9 Small Vessel Disease
9.1 ABRA/Amyloid Spectrum
9.1.1 Clinical Case
A 67-year-old male with memory impairment and encephalopathy.
9.1.2 Description of Imaging Findings and Diagnosis
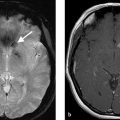
Infiltrative mass in the left temporal lobe with faint leptomeningeal enhancement. Multifocal bilateral T2* white matter and gray matter hypointense lesions consistent with microhemorrhage. Biopsy revealed a diagnosis of amyloid-beta related angiitis (ABRA) (Fig. 9.1).
9.1.3 Background
Amyloid angiopathy is a relatively common cause of lobar hemorrhage in the elderly population. It is the result of deposition of amyloid in the media and adventitia of cortical and leptomeningeal vessels. This process results in vascular fragility and resultant multicompartimental, predominantly lobar hemorrhage. Screening studies using SWI and GRE imaging have found that up to 15% of asymptomatic elderly patients have imaging findings compatible with amyloid angiopathy. It is found in up to 50% of patients over the age of 90 on autopsy. Approximately 90% of the Alzheimer population have amyloid angiopathy. There is no association between amyloid angiopathy and systemic amyloidosis.
Among patients with amyloid angiopathy is a subset of patients with an inflammatory response to amyloid deposition. ABRA is characterized as a transmural granulomatous inflammatory vasculitis that is angiodestructive. CAA-related inflammation (CAA-RI) is characterized by an inflammatory reaction surrounding CAA-affected vessels without angiodestruction. Both ABRA and CAA-RI are treated with immunosuppressive agents including steroids and cyclophosphamide while CAA is not. Thus, the importance of making the distinction between these entities.
9.1.4 Imaging Findings
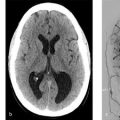
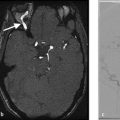
Typical findings in cerebral amyloid angiopathy include superficial lobar hemorrhages, multiple microhemorrhages seen on T2*-weighted imaging primarily located in the gray-white junction of the cerebrum and cerebellum, convexal subarachnoid, or subpial hemorrhage seen on CT, FLAIR (fluid attenuation inversion recovery), or T2*-weighted imaging, cortical superficial siderosis located supratentorially, and leukoaraosis without involvement of the subcortical U fibers (Fig. 9.2 and Fig. 9.3). Hemorrhagic lesions in CAA can be unilateral or bilateral, cerebral or cerebellar, and single or multiple. Lobar hemorrhage is the most common imaging finding seen in 60% of patients and has a sensitivity and specificity of 63 and 93% in distinguishing it from CAA-RI and ABRA. Occasionally, CAA can present as an infiltrative mass-like process resembling a glioma, but the presence of peripheral microhemorrhages at the gray-white junction should lead one to consider a diagnosis of CAA ( Fig. 9.1 and Fig. 9.2 ).
ABRA and CAA-RI have very similar imaging manifestations and are nearly impossible to distinguish from one another on imaging. Typical findings in ABRA and CAA-RI include leptomeningeal enhancement with infiltrative white matter abnormalities, which can occasionally mimic a low-grade glioma ( Fig. 9.1 ). Lobar hemorrhage is rare. Both of these entities commonly present with subcortical and cortical microhemorrhages on SWI, which is key to distinguishing them from neoplasms and other vasculopathies. The sensitivity and specificity of leptomeningeal enhancement in identifying CAA-RI and ABRA are 70 and 93%, respectively ( Fig. 9.1 ). The identification of leptomeningeal enhancement is essential in guiding biopsies as well.



9.1.5 What the Clinician Needs to Know
The presence of lobar hemorrhage(s) in setting of multiple microhemorrhages on SWI is highly suggestive of CAA.
Leptomeningeal enhancement along with cortical/subcortical microhemorrhages should prompt a diagnosis of CAA-RI or ABRA. The leptomeninges should be biopsied in these cases.
Serial imaging is helpful in determining whether therapeutic agents are achieving their desired effect, especially in CAA-RI and ABRA.
9.1.6 High-yield Facts
Diffuse lobar vasogenic edema or mass-like nonenhancing white matter T2 hyperintensities may mimic low-grade glioma, but the presence of microhemorrhage on SWI should suggest CAA-RI or ABRA, which should prompt the radiologist to contact the treating neurologist about the possibility of these entities and their excellent response to steroids.
Lobar hemorrhage has a high sensitivity and specificity in distinguishing CAA from CAA-RI/ABRA.
Leptomeningeal enhancement has a high sensitivity and specificity in distinguishing CAA-RI/ABRA from CAA. While the latter does not respond to steroids, the former two entities show a dramatic and rapid improvement.
Further Reading
[1] Salvarani C, Hunder GG, Morris JM, Brown RD , Jr, Christianson T, Giannini C. Aβ-related angiitis: comparison with CAA without inflammation and primary CNS vasculitis. Neurology. 2013; 81(18):1596–1603 [2] Salvaranti C, Morris JM, Giannini C, Brown RD, Christianson T, Hunder GG. Imaging Findings of Cerebral Amyloid Angiopathy, AB-Related Angiitis (ABRA) and Cerebral Amyloid Angiopathy-Related Inflammation: A Single-Institution 25-Year Experience. Baltimore Medicine. 2016; 95:1–79.2 Susac’s Syndrome
9.2.1 Clinical Case
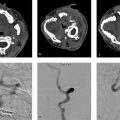
A 45-year-old female with encephalopathy, sensorineural hearing loss, and vision loss ( Fig. 9.4 ).

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree