Abstract
Spontaneous hemopneumothorax is a rare but potentially life-threatening condition requiring urgent intervention. We report the case of a 58-year-old male who presented with acute right-sided chest pain, dyspnea, and hemodynamic instability without a history of trauma. Imaging confirmed a tension hemopneumothorax, which was initially managed with chest tube placement, leading to stabilization and partial lung re-expansion. However, persistent air leaks and incomplete re-expansion necessitated further intervention, including the placement of a second chest tube and transfer for video-assisted thoracoscopic surgery. This case highlights the importance of prompt diagnosis and a multidisciplinary approach to managing spontaneous hemopneumothorax to prevent life-threatening complications.
Introduction
Spontaneous hemopneumothorax (SHP) is a rare but potentially life-threatening condition characterized by the accumulation of air and blood within the pleural space without any preceding trauma [ ]. It can result from various underlying pathologies and presents with a spectrum of symptoms, ranging from mild dyspnea to severe respiratory distress [ ]. The complexity of this condition arises from its varied presentations and the need for prompt intervention to prevent complications such as respiratory failure or shock [ ]. Although no specific guidelines exist for managing SHP, the literature remains divided on patient selection for surgery, with recent trends indicating a growing preference for early surgical intervention. This case report aims to provide insight into the clinical presentation, diagnostic approach, and initial conservative management of SHP, followed by surgical intervention.
Case presentation
This 58-year-old male with a 45-pack-year smoking history arrived at the emergency department (ED) via advanced life support (ALS) with a 1-day history of progressively worsening right-sided chest pain, culminating in a syncopal episode. The patient reported exerting himself the day prior, having pushed his car out of the garage but denied any trauma. He has no known drug allergies and does not take regular medications, except for occasional ibuprofen, about once a month. His surgical history includes appendectomy and open reduction and internal fixation of the right femur. He does not see a primary care physician regularly.
Upon initial evaluation in the ED, he was in significant respiratory distress, complaining of dyspnea and chest pain. Vital signs were as follows: BP 75/51 mmHg, HR 131 bpm, RR 20, SpO2 96% on room air, and T 36°C. Physical examination showed he was alert and oriented x4, tachycardic without murmur, and demonstrated increased work of breathing. Lung auscultation revealed decreased breath sounds on the right, but the rest of the exam was normal.
A bedside ultrasound showed moderate-to-large right-sided pleural effusion and absent lung sliding in the anterior thorax. Initial resuscitation with IV fluids was initiated, and the patient underwent a computed tomography (CT) angiogram of the chest, which revealed a right-sided hemopneumothorax with a significant mediastinal shift to the left, indicative of tension pneumothorax ( Figs. 1 and 2 ).


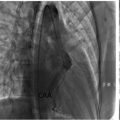
No evidence of pulmonary embolism or aortic dissection was found. An emergent chest tube was placed on the right side, draining both air and approximately 1L of pleural fluid, which appeared to be blood. This led to hemodynamic stabilization and re-expansion of the right lung, with minimal pleural effusion and improved mediastinal shift, as confirmed by chest x-ray (CXR) ( Fig. 3 ).

The laboratory results were notable for mild leukocytosis (WBC 11 × 10⁹/L [normal: 4.0-10.0 × 10⁹/L]) and anemia, with an initial hemoglobin level of 7.9 g/dL [normal: 13.0-17.0 g/dL]. The pleural fluid analysis from the initial drainage showed a hematocrit of 32%, exceeding 50% of that in the peripheral blood. The patient was transferred to the intensive care unit (ICU) for close monitoring. A total of 1650 cc of blood was drained over 48 hours following the chest tube insertion. An additional unit of packed red blood cells (PRBCs) was transfused, and no further signs of hemodynamic instability were observed during hospitalization. Additional bloodwork, including blood, respiratory, and pleural fluid cultures, showed no growth; respiratory viral panel (RVP) testing, procalcitonin levels, and polymerase chain reaction (PCR) testing for Methicillin-Resistant Staphylococcus Aureus (MRSA), as well as urine tests for Legionella and Streptococcus pneumoniae, were all negative. Despite the initial chest tube placement, the patient’s hemopneumothorax persisted, raising concerns about ongoing air leaks and incomplete lung re-expansion.
Following a repeat CT scan confirming a persistent moderate right-sided hemopneumothorax with right lower lobe consolidation ( Fig. 4 ), a second chest tube was inserted anteriorly on the right side, resulting in an effective reduction of the pneumothorax ( Fig. 5 ).