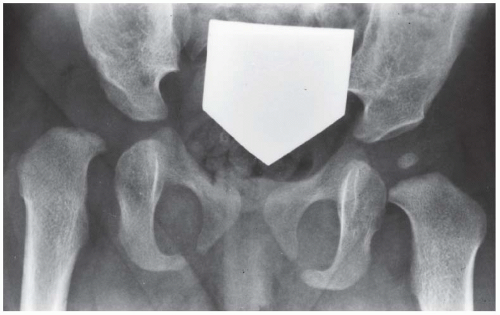
Case 4.7 Developmental Dysplasia of the Hip (DDH)
CLINICAL HISTORY Newborn baby girl.
FINDINGS AP pelvis radiograph shows a dysplastic, dislocated right hip. The capital femoral ossification is not yet present, unlike the contralateral side. The acetabular angle is steep and shallow.
DIFFERENTIAL DIAGNOSIS None.
DIAGNOSIS Developmental dysplasia of the hip (DDH).
DISCUSSION In DDH, an abnormally lax joint capsule allows the femoral head to fall out of the acetabulum shortly before or after birth, leading to congenital or postnatal deformation of an initially normal structure. The causes are multifactorial and appear to be related to the effects of restricted intrauterine movement and maternal hormones. Restricted fetal movement during the third trimester may result from conditions such as breech presentation or oligohydramnios, and may partially or completely dislocate the hip. Maternal hormones (such as estrogen) that relax the pelvic ligaments to facilitate childbirth also increase the laxity of the fetal ligaments and joint capsules. This effect is particularly evident in female fetuses and may account for the 6:1 female preponderance of DDH. DDH also has a familial tendency, which is possibly related to an inherited abnormality in estrogen metabolism. Although sonography is the imaging examination of choice in the neonate and has the advantage of immediate correlation with physical examination, results vary with technical and interpretive factors [16]. In older infants, the AP radiograph becomes more reliable as the capital femoral epiphysis becomes ossified.
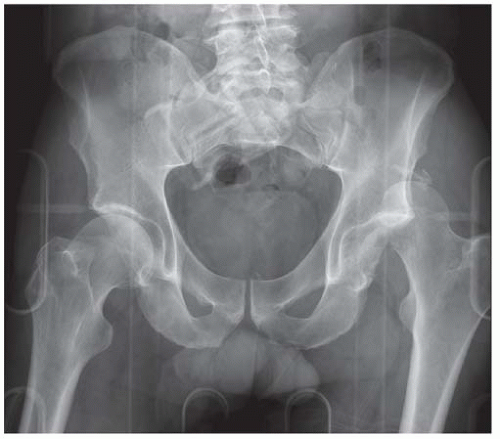
Each hip can be divided into quadrants by drawing a horizontal baseline through the triradiate cartilages (Hilgenreiner’s horizontal line) and a perpendicular line through the most lateral ossified margin of the roof of the acetabulum (Perkins’ line). The normal location of the femoral head is in the lower inner quadrant (down and in). A dislocated femoral head will be in the upper outer quadrant (up and out), and a subluxated femoral head will be in the lower outer quadrant (down and out). The angle between the acetabulum and the horizontal baseline should be less than 40 degrees in a newborn, 33 degrees in a 6-month-old, and 30 degrees in a 1-year-old. In the normal hip, a smooth curve can be drawn along the inferior margin of the superior pubic ramus and the medial femoral cortex (Shenton’s line). Other findings include a shallow acetabulum, development of a false acetabulum, and delayed ossification of the involved capital femoral epiphysis. CT scanning may be necessary to confirm anatomic relocation of the hips once the patient has been placed in a cast [17]. MRI may be used to evaluate problematic cases.
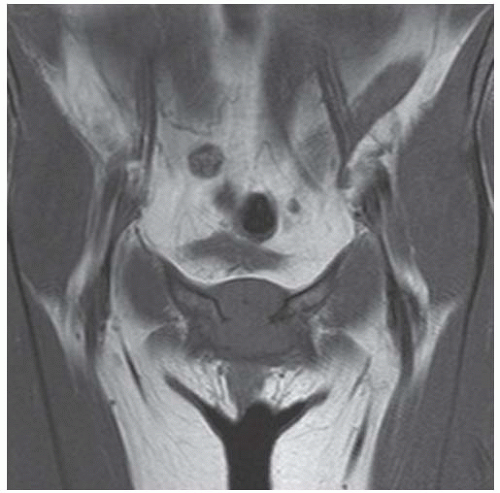
Case 4.8 Chondrosarcoma
CLINICAL HISTORY A 36-year-old female with pubic pain.
FINDINGS
A. AP view of pelvis shows a multiloculated lytic lesion causing destruction about the symphysis pubis. There is no periosteal reaction in the adjacent pubic rami.
B. Coronal T1-weighted MRI shows lobulated mass centered at the symphysis and isointense to muscle.
C, D. This mass shows high signal in axial fat-saturated T2-weighted sequence (C) and heterogeneous enhancement with gadolinium on T1-weighted fatsaturated sequence (D).
DIFFERENTIAL DIAGNOSIS Chondrosarcoma, metastasis, plasmacytoma, infection
DIAGNOSIS Chondrosarcoma
DISCUSSION Chondrosarcomas are malignant, cartilagecontaining tumors that arise de novo or from preexisting cartilage-containing lesions such as osteochondromas. In the Mayo Clinic series, approximately 24% of chondrosarcomas were found in the pelvis, and of those, about 24% were found at the symphysis; it is unusual to find chondrosarcoma distal to the ankle or wrist [11]. Chondrosarcomas are the third most common primary malignant bone tumor [12]. Chondrosarcomas tend to present in patients between the ages of 30 and 60, but the age distribution is broad. Lesions in the axial skeleton tend to present in an older age group than lesions in the peripheral skeleton. Lack of reactive bone is ominous for an aggressive, malignant process. Without the characteristic calcification and lobular structure, the diagnosis of chondrosarcoma cannot be made prospectively, and a biopsy is required. Chondrosarcomas follow a slow clinical evolution. They tend to metastasize late in the clinical course, and although the lesions are often large, patients rarely present with metastatic disease [13].
Case 4.9 Osteosarcoma
CLINICAL HISTORY A 36-year-old man with worsening pelvic pain.
FINDINGS
Axial T1-weighted MRI shows a lesion occupying the left sacrum, obliterating the left S2 neural foramen and extending across the midline.
Axial T1-weighted fat-suppressed MRI following gadolinium infusion shows intense enhancement of the lesion, with a few regions of nonenhancement.
Axial CT scan shows a destructive lesion in the left sacrum with loss of the anterior sacral cortex. Focal regions of mineralization are present within the lesion.
AP radiograph shows vague increase in density overlying the left sacrum, perhaps with speckled mineralization.
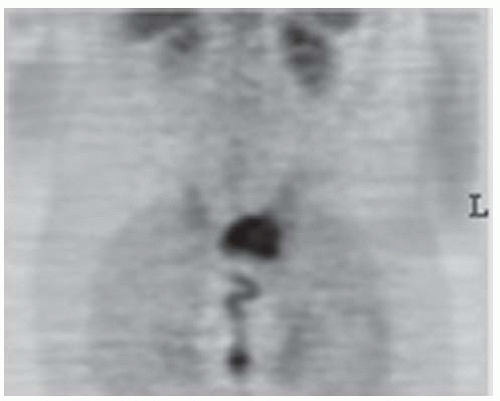
Coronal image from positron emission tomography (PET) scan shows intense activity corresponding to the lesion (maximum standard uptake value (SUVmax) was 6.4).
DIFFERENTIAL DIAGNOSIS Osteosarcoma, chondrosarcoma, lymphoma, metastasis.
DIAGNOSIS Osteosarcoma
DISCUSSION An aggressive, destructive lesion centered within bone that has internal mineralization raises the necessity for a tissue diagnosis. Of the other possibilities in the differential diagnosis, metastases tend to be multiple and smaller and frequently have a known primary site, chondrosarcomas tend to have a lobular morphology and rings-andarcs calcifications, and lymphomas tend to be infiltrative. Although the peak incidence for onset of osteosarcoma is in the second decade of life (45% of the osteosarcomas in the Mayo Clinic series), more osteosarcomas actually occur in the third or later decades (50% in the Mayo Clinic series) [14]. Only about 2% of osteosarcomas are found in the sacrum. PET and PET/CT have become important modalities in the imaging evaluation of bone lesions [15]. However, an abnormal PET scan is nonspecific and does not obviate the need for a tissue diagnosis.
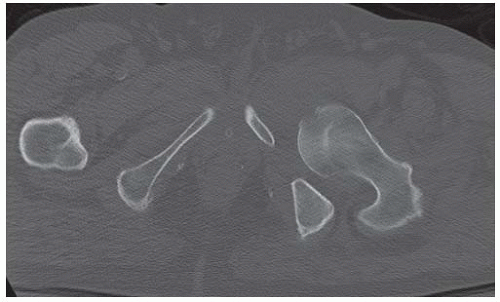
Case 4.10 Acetabular Dysplasia
CLINICAL HISTORY A 21-year-old woman with mild hip pain.
FINDINGS
Radiograph of the pelvis shows shallow, minimally dysplastic acetabula. Both femoral heads are normally formed and located.
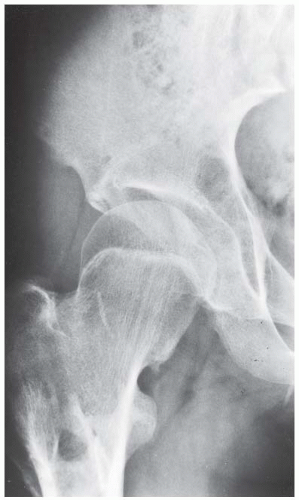
Frog-leg lateral radiograph of left hip shows the shallow acetabulum and normally shaped femoral head.
DIFFERENTIAL DIAGNOSIS None.
DIAGNOSIS Acetabular dysplasia.
DISCUSSION Acetabular dysplasia is a common cause of early osteoarthritis in adults [18]. The normal acetabulum is nearly a full hemisphere, forming the socket for the femoral head. The dysplastic acetabulum is like a shallow bowl, normally oriented but forming only a shallow socket for the femoral head. As a consequence, both the anterior and posterior articular surfaces are reduced in area, and a smaller proportion of the femoral head is covered by bone. On the radiograph, the roof of the acetabulum normally covers the top of the femoral head and inclines downward at its lateral margin. In acetabular dysplasia, the roof often fails to reach a horizontal orientation at its lateral margin, with much less incline downward. Patients are usually moderately symptomatic when they present at 30 or 40 years old, but will progress inevitably to end-stage osteoarthritis if untreated. An acetabular osteotomy provides more complete bony coverage of the femoral head and can prevent accelerated osteoarthritis [19].
Case 4.11 Femoroacetacular Impingement
CLINICAL HISTORY A 16-year-old male with recently healed left acetabular fracture with childhood history of “walking funny.”
FINDINGS
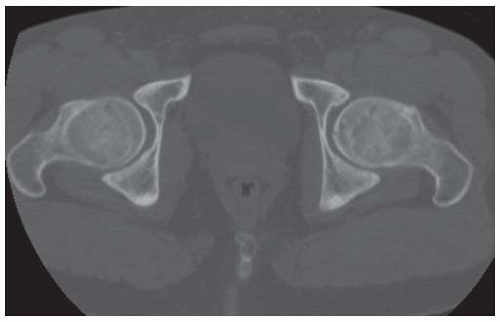
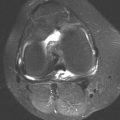
AP view of pelvis shows bilateral mild superior hip joint space narrowing, subchondral sclerosis, and subchondral cystic changes. Note is made of deformity of bilateral proximal femoral head and neck junctions with lateral extensions of epiphyseal scars, described as “pistol grip deformity.”
Axial CT image through bilateral femoral head and neck junction shows an abnormal “bump” anteriorly with associated subchondral cysts.
DIFFERENTIAL DIAGNOSIS Prior traumatic osteoarthritis, femoroacetabular impingement (FAI), prior slipped capital femoral epiphysis (SCFE).
DIAGNOSIS Femoroacetabular impingement.
DISCUSSION In this case, the FAI was secondary to previous SCFE. FAI is early progressive osteoarthritis of the hip joint due to abnormal mechanical relation between proximal femur and acetabulum. Pincer type is due to abnormally shaped acetabulum, whereas cam type is due to abnormal femoral head-neck junction shape [20]. Abnormal femoral headneck junction shape can be seen as a result of prior SCFE, Legg-Calve-Perthes disease, trauma, adult-onset avascular necrosis, or unknown (idiopathic) causes [21]. SCFE occurs most often in overweight boys during their pubescent years. There is posteromedial slip of the femoral epiphysis off the proximal femur.
Case 4.12 Intramuscular Myxoma
CLINICAL HISTORY A 44-year-old woman with a “knot” in her right thigh for a few months.
FINDINGS
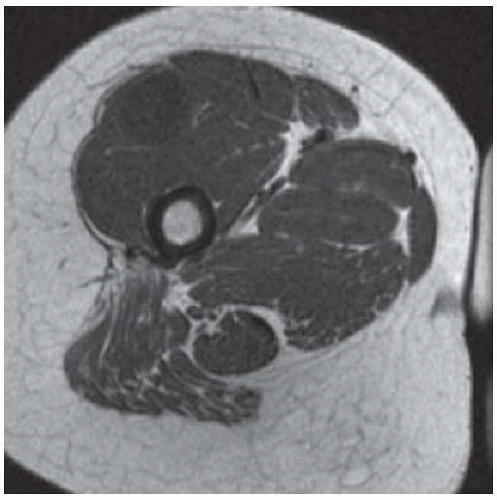
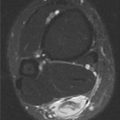
Axial T1-weight MRI shows a round well-circumscribed mass within the vastus lateralis muscle which is isointense to muscle.
On T2-weighted fat-saturated MRI image, this mass is uniformly bright in signal.
After intravenous gadolinium administration, this mass shows patchy enhancement on T1-weighted fat-saturated MRI sequence.
DIFFERENTIAL DIAGNOSIS Soft tissue sarcoma, intramuscular myxoma, nerve sheath tumor.
DIAGNOSIS Intramuscular myxoma.
DISCUSSION The location of the mass is within the vastus lateralis muscle. Intramuscular myxoma is a benign, soft tissue tumor that presents as a deep mass within skeletal muscle [22]. It is a hypocellular and hypovascular lesion with a gelatinous consistency. On CT, the lesion is spherical or ovoid and is sharply marginated, but with no discernible capsule. Attenuation is typically 10 to 30 Hounsfield units, the lesions are homogeneous, and they do not exhibit enhancement. On MRI, the lesions have low signal intensity on T1-weighted images and high signal intensity on T2-weighted images. Typical size at presentation is 6 cm, and the most common location is in the thigh musculature. The possibility of soft tissue sarcoma, particularly sarcomas with myxoid components, can only be definitively excluded by biopsy. CT-guided biopsy may be nondiagnostic if only fine-needle aspiration is used; usually aspiration with a large-bore needle (larger than 20 gauge) is required to sample the gelatinous material. Surgical excision is virtually always curative. The lesion is more common in women (2:1) and is found in adults (mean age 52 years). Association of intramuscular myxomas with fibrous dysplasia of bone is called Mazabraud syndrome [23].
Case 4.13 Fibrodysplasia Ossificans Progressiva
CLINICAL HISTORY A 17-year-old girl with progressive stiffness involving the hip and other joints.
FINDINGS
AP radiograph at presentation reveals a deformity of the femoral neck, with broadening and a small medial inferior protuberance.
Two years later, AP radiograph shows ossification of the sacrotuberous ligament, as well as ossification of a small band from the medial femoral neck to the high iliac crest, and a larger band from the mid femoral neck to the supra-acetabular region.
DIFFERENTIAL DIAGNOSIS Burns, trauma, paralysis, diffuse idiopathic skeletal hyperostosis, fibrodysplasia ossificans progressiva (FOP).
DIAGNOSIS Fibrodysplasia ossificans progressiva.
DISCUSSION Ossification in the soft tissues can be recognized and distinguished from calcification by the presence of a cortical and trabecular structure. The most commonly seen soft tissue ossification is that occurring after trauma, not only in the form of myositis ossificans, but more frequently at sites of ligamentous sprains. Burns and paralysis may also be associated with focal or periarticular soft tissue ossification. Diffuse idiopathic skeletal hyperostosis is a condition of soft tissue ossification, but in this condition it is always entheseal (at the attachment of ligaments, capsules, and tendons to bone).
FOP is a rare and catastrophic genetic disorder of progressive heterotopic ossification, with extensive and cumulative disabling extraskeletal ossification [24]. Individuals with FOP appear normal at birth except for great toe malformations that look like congenital bunions. Then starting first decade of life, patients undergo multiple “flare-ups” in response to minor traumas including vaccinations or minor bumps and bruises from sports events. During these “flare-ups,” there is transient inflammatory reaction that leads to new heterotopic ossifications. This rare condition occurs mostly as new mutations, but when inherited, it is transmitted in autosomal dominant fashion [25]. FOP has been recently linked to mutations in the bone morphogenetic protein type 1 receptor gene [26]. Severe disability results from progressive immobilization of the limbs, jaw, and chest wall. Life-threatening complications include restrictive chest wall disease [27,28] and falls [29]. Falls can be particularly catastrophic, and frequently they initiate a painful flare-up that leads to the permanent loss of movement. Intracranial injuries are common and may be severe, probably the result of deficiencies in coordinated gait and protective reflexes. Most patients die of thoracic insufficiency syndrome.
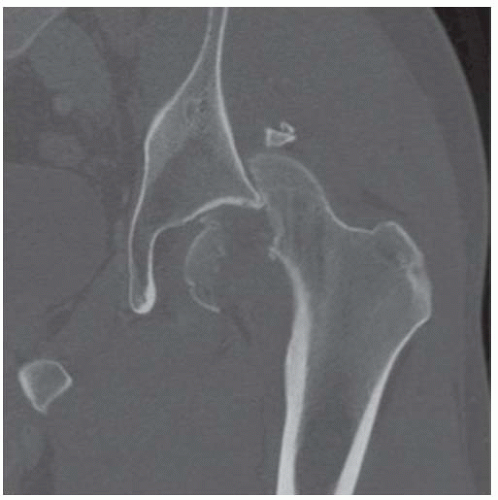
Case 4.14 Posterior Hip Dislocation
CLINICAL HISTORY A 50-year-old man in a high-speed motor vehicle crash.
FINDINGS (A) AP view of the pelvis and (B) AP view of left hip show superior and lateral displacement of the left femur. In addition, there is comminuted fracture of the left femoral head. Axial (C) and coronal (D) CT images of the left hip show posterior hip dislocation with impacted femoral head fracture, with the head coming to rest posterior to the iliac wing.
DIFFERENTIAL DIAGNOSIS Anterior hip dislocation, posterior hip dislocation.
DIAGNOSIS Posterior hip dislocation.
DISCUSSION Hip dislocations result from severe trauma such as motor vehicle accidents. Posterior dislocations, with or without acetabular fractures, account for 85% to 90% of traumatic hip dislocations. The mechanism of injury is a blow along the axis of the femoral shaft with the hip flexed (e.g., hitting the dashboard with the knee). The posterior wall or column of the acetabulum is often fractured, and the femoral shaft or knee may also be injured. Associated fractures of the femoral head occur occasionally, and intra-articular fragments may be particularly problematic for reduction. The thigh is characteristically adducted after a posterior dislocation. CT can identify intra-articular fragments and confirm relocation of the hip after reduction. The presence of gas bubbles in the hip joint capsule after trauma, in the absence of penetrating injury, is a reliable indicator of recent hip dislocation [30]. Most bubbles are located anterior to the femoral neck, but bubbles may also be found posteriorly.
If hip dislocation is unsuspected because of spontaneous relocation or reduction at the scene, the presence of gas should alert the clinician to the possibility of complications. Complications of hip dislocation include avascular necrosis of the femoral head, transient or permanent sciatic nerve palsy, myositis ossificans, and posttraumatic degenerative arthrosis. A posteriorly dislocated hip stretches and twists the external iliac, common femoral, and circumflex arteries, resulting in changes in extraosseous blood flow. Although collateral circulation from gluteal vessels may preserve intraosseous blood flow, delayed relocation may produce a progressive and delayed form of arterial damage that leads to osteonecrosis [31].
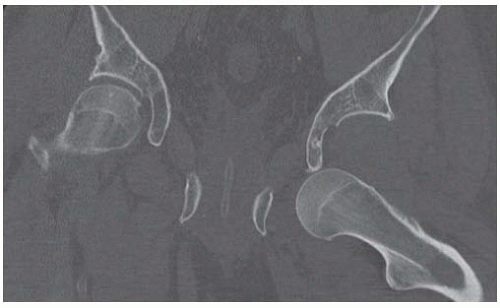
Case 4.15 Anterior Hip Dislocation
CLINICAL HISTORY A 59-year-old man found unconscious after a ground-level fall.
FINDINGS (A) AP radiograph of the pelvis shows anteroinferior dislocation of left femoral head from the acetabulum. The femoral head overlies the obturator foramen and is inferior to the empty acetabulum. The femur is severely abducted. No fracture is seen. Coronal (B) and axial (C) CT images confirm these findings. There are no intra-aricular fracture fragments.
DIFFERENTIAL DIAGNOSIS Anterior hip dislocation, posterior hip dislocation.
DIAGNOSIS Anterior hip dislocation.
DISCUSSION This case illustrates an obviously dislocated hip, but where has the femoral head come to rest? About 11% of traumatic hip dislocations are anterior [32], with the femoral head in most cases resting inferiorly over the obturator foramen, as in this case. The mechanism of injury is forced abduction, external rotation, and flexion of the hip, causing the femoral head to slip anteriorly and medially through the hip capsule, but beneath the strong pubofemoral ligament. The pubofemoral ligament runs from the base of the superior pubic ramus to the lesser trochanter. In approximately 10% of anterior hip dislocations, forced abduction, external rotation, and extension of the hip cause the femoral head to rupture the anterior hip capsule above the pubofemoral ligament, with the femoral head resting superiorly, above the level of the anterior pubic ramus, over the anterior abdominal wall. The iliofemoral ligament may be torn or avulsed from its insertion at the anterior inferior iliac spine. Associated with anterior hip dislocations may be an impaction fracture of the superolateral aspect of the femoral head where it impinges on the anterior inferior rim of the acetabulum after it dislocates. Long-term sequelae include arthritis and osteonecrosis.
Case 4.16 Fluorosis
CLINICAL HISTORY A 43-year-old woman with bone pain and muscle weakness.
FINDINGS AP radiograph of the pelvis shows symmetrically dense bones, involving principally the cortices. The medullary space is present, and the trabecular pattern is normal. There are degenerative changes in the hips, sacroiliac joints, and lumbar spine.
DIFFERENTIAL DIAGNOSIS Osteopetrosis, fluorosis, hypervitaminosis A, renal osteodystrophy, sickle cell anemia, other causes of diffuse sclerosis.
DIAGNOSIS Fluorosis.
DISCUSSION Generalized osteosclerosis and hyperostosis can be seen in a variety of metabolic and systemic conditions. Fluorosis may be related to chronic ingestion of drinking water with endemic, excessive levels of fluoride (four parts or more per million), occupational exposure, or fluoride-containing medication. Endemic regions with large populations include parts of India and China [33,34]. In some circumstances, endemic fluorosis has been described even when fluoride levels in drinking water are not excessive. Tea plants may concentrate the fluoride found in the water and soil. The fluoride content of leaves from these tea plants is related to the length of time they have been growing, resulting in high fluoride levels in tea that is brewed from old leaves and stems, but not in tea brewed from tender leaves and buds [35]. Among occupational exposures, aluminum workers are at particular risk of fluorosis.
The definitive diagnosis is from direct measurements of bone fluoride content. Bone fluoride content is related to exposure, and radiographic findings are found more frequently among those with higher bone fluoride content [36,37]. Radiographic findings include osteopenia, osteosclerosis and hyperostosis involving the axial skeleton, periostitis and enthesopathy in the appendicular skeleton, and dental abnormalities. Early degenerative arthropathy may also be seen. Clinically, there may be decreasing range of motion in the limbs that often progresses to rigidity.
Case 4.17 Rickets
CLINICAL HISTORY A 8-year-old girl with sacroiliac joint pain and chronic disease.
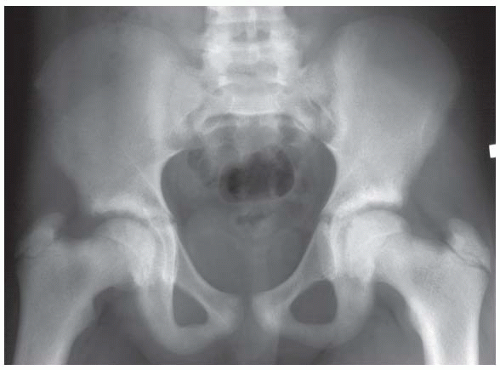 FIGURE 4.17A
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|