SECTION VI INTERVENTIONAL IMAGING
Essentials 1
Questions
1. The uterine artery anatomically arises from which major pelvic arterial branch?
A. The posterior division of the internal iliac artery
B. The anterior division of the internal iliac artery
C. The inferior mesenteric artery
D. The anterior division of the inferior gluteal artery
2. Uterine fibroid embolization (UFE) is typically performed using which type of embolic material?
A. Coils
B. Glue
C. Ethanol
D. Particles
3. What is the best preprocedural planning study for uterine fibroid embolization?
A. Magnetic resonance imaging
B. Ultrasound
C. Computed tomography
D. Hysterosalpingogram
Answers and Explanations
Question 1
B. Correct! The uterine artery traditionally arises from the anterior division of the internal iliac artery on each side of the pelvis.
Other choices and discussion
A. The uterine artery traditionally arises from the anterior, not the posterior, division of the internal iliac artery.
C. The inferior mesenteric artery supplies the left colon and rectum.
D. The inferior gluteal artery (like the uterine artery) is a branch of the anterior division of the internal iliac artery, but it does not supply the uterus.
Question 2
D. Correct! Particles, in various forms, are used to provide optimal distal embolization of fibroids during UFE. Either spherical embolic beads or irregular polyvinyl alcohol particles are employed. A total of 500 to 700 micron and 700 to 900 micron particles are the most common sizes used. Studies have shown that smaller particles do not provide a benefit over these larger particles, except in cases of adenomyosis.
Following treatment, intracavitary fibroids may slough and pass as fragments. Retained fragments have the potential to become infected. Uterine necrosis is a rare post z embolization phenomenon.
Other choices and discussion
A. Coils are good at achieving vessel occlusion, but do not provide enough distal occlusion for an optimal UFE result.
B. Glue is a liquid embolic and can achieve deeper penetration than coils. However, it is not traditionally used for fibroid embolization. It is expensive and, at times, challenging to work with.
C. Ethanol is a liquid embolic that is a powerful sclerosing agent. Potential limitations include risk of tissue necrosis and difficulty in achieving predictable results.
Question 3
A. Correct! MRI is the preferred study in the United States to evaluate a patient prior to fibroid embolization. MRI provides information on fibroid vascularity (based on enhancement), fibroid location, potential presence of adnexal or additional uterine masses, potential presence of adenomyosis, and helps to define other vessels that may supply the fibroids. MRI may also be used to evaluate posttreatment efficacy.
Fibroid embolization should not be performed if there is a suspicion for leiomyosarcoma. Differentiating leiomyosarcoma from uterine fibroids can be quite challenging with imaging. Patients that have tremendous bulk symptoms, or patients that demand guaranteed eradication of their fibroids, may benefit from hysterectomy or myomectomy over UFE. If uterine artery embolization does not successfully treat all of the fibroids, an ovarian supply to the residual fibroids should be considered.
Other choices and discussion
B. Ultrasound is also a very good way to evaluate the uterus and ovaries. MRI has advantages over ultrasound, as listed above. However, ultrasound is a reasonable preprocedural approach for UFE when MRI is not available.
C. Computed tomography does not provide the detail needed for UFE that MRI and ultrasound offer.
D. HSG is typically used to evaluate female patients for an anatomic source of infertility or to assess the efficacy of implantable contraception devices in the fallopian tube. HSG does not provide robust information about fibroids. Theoretically, HSG could be helpful in evaluating intracavitary fibroids.
Suggested Readings
Deshumkh SP, Gonsalves CF, Guglielmo FF, Mitchell DG. Role of MRI imaging of uterine leiomyomas before and after embolization. Radiographics 2012;32(6):E251–E281Top Tips
A total of 500 to 700 micron or 700 to 900 micron particles are typically used for uterine artery embolization.
Cervical fibroids do not respond as well to UFE because they often have alternate blood supply.
The symptom that drives most women to seek treatment for fibroids is menorrhagia.
Essentials 2
Questions
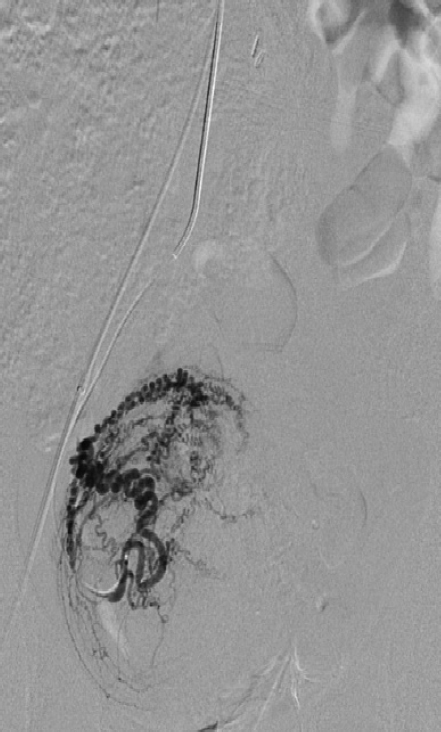
1. The test image depicts what abnormality?
A. Arteriovenous fistula
B. Pseudoaneurysm
C. Arterial thrombus
D. Arterial dissection
2. Which of the following methods of treatment for a pseudoaneurysm in this location is LEAST desirable?
A. Ultrasound-guided compression
B. Thrombin injection
C. Surgical repair
D. Covered stent placement
3. Which pseudoaneurysm characteristics are most amenable to safe treatment with thrombin injection?
A. Short, wide neck
B. Long, wide neck
C. Long, narrow neck
D. All of the above
Answers and Explanations
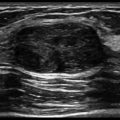
Question 1
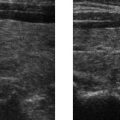
B. Correct! This represents a pseudoaneurysm. To-and-fro flow is depicted as red and blue color Doppler flow (yin-yang sign). This is seen within a hypoechoic sac adjacent to an artery. This is the typical sonographic appearance of a pseudoaneurysm. These usually occur after catheterization or other trauma. Pseudoaneurysms that are symptomatic and/or are > 2 cm are frequently treated. Small pseudoaneurysms often thrombose without treatment.
Other choices and discussion
A. An AV fistula would present with arterial flow in the adjacent vein, not the to-and-fro color Doppler appearance shown here.
C. Pseudoaneurysms may contain thrombus, but no thrombus is present here.
D. Iatrogenic dissection is a potential complication of catheterization, but no dissection flap is identified here.
Question 2
D. Correct! Covered stent placement across a joint, such as the hip, is undesirable because of the risk of stent fracture from the motion of the joint.
Other choices and discussion
A. Ultrasound-guided compression is a traditional treatment used for common femoral artery pseudoaneurysm. Ultrasound is less invasive than surgery and yields good results. Ultrasound-guided compression is less successful in patients on anticoagulation.
B. Thrombin injection into the pseudoaneurysm sac has now become the standard treatment for common femoral artery pseudoaneurysm.
C. Historically, surgery was the first-line treatment for pseudoaneurysm that failed manual compression.
Question 3
C. Correct! A long, narrow neck to a pseudoaneurysm is the most favorable configuration to allow for safe thrombin injection. A long distance to the parent artery and a narrow channel of flow between the pseudoaneurysm and artery make the likelihood of inadvertent introduction of thrombin into the native artery less likely.
Thrombin is usually reconstituted to 1000 U per mL. However, some practitioners dilute it further to 100 U per mL. Another consideration in choosing a therapy is that some patients may be allergic to thrombin.
The other choices have increased risk of complications.
Suggested Readings
Webber GW, Jang J, Gustavson S, Olin JW. Contemporary management of postcatheterization pseudoaneurysms. Circulation 2007;115:2666–2674Top Tips
Thrombin injection should be performed in a part of the pseudoaneurysm sac away from the neck. This reduces the chance of embolization of thrombin down the extremity.
The success rate for thrombin injection is > 90%.
Thrombin injection should not be attempted on pseudoaneurysms that arise from arterial anastomoses or from mycotic pseudoaneurysms.
Essentials 3
Questions
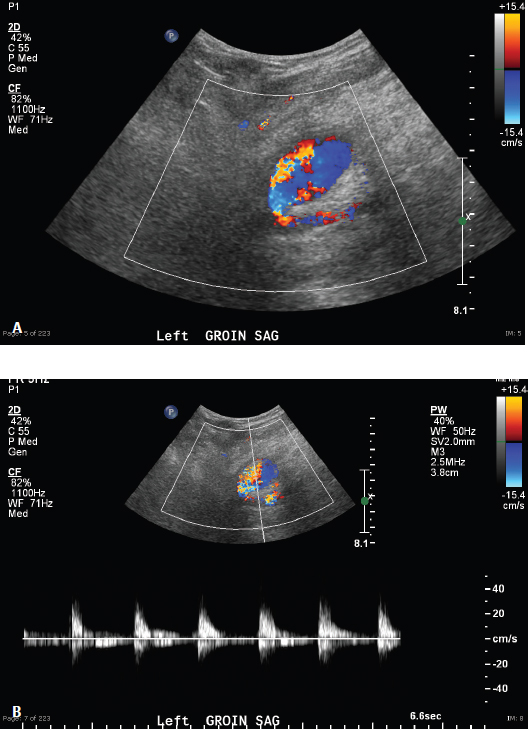
1. What is the most likely clinical history for this 25-year-old patient?
A. Atrial fibrillation
B. Renal failure on dialysis
C. Cold hands
D. Post trauma with pain
E. Unilateral arm swelling
2. Match the letter to the correct vessel on the test image. _ Brachial artery
_ Interosseous artery
_ Radial artery
_ Ulnar artery
3. The deep palmar arch is typically supplied by which artery?
A. Radial artery
B. Ulnar artery
C. Princeps pollicis artery
D. Radialis indicis artery
4. How does a Barbeau test differ from an Allen test?
A. A blood pressure cuff is used in an Allen test.
B. A pulse oximeter is used in a Barbeau test.
C. There are four classifications for the result of an Allen test.
D. The Barbeau test determines the patency of the radial artery.
Answers and Explanations
Question 1
C. Correct! The patient presented with bilateral cold hands. This patient has vasoconstriction that is reversible when the extremity is warmed. This finding is consistent with a thermally related vasoconstrictive process (Raynaud syndrome). Raynaud syndrome is not typically diagnosed with angiography or any given endovascular treatment.
Other choices and discussion
A. Atrial fibrillation resulting in emboli to all of the forearm arteries is unlikely in this 25-year-old. Additionally, reversal of impaired circulation with warming of the arm would not be expected.
B. Although it is unknown if the patient has renal failure, there does not appear to be calcification of the arteries, and no fistula is identified. If a fistula was present, steal could be considered.
D. There is no evidence of active extravasation/bleeding, aneurysm, or pseudoaneurysm to support a history of trauma. It is unlikely for changes from trauma to reverse after warming the extremity.
E. Ischemia can present with swelling, but in this case the impeded arterial flow is reversible when the extremity is warmed. This patient is more likely to complain of cold hands than of swelling. In addition, the patient’s arms are rather slender on the unsubtracted angiogram images (rather than swollen).
Question 2
A. Brachial artery
B. Interosseous artery
C. Radial artery
D. Ulnar artery
Question 3
A. Correct! The radial artery typically provides the dominant supply to the deep palmar arch.
Other choices and discussion
B. The ulnar artery usually supplies the superficial arch.
C. There is no thenar artery in the hand. The thumb is supplied by the princeps pollicis artery.
D. The radialis indicis does not supply the deep arch but arises close to the princeps pollicis artery.
Question 4
B. Correct! A pulse oximeter is used in a Barbeau test. A pulse oximeter is typically placed on the thumb, whereas the radial artery is occluded during a Barbeau test.
Other choices and discussion
A. A blood pressure cuff is typically not used in either test. Both the Allen and the Barbeau involve manually occluding one or both of the major arteries to the hand (ulnar and radial).
C. There are four classifications of the results of a Barbeau test. An Allen test is usually positive or negative.
D. The Barbeau test typically tests the sufficiency of the ulnar artery to supply the hand as the radial artery is occluded during the test. It is not a test of radial artery patency.
Suggested Readings
Kim YH, Ng SW, Seo HS, Chang AH. Classification of Raynaud’s disease based on angiographic features. J Plast Reconstr Aesthest Surg 2011;64(11):1503–1511 Kotowycz MA, Dzavik V. Radial artery patency after transradial catheterization. Circ Cardiovasc Interv 2012;5:127–133Top Tips
Raynaud syndrome can be a primary or secondary disorder, with secondary Raynaud syndrome related to an underlying disease (usually connective tissue disease).
A Barbeau test is typically performed prior to radial artery catheterization to determine the patient’s ability to tolerate radial artery occlusion. If there is no change in pulse oximetry or plethysmographic waveform, then the radial artery is likely to be safe to use for catheterization.
The radial artery typically supplies the deep palmar arch, and the ulnar artery supplies the superficial palmar arch.
Essentials 4
Questions
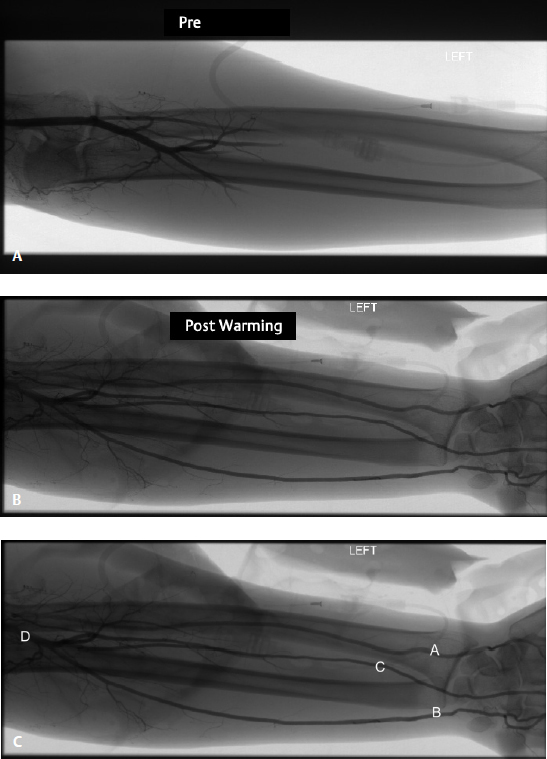
1. This patient, who is in need of an inferior vena cava (IVC) filter, has which of the following anatomic variants?
A. Duplicated IVC
B. Retroaortic left renal vein
C. Circumaortic left renal vein
D. Standard caval anatomy
E. Caval agenesis
2. In patients with more than one left renal vein, the preferred position for placement of an IVC filter is? (Select the ONE best answer.)
A. In between the renal veins
B. Below the lowest renal vein
C. Over the ostium of the superior renal vein
D. In the left iliac vein
E. In the superior vena cava
3. The incidence of new DVT in patients after placement of an IVC filter is:
A. Increased compared to those patients without IVC filters
B. The same as those patients without IVC filters
C. Decreased compared to those patients without IVC filters
D. Unknown
E. Dependent on the anticoagulation status of the patient
Answers and Explanations
Question 1
C. Correct! This patient has a circumaortic left renal vein. Circumaortic left renal veins can be seen in up to 17% of the population.
The other choices are all incorrect.
Question 2
B. Correct! Below the lowest renal vein is an acceptable placement for an IVC filter. A filter below the lowest renal vein does not permit clot to potentially circumvent the filter. IVC filters can either be placed from an internal jugular or a femoral approach. The choice of approach is determined by the operator and by clinical factors. For example, if a patient has a right common femoral deep venous thrombosis, a left common femoral or internal jugular approach is preferable. Some filters are low profile enough to permit placement from a brachial or large basilic vein of the arm.
Other choices and discussion
A. Placement between the renal veins is suboptimal because of the theoretical risk of clot entering a lower renal vein, which is below the filter, and subsequently emerging from a higher renal vein, which is above the filter, permitting a pulmonary embolism to occur.
C. Placement over the ostium of a renal vein is suboptimal because this impedes venous drainage from that kidney, which could lead to renal vein thrombosis. Most filters are intended to be positioned 1 cm below the ostium of the renal vein. In this case, placement of the filter either below the lowest renal vein or above the highest renal vein (which is off-label use) is optimal, in terms of reducing the chance of thrombus circumventing the filter.
D. A filter in the left iliac vein is sometimes placed in the setting of a duplicated IVC (not present in this case). In that instance, a second filter would need to be placed in the IVC or in the right iliac vein to protect against a right lower extremity DVT.
E. A superior vena cava filter would not protect against lower extremity DVT.
Question 3
A. Correct! The chance of developing DVT is increased in patients with an IVC filter in place. This is counterintuitive, but has been borne out in the literature. This is one of the reasons there is a push to remove retrievable filters when caval filtration is no longer needed.
Radiologists looking at imaging on patients with IVC filters should note: penetration of the legs beyond the confines of the IVC, filter tilt, migration of position from the prior study, and filter fracture. All of these may indicate an IVC filter complication.
The other choices are all incorrect.
Suggested Readings
Fedullo PF, Roberts A. Placement of vena cava filters and their complications. UpToDate. September 2015. http://www.uptodate.com/contents/placement-of-vena-cava-filters-and-their-complications Karazincir S, Balci A, Gorur S, Sumbas H, Kiper AN. Incidence of the retroaortic left renal vein in patients with varicocele. J Ultrasound Med 2007;26(5):601–604Top Tips
IVC filters come in permanent and retrievable varieties. Nevertheless, all US Food and Drug Administration–approved filters are approved for permanent use.
The US Food and Drug Administration recommends removal of retrievable filters if there is no longer a clinical necessity. It is believed that there is an increased risk of adverse events (filter fracture, penetration of legs, etc.) with longer indwelling times.
In general, the longer a filter has been in, the harder it will be to remove. Each manufacturer of retrievable filters has a suggested retrieval window for each of their products.
Essentials 5
Questions
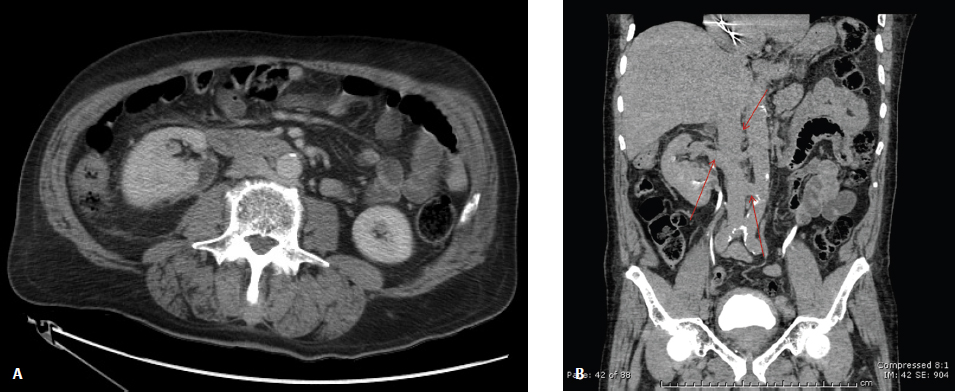
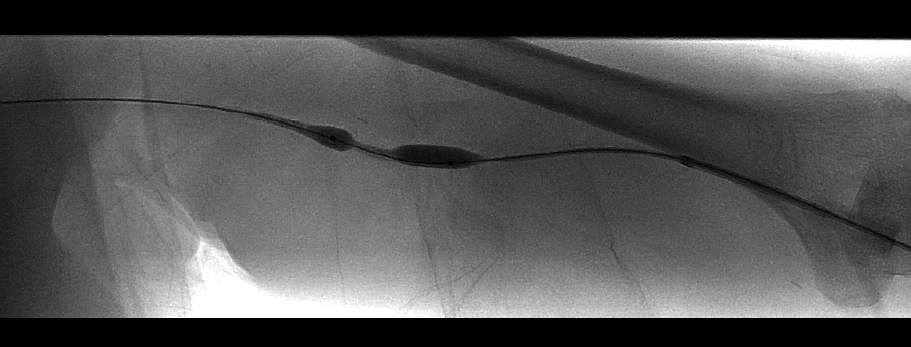
1. What finding on physical exam is expected based on this image taken from an elderly patient on dialysis with an antecubital fossa fistula?
A. Weak thrill
B. Mottled hand
C. Swollen arm
D. Pulsatility
E. Strong thrill
2. In the event of contrast extravasation after angioplasty of a fistula, which ONE of the following is an appropriate initial maneuver?
A. Placing a tourniquet in the axillary region
B. Putting up a balloon at the site of rupture
C. Placing coils at the site of rupture
D. Injecting thrombin at the site of rupture
E. Using a suture to ligate the fistula
3. In an arteriovenous dialysis graft, where is the most common site of stenosis?
A. Arterial anastomosis
B. Venous anastomosis
C. Intragraft
D. Subclavian
E. Superior vena cava
Answers and Explanations
Question 1
D. Correct! Pulsatility would be expected. When a patient has outflow stenosis of the fistula back to the heart, there is backpressure. This backpressure presents on physical exam with absence of a thrill and increased pulsatility, as the arterial pressure pushes against a fixed obstruction.
Other choices and discussion
A. Arterial stenosis would cause a weak or absent thrill.
B. The patient’s arterial flow to the hand is not likely compromised by the fistula outflow stenosis. There is an entity known as a steal phenomenon whereby there is relatively increased flow through the fistula compared to the hand, resulting in symptoms. In this case, the outflow stenosis may function to force more blood to the hand than through the fistula, so the hand is less likely to be ischemic than when the fistula is fully patent.
C. The patient’s arm is unlikely to be swollen, as swelling in these patients is often due to outflow stenosis at the level of the axillary, subclavian, or brachiocephalic veins. This stenosis is in the upper arm but not at the level of the subclavian, which would inhibit all venous drainage of that extremity and more likely result in swelling.
E. A thrill is created by turbulent flow through a fistula. A strong thrill is a reassuring physical exam finding. In the case of a stenosis in the fistula circuit, the normal thrill may be diminished or absent. In this patient with outflow stenosis, increased pulsatility would be expected rather than a strong thrill. This is due to the preservation of arterial pulsations as the arterial pressure is transmitted against a fixed obstruction.
Question 2
B. Correct! A balloon at the site of rupture will often arrest further bleeding. The efficacy of this treatment may be confirmed by excluding further bleeding after taking down the balloon. A balloon is also useful in temporizing the situation, until the operator is prepared to place a covered stent across the area of rupture. After angioplasty, technical success is defined as having < 30% residual stenosis.
Other choices and discussion
A. A tourniquet in the axillary region to stop arterial inflow into the arm may be used as a final effort after other measures have failed. A tourniquet is not a good initial treatment for extravasation, as it causes increased backpressure by obstructing venous outflow, and this may lead to further bleeding from the site of rupture.
C. While coils can cause thrombus that will stop the bleeding, they create an irreversible occlusion and are therefore not typically used to treat contained fistula ruptures.
D. Thrombin is not typically used to treat bleeding after angioplasty because of the potential risk of creating fistula thrombosis or generate a clot that may enter the central circulation.
E. Ligation of the fistula with a suture would make the dialysis access permanently unusable. This would only be considered as an emergent surgical procedure for life-threatening bleeding.
Question 3
B. Correct! The venous anastomosis is the most common site for stenosis in dialysis grafts.
The other choices are all incorrect. Although intragraft, subclavian, and central stenosis may occur, they are all less common sites than at the venous anastomosis.
Suggested Readings
Beathard GA. Physical examination of the dialysis vascular access. Semin Dial 1998;11:231–236 Kornfield ZN, Kwak A, Soulen MC, Patel AA, Kobrin SM, Cohen RM, Mantell MD, Chittams JL, Tereotola SO. Incidence and management of percutaneous transluminal angioplasty—induced venous rupture in the “fistula first” era. J Vasc Interv Radiol 2009;20:744–751Top Tips
Fistulas (native veins) have longer patency than grafts (synthetic material), so fistulas are often placed first.
Grafts have both a venous and an arterial anastomosis, and fistulas only have an arterial anastomosis.
Fistulas with outflow stenosis may have prolonged bleeding after removal of dialysis needles, in addition to increased fistula pulsatility on physical exam.
Essentials 6
Questions
1. What is the most common etiology for this finding?
A. Infectious
B. Atherosclerotic
C. Hypoplastic
D. Iatrogenic
E. Congenital
2. Patients with these imaging findings may present with a classic triad of symptoms, which includes which ONE of the following?
A. Abdominal pain
B. Renal failure
C. Back pain
D. Impotence
E. Thigh claudication
3. Why are many patients asymptomatic?
A. Longevity of the findings
B. Coexisting diabetes
C. Collateral pathways preserving distal blood flow
D. Nerve injury from ischemia
E. Muscular atrophy
Answers and Explanations
Question 1
B. Correct! This patient has distal aortic occlusion. Atherosclerotic disease is the most common etiology.
The other options are all incorrect—that is, although all of the other options (infectious, hypoplastic, iatrogenic, and congenital pathologies) can lead to aortic occlusion, none are more common than atherosclerosis.
Question 2
D. Correct! These patients, if symptomatic, classically present with a triad of buttock claudication, absent or decreased femoral pulses, and impotence. This patient has flow in his common femoral arteries, so he likely has palpable femoral pulses.
Other choices and discussion
A. These patients do not usually present with abdominal pain.
B. The occlusion does not extend to the renal arteries, so these patients do not typically present with renal failure.
C. These patients do not usually present with back pain.
E. These patients classically present with buttock claudication, although thigh claudication is possible.
Question 3
C. Correct! These patients are sometimes asymptomatic because collateral pathways maintain blood flow to the pelvis and lower extremities. These collateral pathways include systemicsystemic pathways (e.g., internal mammary artery to inferior epigastric artery), visceral-visceral pathways, and visceralsystemic pathways.
Aortoiliac disease can be described by the TransAtlantic Inter-Society Consensus criteria, with lesion complexity increasing from type A to type D. Type A is a short (usually under 3 cm) common iliac or external iliac lesion that can be treated from an endovascular approach, whereas Type D is a > 10 cm iliac stenosis or occlusion that may need surgical treatment.
The other choices are all incorrect. Many of these patients do have diabetes, but there is a better answer for why these patients are often asymptomatic.
Suggested Readings
Jaffan AAA, Murphy TP. Aortoiliac revascularization. In Mauro MA, Murphy KPJ, Thomson KR, et al (eds). Image-Guided Interventions. Philadelphia, PA: Saunders; 2013: 189–209Top Tips
Leriche syndrome describes the triad of buttock claudication, impotence, and absent or decreased femoral pulses that occurs in the setting of chronic aortoiliac occlusive disease. Risk factors include smoking, diabetes, hypertension, and hyperlipidemia.
Many such patients are asymptomatic, due to rich collateral pathways that allow for lower extremity blood flow.
Treatment may be purely endovascular or surgical. Higher TransAtlantic Inter-Society Consensus lesions are at an increased risk for loss of patency.
Essentials 7
Case
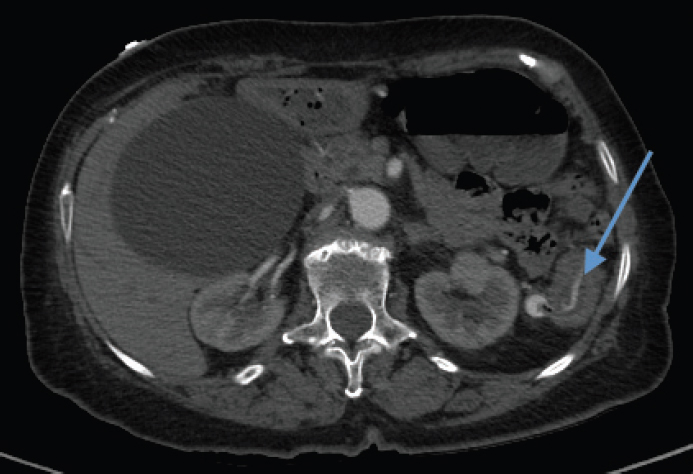
A 60-year-old man presents with bright red blood per rectum. Image is from a gastrointestinal (GI) bleed protocol computed tomography angiogram (CTA).
Questions
1. The vessel that normally supplies the splenic flexure also supplies which other organ?
A. Small bowel
B. Rectum
C. Spleen
D. Pancreas
E. Cecum
2. Which ONE of the following is a potential advantage of a tagged red blood cell scan over a CTA for a GI bleed?
A. Detection of slower bleeding rates
B. Precise anatomic bleed localization
C. Detailed depiction of arterial anatomy
D. Shorter acquisition time
E. More readily available
3. Assuming normal anatomy, from which location should catheter-based therapy for this GI bleed take place?
A. Proximal SMA
B. Proximal IMA
C. Proximal middle colic artery
D. Proximal left colic artery
E. Distal to the marginal artery
Answers and Explanations
Question 1
B. Correct! The rectum is supplied by the inferior mesenteric artery (IMA), which also supplies the splenic flexure.
Other choices and discussion
A. The small bowel is supplied by the superior mesenteric artery (SMA).
C. The spleen is supplied by the splenic artery, which arises from the celiac artery.
D. The pancreas is supplied by multiple arteries originating from the celiac artery and the SMA.
E. The cecum is supplied by the SMA.
Question 2
A. Correct! Detection of slower bleeding rates is an advantage of the nuclear medicine study. A tagged red blood cell scan can detect bleeding rates as low as 0.1 mL/min, compared to CTA, which can detect bleeding rates as low as 0.3 to 0.7 mL/min. Catheter angiography can detect bleeding rates as low as 0.5 to 1 mL/min.
