Key Points
- •
Evaluation of right ventricular function in patients with undifferentiated respiratory failure and shock is essential to guide management.
- •
The objective of point-of-care right ventricular assessment is to evaluate for acute right heart failure caused by an increase in pulmonary pressure or direct right ventricular injury.
- •
Right ventricular failure can be rapidly recognized using point-of-care ultrasound through a qualitative analysis of right ventricular size, function, and interventricular septal kinetics.
Background
The left ventricle (LV) has historically been the focus of hemodynamic and echocardiographic evaluation of the heart. More recently, the importance of right ventricular (RV) function has been recognized, and guidelines have emerged describing standard ways to assess normal RV dimensions and function.
Evaluation of the RV is essential to help diagnose and manage shock and respiratory failure in acutely ill patients. Conditions that may cause acute RV failure, either through sudden pulmonary hypertension (e.g., pulmonary embolism [PE], mechanical ventilation, acute respiratory distress syndrome [ARDS]) or through primary RV failure (e.g., trauma or infarction) should be considered, depending on clinical circumstances.
Assessment of RV function to identify acute right heart failure is essential in management of patients with shock. In addition to guiding decisions about inotropic support and fluid resuscitation, RV structure and function has been shown to be a prognostic indicator for patients with left heart failure, acute PE, ARDS, and severe sepsis. Furthermore, acute RV dysfunction may occur in patients with septic shock. In these patients, RV size can guide fluid resuscitation. Giving fluids in the context of a dysfunctional RV with interventricular septal bowing can further compromise LV filling, worsening LV output and a progressive shock state.
In patients with suspected PE who are in circulatory failure, a small study has suggested that upwards of 90% of patients with PE as the cause of their shock will have features of RV failure on point-of-care cardiac ultrasound. For those with established PE without shock, if signs of RV failure are demonstrated by ultrasound, enduring pulmonary hypertension is a risk, and early aggressive therapy (thrombolysis or embolectomy) should be considered based on current guidelines.
In patients with ARDS, evaluation of RV function can guide titration of positive end-expiratory pressure (PEEP). Indiscriminate increases in PEEP increase pulmonary capillary resistance and increase RV afterload. RV pressure overload leads to acute RV dilation and reduced RV contractility, potentially leading to decreased LV output and a corresponding decrease in oxygen delivery. Assessing RV dimensions during titration of PEEP can help determine when this maximum threshold is reached.
Anatomy
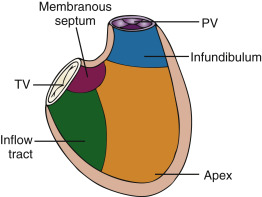
The right ventricle is located in the mediastinum behind the middle to lower part of the sternum. It is positioned anterior to the LV, and the RV chamber is divided anatomically into three parts: an inflow tract (sinus), outflow tract (infundibulum), and apex. Even though the apical muscle is heavily trabeculated, the main contributors of RV systolic function are the sinus and infundibulum ( Figures 15.1 and 15.2 ). During systole, muscles of the sinus primarily contract to elevate RV pressure, and muscles of the infundibulum stretch to modulate pressure and prolong systole.
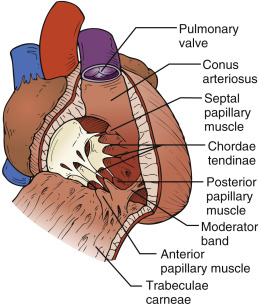
RV contraction is complex and occurs in phases. First, the trabeculated sinus contracts longitudinally, shortening the distance from base to apex. Second, the RV free wall contracts radially toward the interventricular septum, shortening the circumference of the chamber. Last, torsion from contraction of the left ventricular base and apex pulls the right ventricle to contract similarly.
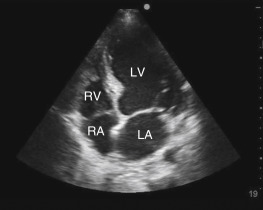
The RV free wall is normally thinner than the LV free wall because the RV pumps blood into the pulmonary vasculature, which has lower resistance compared to the systemic circulation. The normal RV chamber size is approximately two thirds the size of the LV chamber. The RV has a crescent shape when viewed in transverse cross section from a parasternal short-axis view ( Figure 15.3 ) and a triangular shape when viewed in a coronal plane from an apical 4-chamber (A4C) view ( Figure 15.4 ).

Assessment of RV from Common Views
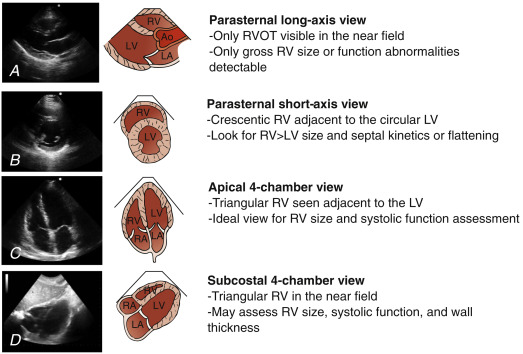
The RV is best visualized using the standard echocardiography views that are discussed in Chapter 13 . Because of its complexity in structure and function, the RV should be assessed from all available cardiac views. Interpretation of RV size and function from the most common cardiac views includes the following ( Figure 15.5 ):
- 1.
Parasternal long-axis view: Visualization of the proximal RV outflow tract and RV free wall is seen in the near field ( Figure 15.5 A). This view may detect gross RV dilation or hypokinesis, but the RV cannot be assessed to be “normal” from this single view. Findings should be confirmed in additional views before making any important clinical decisions.
- 2.
Parasternal short-axis view (mid-ventricular level): Normally, the crescent-shaped RV sits next to the circular LV in this view. This view allows assessment of relative RV size by direct comparison to the size of the neighboring LV ( Figure 15.5 B). Further, the interventricular septum is well visualized and altered septal kinetics are seen with RV pressure overload (ranging from a septal “bounce” to a flattened septum—see interpretation below).
- 3.
Apical 4-chamber view (A4C): This is the most informative view for global RV assessment. With a side-by-side comparison of right and left ventricles, the relative RV size can be easily interpreted when an on-axis view is acquired ( Figure 15.5 C). The interventricular septum is well visualized allowing interpretation of septal kinetics. The RV systolic function is usually qualitatively estimated, but a quantitative estimate may also be calculated (see discussion of tricuspid annular plane systolic excursion [TAPSE] below). Alignment of blood flow parallel to the ultrasound beam in this view is ideal for Doppler flow evaluation of the tricuspid valve or determination of pulmonary pressure for providers trained in such techniques.
- 4.
Subcostal 4-chamber view (S4C): The RV is seen as a triangular chamber adjacent to the liver in the near field ( Figure 15.5 D). A subcostal 4-chamber view provides a side-by-side comparison of size and function of the RV to the LV. Although off-axis imaging is a common pitfall, this view can be extremely valuable to evaluate the RV when an A4C view cannot be obtained. Because the RV free wall is nearly perpendicular to the ultrasound beam, this view can provide excellent visualization of the RV endocardium and is well suited to assess RV wall thickness—a finding that can help differentiate acute from chronic RV disease.
Interpretation of RV Size and Function
Point-of-care evaluation of the RV is often performed in patients with acute circulatory dysfunction or respiratory failure. In these patients, RV evaluation is focused to determine the presence or absence of right heart failure. Acute right heart failure commonly results from either direct RV tissue damage or a sudden increase in resistance to the pulmonary circulation (acute cor pulmonale). Direct RV tissue damage typically occurs from infarction or blunt trauma, whereas acute cor pulmonale typically results from a large PE, metabolic causes, ARDS, or mechanical ventilation at high pressures.
In addition to acute RV failure, many other important diagnostic findings may be obtained from a detailed RV evaluation. Some applications, such as characterization of tricuspid regurgitation, determination of RV systolic pressure, evaluation for congenital anomalies, or evaluation for or detection of endocarditis, require additional training.
Assessment of the RV should be performed systematically to look for characteristic signs of RV stress or failure. The constellation of findings described below varies between patients depending on the etiology and chronicity of disease, physiologic adaptation, and therapies initiated.
- 1.
RV size: The RV free wall musculature is relatively weak, and in acute RV failure the chamber dilates. The most common and practical approach to determine RV enlargement is to perform a direct side-by-side comparison to the LV. RV size assessment is most intuitively done from the A4C view but can also be appreciated from the S4C view. In the A4C view, the transducer should be oriented to appropriately visualize the lateral free wall of the RV and acquire the largest possible RV chamber width ( Figure 15.6 and
 ). A qualitative assessment of RV size is most commonly performed using the following parameters in end-diastole ( Figure 15.7 ):
). A qualitative assessment of RV size is most commonly performed using the following parameters in end-diastole ( Figure 15.7 ):
- a.
Normal RV size: <2/3 LV size
- b.
Moderate dilation: RV size >2/3 LV size
- c.
Severe dilation: RV size >LV size
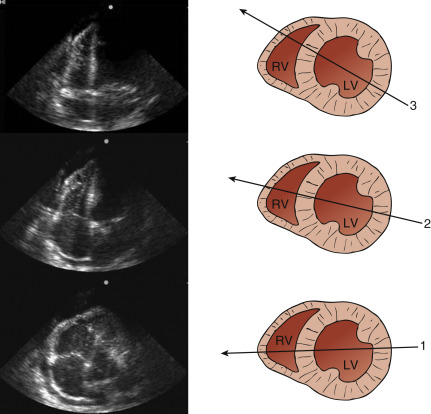
Figure 15.6
An apical 4-chamber image of the right ventricle should be acquired at its greatest dimension (line 1). Off-axis imaging can lead to significant errors in right ventricular size and function assessment (lines 2 and 3). RV, right ventricle; LV, left ventricle.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


- a.