The appearance of osseous, labral, hyaline cartilage, ligament, muscle, and tendon variants and pitfalls are discussed with attention to the keys to distinguishing each of the findings from pathologic lesions of the shoulder.
MR imaging of the shoulder is commonly used to evaluate patients with shoulder impingement, acute and chronic rotator cuff pathology, and instability lesions. Interpreting radiologists, therefore, need to apply knowledge not only of the imaging appearance of these pathologic conditions but also of normal anatomic variants and imaging artifacts. The ability to discern these findings from true pathology is essential in providing a useful and accurate interpretation for referring clinicians. The appearance of osseous, labral, hyaline cartilage, ligament, muscle, and tendon variants and pitfalls is discussed with attention to the keys to distinguishing each of the findings from pathologic lesions of the shoulder.
Osseous structures
Acromion
The acromion process has been classified into different types based on shape. Bigliani and colleagues first described three types based on the undersurface morphology:
Type 1: straight or flat
Type 2: curved
Type 3: hooked.
Since this initial description, a fourth type has been added describing a convex or upward pointing undersurface.
These acromial morphologic variations were initially described by using scapular Y-view radiographs; however, they also can be accurately characterized on shoulder MR imaging using sagittal oblique and coronal oblique sequences ( Fig. 1 ).
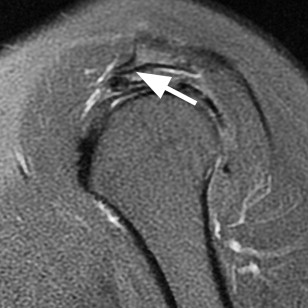
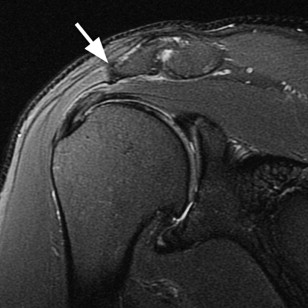
The association of differing acromial morphology with subacromial impingement and rotator cuff disease has been disputed. Some investigators think that a type 3 acromion is developmental in origin from traction of the coracoacromial ligament, creating an enthesophyte, whereas others consider it a morphologic variant. In either case, a type 3 acromion or prominent enthesophyte can play a primary role in subacromial impingement syndrome and in injury to the anterior leading edge of the supraspinatus. Other morphologic changes, such as a downward-projecting keel spur from the acromion ( Fig. 2 ) or lateral downsloping of the acromion ( Fig. 3 ), also likely result in the development of rotator cuff pathology. Although disputed, the relationship between acromial morphology and subacromial impingement remains an often applied rationale for subacromial decompression surgery in patients with rotator cuff pathology.
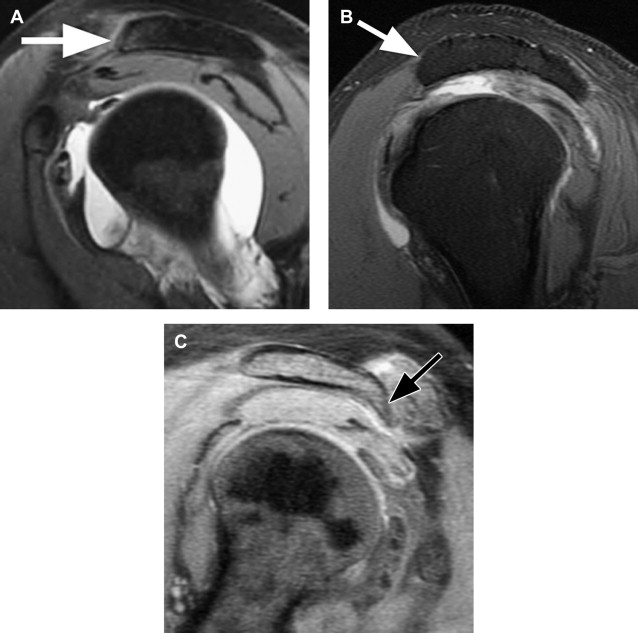
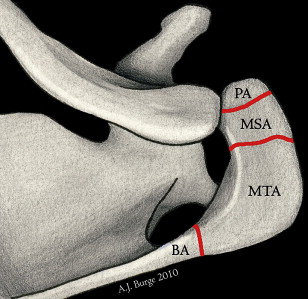
The acromion is formed by multiple ossification centers, one that appears at 3 months of fetal life and others that follow during later teenage years. Embryologically, the acromion is divided into the basiacromion, meta-acromion, mesoacromion, and preacromion ( Fig. 4 ). After age 25 years, nonfusion of these ossification centers can result in formation of an accessory ossicle, or os acromiale. This is found in up to 15% of shoulders and, when present, is bilateral in one-third of cases. Multiple shapes and sizes of the os acromiale are possible based on the site of fusion failure. An os acromiale is best identified on axial MR images, where a signal gap is seen between the fat-containing marrow of the distal acromion and the nonfused os ( Fig. 5 ). The os forms a pseudoarticulation with the base of the acromion via fibrous tissue, periosteum, cartilage, or synovium accounting for the variability seen on T2-weighted images. On sagittal MR imaging, the presence of the os can be determined because it is the site of attachment of the coracoacromial ligament, which inserts on its anterior-inferior border. The presence of a double acromioclavicular joint may be seen on sagittal images, where the os is seen articulating with both the native acromion and the clavicle. It is important to identify an os acromiale because it may play a role in the development of shoulder impingement symptoms due to inferior displacement with deltoid contraction. Its presence may also serve as a contraindication to subacromial decompression surgery in cases of clinical shoulder impingement. Equally important is that degenerative changes across the synchondrosis or associated acromioclavicular degeneration may be an isolated source of shoulder pain ( Fig. 6 ).
Humerus
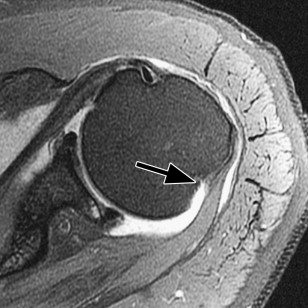
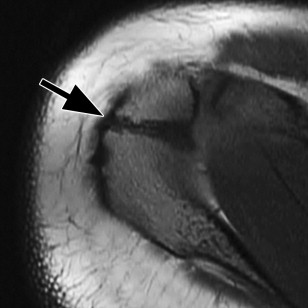
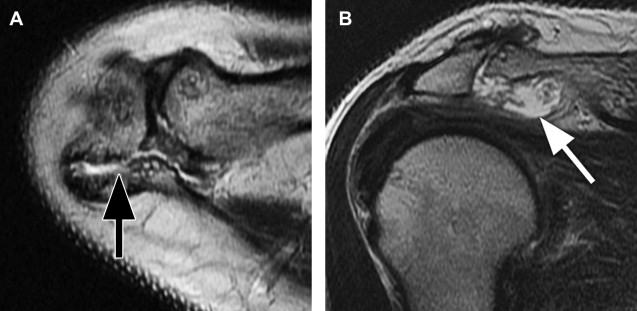
The proximal humerus, including the head, greater and lesser tuberosities, and anatomic neck, all contribute to the articulation of the glenohumeral joint. The bicipital or intertubercular groove, located between the greater and lesser tuberosities, contains the extra-articular long head of the biceps tendon at the anterior aspect of the humerus. An additional, normal groove exists at the posterior aspect of the humerus near the junction of the head and proximal diaphysis ( Fig. 7 ). This is a potential source of a false-positive interpretation on axial MR imaging and should not be mistaken for a Hill-Sachs lesion, a posterolateral impaction fracture of the humeral head as a result of anterior shoulder dislocation ( Fig. 8 ). This distinction becomes important in patients with a history of glenohumeral dislocation, because the presence of a Hill-Sachs lesion may warrant further surgical treatment in addition to repair of the anterior-inferior glenoid and labrum. There can be overlap in the appearance of a normal posterolateral humeral groove and a Hill-Sachs lesion, although delineation of the two can be determined by their location within the humerus. Hill-Sachs lesions are visible on the uppermost axial sections of the humerus and are positioned within 5 mm of the top of the humeral head superolaterally. The normal anatomic groove of the humerus usually lies 20 to 30 mm from the superior humeral head and is positioned more posteriorly and medial on axial sections. The depth and width of the posterolateral defect are not reliable indicators to its origin.