Key Points
- •
Focused abdominal ultrasonography is a sensitive and reliable bedside technique to detect intraperitoneal free fluid, although it cannot differentiate specific types of fluid.
- •
Ultrasound improves the success rate and reduces complications related to paracentesis.
- •
Ultrasound is the diagnostic modality of choice for the initial screening of unstable blunt trauma patients for peritoneal free fluid.
Background
The gravitationally dependent anatomic locations where peritoneal fluid preferentially accumulates have been recognized for over a century. It has been known that physical examination of the abdomen has low sensitivity for diagnosing intra-abdominal pathologies. Providers can use ultrasound to detect peritoneal free fluid and guide procedures like paracentesis. Collections of peritoneal free fluid appear black, or anechoic, on ultrasound imaging. Although ultrasound is sensitive to detect small amounts of peritoneal free fluid, it cannot accurately differentiate types of peritoneal free fluid. Therefore, historical clues, such as recent trauma or surgery and presence of preexisting medical conditions, must be considered when interpreting positive findings. The minimum amount of fluid in the peritoneal cavity detectable by ultrasound will vary depending on several factors: patient positioning, etiology of fluid accumulation, elapsed time from onset of fluid accumulation, body habitus, quality of the images, and provider skill level. A range of 100–620 mL has been reported as the minimum amount of intraperitoneal free fluid detectable by ultrasound.
Etiologies of peritoneal free fluid can be divided into traumatic and nontraumatic causes. In trauma patients, the presence of peritoneal free fluid is a surrogate marker for solid organ injury. Hemoperitoneum from blunt trauma most commonly originates in the upper abdomen from injury to the spleen and liver. The hepatorenal recess is the most sensitive single area for hemoperitoneum secondary to blunt trauma. Nontraumatic etiologies of peritoneal free fluid include emergent causes, such as ruptured ectopic pregnancy, and nonemergent causes, such as chronic ascites due to cirrhosis.
When used for procedural guidance, ultrasound can guide site selection to perform a diagnostic or therapeutic paracentesis. Ultrasound guidance for paracentesis has been shown to improve procedural success rates and decrease complications, hospital costs, and length of stay.
Normal Anatomy
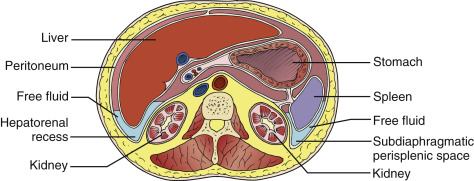
Detection of peritoneal fluid by ultrasound requires an understanding of the anatomic spaces where peritoneal free fluid accumulates. The peritoneal cavity is subdivided into greater and lesser peritoneal sacs. The greater peritoneal sac is further divided into supracolic and infracolic compartments by the transverse mesocolon. Pathologic fluid can pass between the supracolic and infracolic compartments via the paracolic gutters, the peritoneal spaces lateral to the ascending and descending colon. In a supine position gravity causes fluid in the upper abdomen to flow from the left upper quadrant and right paracolic gutter into the right upper quadrant. In an upright position, gravity causes this same fluid to flow into the pelvis.
In the upright and supine positions, the most gravitationally dependent area of the combined abdominopelvic peritoneal space is the pelvis, specifically caudal to the sacral promontory. In the abdominal peritoneal space alone, the hepatorenal recess, or Morison’s pouch, is the most gravitationally dependent area above the pelvic inlet. If the source of fluid is above the pelvic inlet and fluid accumulation begins in a supine position, fluid gravitates toward the hepatorenal recess for three reasons. First, the hepatorenal peritoneal reflection is more posterior relative to other abdominal structures. Second, the lordotic curvature of the lumbar spine and anterior location of the sacral promontory relative to the hepatorenal recess prevents free fluid from flowing into the pelvis. Third, the phrenicocolic ligament , a peritoneal reflection in the left upper quadrant, shunts blood from the left upper quadrant toward the hepatorenal recess in the right upper quadrant. However, if a patient has been upright for a significant amount of time, the pathologic fluid will pool in the more dependent pelvis regardless of the site of origin.
Image Acquisition
A low-frequency curvilinear or phased-array transducer is needed to examine the abdomen and pelvis with ultrasound. Three areas must be evaluated to detect peritoneal free fluid: right upper quadrant, left upper quadrant, and pelvis ( Figure 23.1 ). The liver, spleen, and urine-filled bladder serve as the major acoustic windows to evaluate the right upper quadrant, left upper quadrant, and pelvis, respectively. An empty or ruptured bladder, subcutaneous emphysema, bowel or stomach gas, wound dressings, and asplenia can reduce the sensitivity of ultrasound to detect intraperitoneal free fluid from these windows.
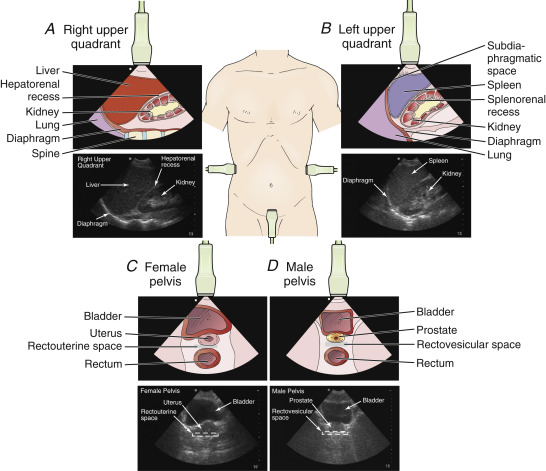
Right Upper Quadrant
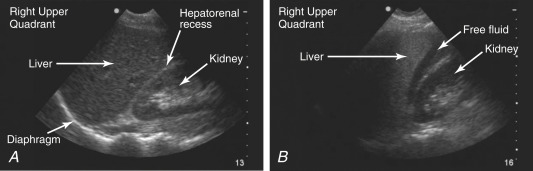
In the right upper quadrant, three spaces should be visualized: below the diaphragm, between the liver and kidney, and the inferior pole of the right kidney in the right paracolic gutter. Place the transducer in a coronal plane in the midaxillary line between the 9th and 11th intercostal spaces with the transducer marker pointing cephalad ( Figure 23.2 ). Adjust the transducer position and angle to visualize the right upper quadrant, focusing on the potential space between the liver and kidney (hepatorenal recess, or Morison’s pouch) ( Figure 23.3 ). Fan the transducer from anterior to posterior through the entire hepatorenal recess to visualize the inferior tip of the liver, looking for free fluid. The inferior pole of the right kidney should be visualized along with the right paracolic gutter. Angle the transducer superiorly to image the right subdiaphragmatic space. Figure 23.4 and ![]() demonstrate free fluid in the right upper quadrant.
demonstrate free fluid in the right upper quadrant.

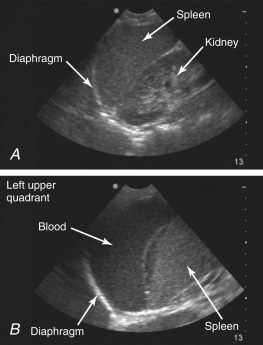
Left Upper Quadrant
In the left upper quadrant, three spaces should be visualized: below the diaphragm in the parasplenic space, between the spleen and left kidney, and the inferior pole of the left kidney with the left paracolic gutter. In contrast to the right upper quadrant, the left upper quadrant is best visualized with the transducer in a more posterior and superior position due to the location and size of the spleen. Place the transducer in a coronal plane on the posterior axillary line between the 6th and 9th intercostal spaces with the transducer marker pointing cephalad ( Figure 23.5 ). The image may be improved by rotating the transducer 10-20 degrees clockwise with the transducer marker pointing slightly posteriorly. If repositioning is possible, the patient can be placed in a right lateral decubitus position to allow more posterior access to the splenic window. Evaluate the left subdiaphragmatic and splenorenal spaces for any signs of free fluid ( Figure 23.6 and ![]() ). Similar to the right upper quadrant, fan the transducer through the splenorenal space from anterior to posterior. The inferior poles of the kidney and spleen should be visualized along with the superior portion of the left paracolic gutter.
). Similar to the right upper quadrant, fan the transducer through the splenorenal space from anterior to posterior. The inferior poles of the kidney and spleen should be visualized along with the superior portion of the left paracolic gutter.

Pelvis
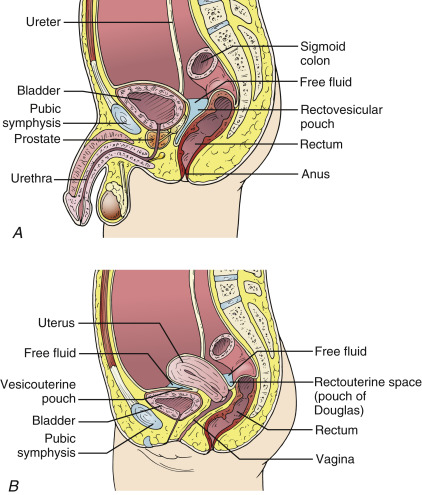
Peritoneal free fluid in the pelvis accumulates in the rectovesicular space in men and the rectouterine space, or pouch of Douglas, in women ( Figure 23.7 ). To image the pelvic space, place the transducer in a transverse plane just superior to the pubic symphysis with the transducer marker pointed toward the patient’s right ( Figure 23.8 ). Fan the transducer inferiorly into the pelvis until the bladder is visualized. Set the imaging depth to view the bladder in the top one-third to one-half of the screen. Posterior acoustic enhancement should be appreciated posterior to the bladder. It is important to fan the transducer to visualize the entire bladder from fundus to neck to thoroughly evaluate the rectovesicular or rectouterine spaces for a free fluid collection ( Figure 23.9 and ![]() ). Rotate the transducer 90 degrees clockwise to obtain sagittal views of the bladder and scan the entire bladder from left to right. If the bladder has been decompressed using a urinary catheter, the bladder can be refilled with warm normal saline through the injection port while clamping the catheter distally to prevent drainage. If the patient does not have a urinary catheter in place, a temporary catheter can be placed to inflate the bladder with saline.
). Rotate the transducer 90 degrees clockwise to obtain sagittal views of the bladder and scan the entire bladder from left to right. If the bladder has been decompressed using a urinary catheter, the bladder can be refilled with warm normal saline through the injection port while clamping the catheter distally to prevent drainage. If the patient does not have a urinary catheter in place, a temporary catheter can be placed to inflate the bladder with saline.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree