Abstract
Rare vascular abnormalities of the central nervous system, spinal intramedullary cavernomas make up fewer than 5% of all spinal cord lesions. Symptoms are vague, making diagnosis difficult. A fast and precise diagnosis is made possible by the early detection and characterization of these lesions, which is made possible by radiological imaging, especially MRI with contrast. A 45-year-old man who had intermittent neck discomfort and developed upper limb weakness also had motor and sensory difficulty. Diagnosis of a spinal canal intramedullary cavernoma was confirmed by an magnetic resonance imaging (MRI) showing a distinct intramedullary lesion. This case report focuses on managerial factors and diagnostic problems.
Introduction
The rare spinal cord lesion known as spinal cord cavernous malformation (SCCM) accounts for around 1% of intramedullary lesions in children and 5% of intramedullary lesions in adults. The appearance of larger channels free of glial or neuronal tissue is a characteristic of these vascular abnormalities. The symptoms of SCCM can range from asymptomatic to progressive myelopathy, and magnetic resonance imaging (MRI) is the most effective diagnostic technique [ ].
Clusters of dilated capillaries with thin walls that are prone to recurrent microhaemorrhages are called cavernomas, or cavernous malformations [ ]. Due to their rarity and nonspecific symptoms, spinal intramedullary cavernomas often go undiagnosed until patients present with significant neurological deficits. Their unpredictable clinical course and potential for causing substantial morbidity highlight the need for timely diagnosis and management.
Among the many clinical features that spinal cavernomas can produce are progressing myelopathy and incidental observations. Mass effects, recurring microhaemorrhages, or spinal cord edema are frequently the cause of these symptoms, which might result in neurological decline, sensory abnormalities, or motor impairments. These symptoms are more likely to occur in the cervical area.
Case presentation
A 45-year-old male residing in South East Asia presented to our outpatient department with complaints of progressive weakness in his upper limbs and intermittent neck pain over 6 months. Initial assessment in the orthopedics outpatient department focused on musculoskeletal causes, given the nature of his complaints. On further physical examination, the patient exhibited normal cranial nerve function, no signs of cerebellar dysfunction and intact lower limb coordination. However, persistent neurological symptoms prompted a referral to neurology.
Neurological examination revealed: Weakness (4/5) in bilateral upper limb muscles. Decreased pinprick and temperature sensation in a cape-like distribution over the shoulders and exaggerated deep tendon reflexes in the upper limbs. Following the physical examination, laboratory investigations, including complete blood count, metabolic panel and inflammatory markers were requested, all of which were within normal limits. Given the clinical presentation, magnetic resonance imaging (MRI) of the cervical spine was performed for further evaluation.
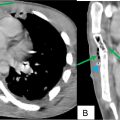
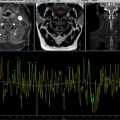
Non contrast MRI cervical spine findings: Focal T1/T2/T2FSWI hypointense popcorn-like rim lesion in the intramedullary region of the cervical cord at the level of the C2 vertebra, measuring approximately 5 × 6 × 7 mm (anteroposterior X transverse X craniocaudal) with surrounding mild edema ( Figs. 1 A and B). It shows blooming on GRE ( Figs. 1 F). There is e/o intramedullary peripheral ring hypointensity on T1/T2WI with peripheral blooming on GRE s/o peripheral chronic haemorrhage with T1 hyperintensity, T2 hypointensity and peripheral blooming on GRE in centre s/o acute haemorrhage it is extending from C1 to C4 vertebrae level s/o hematomyelia ( Figs. 1 G-I).

Post contrast MRI cervical spine findings: No significant enhancement on postcontrast study ( Fig. 2 ). Magnetic resonance spectroscopy (MRS) did not show any significant metabolic peak, making malignancy unlikely ( Fig. 3 ). These imaging features were highly suggestive of a spinal cord cavernoma with associated hematomyelia.