A GI bleed CTA protocol usually includes a noncontrast CT, an arterial phase intravenous contrast CT, and a venous phase delayed CT. No oral contrast is given. With this technique, any new high-density material in the bowel on the arterial phase that becomes more prominent on the venous phase is likely active bleeding. At most centers, angiography with embolization is attempted prior to surgery given its decreased morbidity.
The other choices are all incorrect.
Precise anatomic localization of the bleed, detailed depiction of arterial anatomy, shorter acquisition time, and more readily available modality are all advantages of CTA over nuclear scintigraphy.
Question 3
E. Correct! Distal to the marginal artery. The treatment of lower GI bleeds should occur as distally as possible, to minimize the risk of infarction of a large segment of bowel and prevent collateral flow to the source of bleeding. Treatment should originate beyond the mesenteric border of the colon (marginal or terminal artery in the IMA distribution, or vasa rectae in the SMA distribution). If initial angiography does not reveal active extravasation, then provocative angiography may be considered. Although the yield is low, it may be a worthwhile effort in patients with occult and recurrent lower GI bleeding.
Other choices and discussion
A. The SMA does not normally supply the splenic flexure.
B. A branch of the IMA should be treated, but treatment should be distal, not proximal.
C. The middle colic artery is usually a branch off the SMA, not the IMA.
D. A distal left colic artery branch should be treated, not the proximal left colic artery.
Suggested Readings
Darcy M. Management of lower gastrointestinal bleeding. In Mauro MA, Murphy KPJ, Thomson KR, et al (eds). Image-Guided Interventions. Philadelphia, PA: Saunders; 2013: 374–379 Funaki B. On-call treatment of acute gastrointestinal hemorrhage. Semin Intervent Radiol 2006;23(3):215–222Top Tips
Both CTA and tagged red blood cell scans are appropriate noninvasive exams to investigate lower GI bleeding. Colonoscopy may also be considered. Common etiologies for lower GI bleeding are diverticular hemorrhage and angiodysplasia.
Patients with a positive CTA or tagged red blood cell scan are usually then investigated with angiography. In rare cases where angiography is not available or the patient is too unstable, surgery is considered.
When treating lower GI bleeding with interventional techniques, the use of superselective catheterization and embolization is imperative to minimize the risk of bowel infarction or re-bleeding. The microcatheter should be placed as close as possible to the bleeding source prior to embolization.
Essentials 8
Questions
1. These findings are more likely to be significant:
A. If present during expiration
B. If the narrowing is > 50%
C. If the patient has clinical symptoms
D. If the lactate level is elevated
E. Regardless of the patient presentation
2. The first-line treatment for this patient if he is symptomatic is:
A. Surgery
B. Endovascular stent placement
C. Celiac ganglion block
D. Medical management
E. No treatment
3. The usual location of the median arcuate ligament is:
A. Anterior to the celiac artery
B. Posterior to the celiac artery but anterior to the aorta
C. Inferior to the celiac artery
D. Superior to the celiac artery
E. Posterior to the aorta
Answers and Explanations
Question 1
C. Correct! These findings are more likely to be significant if the patient has clinical symptoms. The diagnosis of median arcuate ligament syndrome is based on clinical and radiologic findings. This patient suffered from abdominal pain and weight loss. The characteristic finding on imaging is focal narrowing of the proximal celiac axis with a hooked shape. This appearance can be transient on expiration, but is more concerning if seen during inspiration. Poststenotic dilatation or collateral vessels are adjunct findings concerning for pathologic narrowing.
Median arcuate ligament syndrome commonly occurs in young females 20 to 40 years old with symptoms of epigastric pain, which may or may not be postprandial, and weight loss. On physical exam, an abdominal bruit that varies with respiration may be audible in the epigastric region. The symptoms are believed to be due to stenosis of the celiac artery, although some believe that celiac ganglion irritation also contributes. Complications of median arcuate ligament syndrome include aneurysm formation of the pancreaticoduodenal arcades, gastroepiploic, or celiac arteries.
Other choices and discussion
A. This appearance is concerning if present during inspiration, as in this case. Conversely, this narrowing may be transient on expiration and is often clinically insignificant in those instances. On inspiration, the diaphragm lowers and the compression by the median arcuate ligament should be the least severe.
B. The degree of narrowing itself does not often directly correlate with the severity of patient symptoms.
D. An elevated lactate level does not contribute to the diagnosis.
E. This appearance is not concerning if the patient is asymptomatic.
Question 2
A. Correct! Surgical release of the median arcuate ligament is the best first treatment for this patient. The patient in this case did, in fact, have surgical release of the median arcuate ligament with subsequent improvement in his symptoms.
Other choices and discussion
B. Endovascular stent placement before surgery has a high failure rate. If symptoms persist after surgery, stent placement may be considered.
C. Although the symptoms of median arcuate ligament syndrome may be due in part to celiac ganglion irritation, a celiac ganglion block alone is not standard treatment for median arcuate ligament syndrome.
D. Medical management is not appropriate.
E. Given the presence of symptoms with this radiologic appearance, treatment is warranted.
Question 3
D. Correct! Normally the median arcuate ligament is superior to the celiac artery.
The other choices are incorrect. The median arcuate ligament is anterior to the celiac axis in a minority of cases, where it may cause compression of the celiac artery.
Suggested Readings
Horton K, Talamini M, Fishman E. Median arcuate ligament syndrome: evaluation with CT angiography. Radiographics 2005;25:1117–1182 Tracci M. Median arcuate ligament compression of the mesenteric vasculature. Tech Vasc Interv Radiol 2015;18(1):43–50Top Tips
The median arcuate ligament is a fibrous ligament connecting the diaphragmatic crura. It is normally situated superior to the celiac artery, but may be found anterior to the celiac artery in 10 to 24% of patients.
While this diagnosis is traditionally made on conventional angiography, computed tomography angiography and magnetic resonance angiography are now increasingly used for this purpose. The imaging findings are exacerbated/exaggerated on expiration.
Treatment initially consists of surgical decompression. Endovascular revascularization of the celiac artery may be performed at the same time or afterward. Endovascular treatment alone (without surgical treatment) has a high failure rate.
Essentials 9
Case
A young female patient presents with left lower extremity swelling, deep venous thrombosis, and this finding on magnetic resonance angiography and angiography.
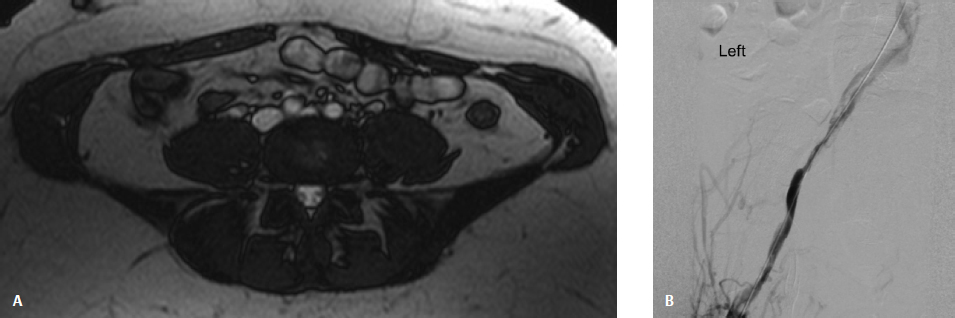
Questions
1. What is the most likely etiology for this finding?
A. Iatrogenic
B. Mechanical
C. Traumatic
D. Inflammatory
E. Degenerative
2. The affected vessel is the:
A. Left common iliac artery
B. Left common iliac vein
C. Left external iliac vein
D. Right common iliac artery
E. Right common iliac vein
3. What is the best treatment strategy for this patient?
A. Endovascular techniques, including angioplasty with possible stent placement
B. Surgical management
C. Conservative management
D. Systemic anticoagulation alone
E. More workup is needed before a treatment plan can be made
Answers and Explanations
Question 1
B. Correct! This patient has May-Thurner syndrome. The most likely etiology is mechanical. The compression defect in the left common iliac vein is the result of compression by the passing right common iliac artery anteriorly and the lumbar vertebral body posteriorly. The presentation may be acute, with left lower extremity pain or swelling, or chronic, with chronic venous insufficiency. A rare presentation is that of pulmonary emboli.
Anatomic compression of the left common iliac vein is seen in up to 25% of asymptomatic patients. Degree of luminal stenosis > 50% and the presence of collateral veins are imaging clues that suggest May-Thurner syndrome. This syndrome likely contributes to the slightly higher incidence of left-sided deep venous thrombosis (DVT). High clinical suspicion is necessary to recognize the syndrome.
Other choices and discussion
A. Although oral contraceptives can contribute to this syndrome, they cannot by themselves explain the specific imaging findings.
C. There is no given history of trauma or findings to support this diagnosis on the provided image.
D. Inflammation alone cannot account for the imaging finding.
E. Degenerative changes do not result in DVT.
Question 2
B. Correct! The compression defect is in the left common iliac vein, which is compressed by the right common iliac artery that passes anterior to the left common iliac vein. Although ultrasound is often used as the initial imaging study, this modality can be quite limited in visualization of the pelvic veins. Both computed tomography and magnetic resonance venography are very useful in delineating the anatomy and estimating the degree of stenosis. Intravascular ultrasound can also demonstrate the degree of stenosis and spur.
The other choices are all incorrect.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree