5.5 Anterior Chest Wall as a Whole
5.5.1 Case 97 (Fig. 5.37)

Case description
Referring physician: radiologist.
Prior history and clinical question: A 35-year-old woman complained of intolerable pain in the right parasternal area and posterior lower chest. She claimed that her pains had worsened after pregnancy and during lactation. The referring radiologist requested confirmation of his diagnosis.
Radiologic Findings
The MR images in Fig. 5.37 b, c show areas of increased edema-like signal intensity in the upper right quadrant of the manubrium sterni and adjacent soft tissues, also in the upper body of the sternum and adjacent structures on the right side. The CT image (Fig. 5.37 a) reveals sclerotic changes around the manubriosternal synchondrosis, mixed destructive and sclerotic changes in the first manubriocostal synchondrosis, and—just visible in the section—sclerosis in the second sternocostal synchondrosis (only the most representative images are shown in the figure). Spinal MRI in Fig. 5.37 f shows increased signal intensity at the anterior inferior corner of the T11 vertebral body; a similar finding was noted at the upper left corner of T12 (not pictured here). Correlative CT shows a mixed pattern of bone destruction and proliferation at the diskoligamentous attachment of T11 and T12 (Fig. 5.37 d, e).
Location
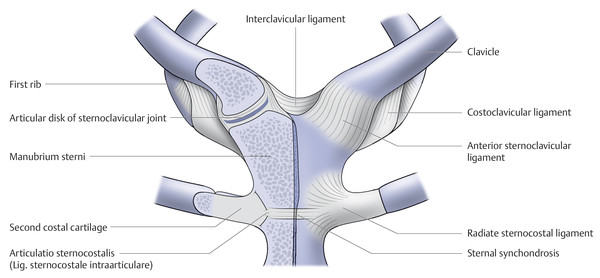
All of the above changes are located at the following entheses in the anterior chest wall, see the anatomic diagram in Fig. 5.38:
Manubriosternal synchondrosis
Costomanubrial synchondrosis and ligament
Costosternal synchondrosis and ligament
The changes in the two lower thoracic vertebrae are also located at an enthesis: the discovertebral junction.
Pathoanatomic Background of the Findings
The mixed radiologic pattern of bone destruction and proliferation at entheses is typical of a chronic, nonbacterial inflammation, that is, an enthesitis with associated osteitis, which explains the edema-like signal on MRI. The findings are based on a generalized enthesitis in the anterior chest wall and lower thoracic spine.
Assignment to a Possible Basic Entity
The pathoanatomic substrate for the radiologic changes is identified by name in the previous paragraph, so we may proceed to the discussion.
Synopsis and Discussion
The patient suffers from a generalized enthesitis that may be classified as belonging to the group of (seronegative) spondyloarthritis. The distribution pattern of the changes is consistent with psoriatic arthritis, although no visible signs of psoriasis or pustulosis palmoplantaris were noted when the images were obtained. The family history was also negative for psoriasis, and the personal history and clinical presentation showed no evidence of Reiter symptoms or bowel disease. Since the patient may eventually develop psoriasis or pustulosis palmoplantaris—though we do not believe the hypothesis of psoriatic arthritis or spondyloarthritis without psoriasis—it appears reasonable to offer a preliminary diagnosis of “undifferentiated spondyloarthritis.” Also, we cannot justify a classification of ankylosing spondylitis or spondyloarthritis because the case does not meet the necessary diagnostic criteria (e.g., the Ankylosing Spondylitis Assessment Study [ASAS] criteria). The disease in the present case is still in an initial phase, and it is hoped that antirheumatic drug therapy, especially with tumor necrosis factor α blockers or antagonists, can prevent progression of the disease.
The initial changes in the anterior chest wall may progress to sternocostoclavicular hyperostosis (SCCH; synonyms: sternocostal arthro-osteitis, intersternocostoclavicular ossification), which is often associated initially with significant complaints, painful swelling, and soft-tissue inflammation that is detectable by imaging. This occurred in one patient with a variant of psoriasis, namely pustulosis palmoplantaris (PPP) (Fig. 5.39). The “bull’s head sign” on bone scans is a typical finding (Fig. 5.40 and Fig. 5.43 d).


SCCH may also have an asymmetric onset, as in the case of a 44-year-old woman with classic psoriasis (Fig. 5.41 a–f). The mixed pattern of bone destruction and proliferation in this and another case (43-year-old woman, Fig. 5.42 a–d) is clearly demonstrated by CT and can be documented but not proven by MRI, as demonstrated in Fig. 5.42 a.


The late stage is marked by plaque-like ossification in the sternocostoclavicular region (Fig. 5.43 a–c, e).

The dominant feature in some cases is manubriosternal synchondritis, as illustrated by the case of a woman with PPP and spondyloarthritis in a lower thoracic vertebra (Fig. 5.44). As in other forms of spondyloarthritis, concomitant involvement of the costotransverse joints is a typical finding (Fig. 5.43 b).

Diseases from the group of seronegative spondyloarthropathies that are associated with pustular skin lesions are also called SAPHO syndrome or, more specifically, pustular arthro-osteitis (PAO) or enthesio-osteitis (PEO), as illustrated in Case 39 and Case 40. Based on information from dermatologists and our own observations, PPP is more prevalent among smokers. We even had a case in which PPP plus extensive destructive-proliferative changes in the scapula and SCCH (see Fig. 5.13 in Case 84) regressed over a period of 10 years after the patient quit smoking. Clinical experience indicates that otherwise a spontaneous remission over a long period is unlikely to occur.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree