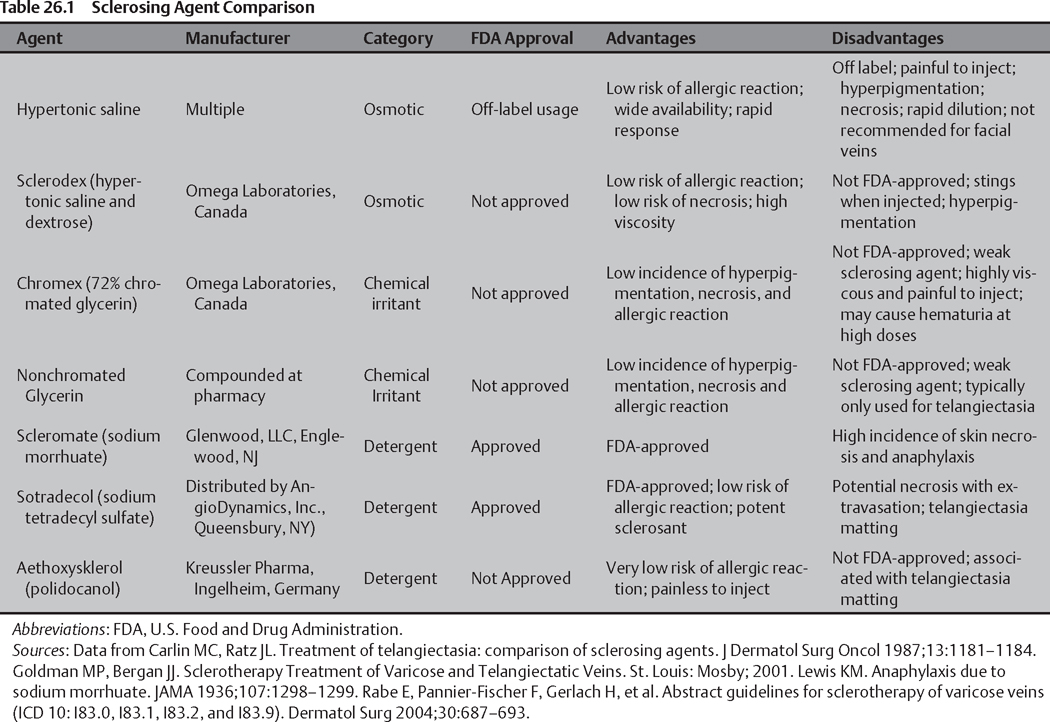
26 Sclerotherapy and Ambulatory Phlebectomy Lowell S. Kabnick Lower extremity venous insufficiency is a common condition that affects millions of people each year. Venous insufficiency frequently surfaces in the form of varicose veins or telangiectasia (spider veins); however, the disease can also result in hyperpigmentation, edema, and ulcers. Several risk factors are associated with the development of venous insufficiency, including family history, obesity, older age, pregnancy, and female gender. Studies over the years have demonstrated that women are approximately twice as likely as men to develop the disease. In 2003, Criqui et al1 studied 4422 limbs and found that 27.7% of women had varicose veins compared with 15% of men. In 2007, estimates showed that 19.4 million women and 8.9 million men in the United States over the age of 40 will present with varicose veins in 2007.2 Ambulatory phlebectomy (AP) and sclerotherapy (ST) are safe and economical procedures that have proven to be effective methods for treating incompetent veins. Patients are able to undergo these procedures in an outpatient setting, using local anesthesia with little or no recovery time. Sclerotherapy involves the intravascular injection of a sclerosing agent to produce endothelial damage and eventual fibrosis of the target vein. Ambulatory phlebectomy permanently removes undesirable veins through a small number of skin punctures, with minimal scarring or adverse effects. Treatment using sclerotherapy or ambulatory phlebectomy may be medically indicated if the veins are symptomatic, whereas asymptomatic veins are classified as a cosmetic procedure. In this chapter several aspects of sclerotherapy and ambulatory phlebectomy are covered including treatment strategies, diagnostic methods, indications, contraindications, procedural techniques, and potential complications. When treating venous insufficiency, the goal is to first treat the highest point of reflux. Accepted treatment strategies to accomplish this include compression therapy, sclerotherapy, ambulatory phlebectomy, endovenous thermal ablation, and topical laser. Although each treatment modality has its specific advantages and indications, there is significant overlap. Sclerotherapy and AP are similar treatment strategies; at present, there is a debate as to which is better. There is a lack of evidence-based literature to support the superiority of either procedure. Until conclusive evidence emerges, it is critical for the physician to be adept at both procedures. There is also substantial controversy over whether ST or AP should be performed at the same time that truncal reflux is being eradicated. The existing data suggest advantages to either ST or AP in conjunction with truncal reflux treatment and to performing the procedures independently. In a retrospective study by Welch,3 the initial success of endovenous ablation to treat truncal reflux allowed most patients to defer subsequent stab phlebectomy. Conversely, in a controlled study by Mekako et al,4 patients who underwent concomitant endovenous laser therapy and ambulatory phlebectomy did not need to return for ensuing phlebectomy procedures. When considering the treatment algorithm, the physician must be selective and make decisions based on the needs of each individual patient. It is appropriate to combine procedures if the varicose veins involve the zone of influence regarding the truncal reflux. Staging is indicated if the varicose veins lie outside the zones of influence. A complete history and physical examination should be performed for each patient. In most cases, a duplex ultrasound (DUS) is performed as part of the preoperative evaluation. Ultrasound examination allows for the identification of sources of reflux that may require treatment before moving forward with sclerotherapy or ambulatory phlebectomy of the target vein. Venous evaluation is also vital in diagnosing contraindications to ST or AP, thus avoiding serious complications. Photographs of the target veins should be taken to subsequently compare with the results of the procedure. In addition, transillumination is beneficial for identifying reticular and feeding veins associated with telangiectasias. Common transilluminating devices include the Veinlite (TransLite, Sugar Land, TX) and VeinViewer (Luminetx Corp., Memphis, TN). Sclerotherapy is a method that has existed since the 1930s for the treatment of lower extremity varicosities. This technique involves the intravenous injection of a chemical agent into the lumen of a vessel. The agent produces endothelial damage to the vessel wall that causes initial thrombosis and subsequent fibrosis. The intent of sclerotherapy is to effectively eliminate the target vein after the highest point of reflux is treated. The injection of an ideal sclerosing agent into a vessel induces an intense inflammatory response that results in endothelial damage. This leads to thrombus formation, fibrosis, and reabsorption of the vessel. ST is a versatile technique and is indicated to treat several levels of incompetent veins including varicose veins <8 mm, reticular veins (2 to 4 mm), telangiectasias (0.1 to 2 mm), recurrent varicosities, unsightly normal veins of the hands and feet, tributaries, perforators, and failed segments of endothermal ablation. Indications vary according to the technique used and the skill set of the physician. Other areas appropriate for sclerotherapy treatment include small congenital malformations (such as hemangiomas), vascular malformations, and facial telangiectasia. The primary limitation of sclerotherapy treatment is vein diameter; the sclerosing agent must make contact with the vein wall to cause endothelial damage. Blood flow within larger veins may dissipate the agent and prevent it from effectively interacting with the vein wall. Sclerosing agents can be grouped into categories based on their mechanism of action for producing endothelial damage. The currently available solutions are categorized as osmotic, alcohol, or detergent. Ideal characteristics of a sclerosing agent include ability to effectively damage the endothelium, low incidence of adverse events, and painless to inject. Each agent category and specific agent has its own advantages and disadvantages that should be considered when choosing an agent (Table 26.1).5–8 Osmotic agents are thought to cause dehydration of the endothelial cells through osmosis, which leads to endothelial destruction.9 There are two primary agents used for lower extremity varicosities: hypertonic saline (23.4% sodium chloride) and a hypertonic saline and dextrose mixture, such as Sclerodex (Omega Laboratories, Montreal, Canada). Alcohol agents are weak sclerosants that cause irreversible destruction of endothelial cells upon contact. The main alcohol agent used for sclerotherapy is chromated glycerin 72% (Chromex, Omega Laboratories, Canada). Nonchromated glycerin is also utilized and is only available through compounding pharmacies. The typical mixture for this solution is two parts 72% nonchromated glycerin to one part 1% lidocaine with epinephrine. Detergent agents are strong sclerosants that produce destruction of the target vein by aggregating on the endohelial wall to cause thrombosis. Currently, two agents are U.S. Food and Drug Administration (FDA-) approved for the treatment of lower extremity venous insufficiency: sodium morrhuate (Scleromate; Glenwood LLC, Englewood, NJ) and sodium tetradecyl sulfate (STS; Sotradecol, distributed exclusively in the United States by AngioDynamics Inc., Queensbury, NY). Although sodium morrhuate is FDA-approved, it is not a preferred detergent agent due to its high incidence of skin necrosis and anaphylaxis.7 Sotradecol was previously available in the United States through Elkins Sinn (then a division of Wyeth-Ayerst, Madison, NJ). In 2000 the company discontinued the production and marketing of STS because the integrity of the active pharmaceutical ingredient (API) could not be maintained to meet FDA standards. An industrial cleaning chemical was being used the make the API, which elevated the FDA concerns about the presence of contaminants. Sodium tetradecyl sulfate has a long history of safety and efficacy for use in sclerosing telangiectasia, reticular veins, and varicose veins. A major advantage of Sotradecol is that it is the only preferred, FDA-approved sclerosing agent currently available. A third detergent agent is polidocanol (POL; Aethoxysklerol, Kreussler Pharma, Ingelheim, Germany). This agent is not FDA-approved; however, it is currently the only approved agent in Germany for sclerotherapy and has been utilized there for over 20 years. In previous studies comparing polidocanol to STS, fewer complications were reported with POL. It should be noted that these studies were conducted with the former industrial-grade STS manufactured by Elkins Sinn. The currently available Sotradecol is a more pure version of STS and there is a paucity of studies to evaluate this new agent. Sclerotherapy has absolute and relative contraindications that are critical to review before commencing with patient treatment (Table 26.2).8,10,11 Before commencing with treatment, digital photographs of the target veins should be obtained to document the appearance before sclerotherapy is performed. Larger target veins, such as varicose veins should be traced with a surgical marker while the patient is standing as they may be difficult or impossible to identify during recumbency. Smaller veins such as telangiectasia and reticular veins typically do not require preoperative marking. When sclerotherapy is combined with saphenectomy or endothermal ablation of the great or small saphenous veins, sclerotherapy below the knee should be performed second. If using a staging approach, the great or small saphenous veins should be treated first, and sclerotherapy should follow several weeks later. This method allows the existing truncal varicosities to decrease in size or disappear before further procedures.12 Depending on the number and severity of diseased veins, several sclerotherapy treatments may be necessary to eliminate the veins. It is important to explain this process to patients and establish the expectation that several sessions could be required.
Treatment Strategies
Staged versus Unstaged Procedures
Diagnostic Methods
Sclerotherapy
Indications
Types of Sclerotherapy Agents
Osmotic Agents
Alcohol Agents
Detergent Agents
Contraindications
Technique
Preoperative Preparation
Surgical Plan
| Absolute Contraindications | Relative Contraindications |
| Known allergy to the sclerosant | Asthma |
| Acute cellulitis | Late complications in diabetes |
| Acute respiratory or skin diseases | Hypercoagulable state |