Abstract
Pineal astrocytoma is an uncommon central nervous system tumor, presenting diagnostic and therapeutic challenges due to its deep-seated location and nonspecific clinical features. This case report describes a 37-year-old female who presented with altered sensorium, persistent headache, and projectile vomiting for 20 days. Initial examination revealed stable vitals and a reduced Glasgow Coma Scale score, necessitating immediate intubation. Magnetic resonance imaging (MRI) of the brain revealed a solid-cystic lesion in the pineal region with intraventricular extension, mass effect on the midbrain, and hemorrhagic changes. Magnetic resonance spectroscopy (MRS) findings, including elevated choline and lipid peaks with reduced N-acetyl aspartate, suggested a neoplastic etiology. The patient underwent a suboccipital craniotomy via a supracerebellar infratentorial approach for partial tumor excision. Histopathological analysis confirmed the lesion as a grade IV astrocytoma. Postoperative recovery was stable, and further management with adjuvant radiotherapy and chemotherapy was planned due to the high-grade nature of the tumor. This case highlights the importance of integrating clinical findings, advanced imaging techniques, and histopathological evaluation to accurately diagnose and manage rare pineal region tumors. Despite surgical intervention, the prognosis for high-grade astrocytomas remains poor, underscoring the necessity for continued research into targeted therapies and novel treatment approaches.
Background
Astrocytomas are primary central nervous system (CNS) tumors that originate from astrocytes, the supportive glial cells in the brain and spinal cord [ ]. These tumors encompass a wide spectrum of histological grades as classified by the World Health Organization (WHO), ranging from benign grade I astrocytomas to highly malignant grade IV glioblastomas. Pineal region astrocytomas represent a rare subset of these tumors, accounting for only a small fraction of intracranial neoplasms [ ]. Their rarity and clinical overlap with other pineal region tumors, such as pineoblastomas, germinomas, and other germ cell tumors, make their diagnosis and management particularly challenging [ ]. Patients with pineal region astrocytomas are typically present with nonspecific symptoms resulting from mass effect or obstructive hydrocephalus caused by tumor growth and intraventricular extension. Common clinical manifestations include headache, nausea, projectile vomiting, and altered mental status due to increased intracranial pressure [ ]. Compression of surrounding structures, such as the midbrain and cerebral aqueduct, may lead to additional neurological deficits, including Parinaud’s syndrome, characterized by upward gaze palsy and convergence-retraction nystagmus [ ].
Advancements in neuroimaging have significantly improved the diagnostic approach to pineal region tumors. Magnetic resonance imaging (MRI) is the modality of choice, offering detailed anatomical and pathological insights. MRI sequences, such as diffusion-weighted imaging (DWI) and gradient echo (GRE), help identify tumor components, including cystic changes, hemorrhage, and necrosis [ ]. Magnetic resonance spectroscopy (MRS) provides metabolic information, such as elevated choline peaks and reduced N-acetylaspartate (NAA), aiding in distinguishing neoplastic from non-neoplastic lesions [ ]. Management of pineal region astrocytomas is multidisciplinary, with surgical intervention playing a pivotal role. Due to the deep location and proximity to critical neurovascular structures, approaches such as suboccipital craniotomy with a supracerebellar infratentorial route are commonly employed [ ]. The primary aim is tissue sampling for histopathological diagnosis and, where feasible, maximal safe resection. Histological evaluation remains the gold standard for confirming the tumor type and grade, which is critical for guiding further management [ ].
High-grade astrocytomas, such as glioblastomas (grade IV), pose significant therapeutic challenges. Despite surgical resection and adjuvant therapies, including radiotherapy and chemotherapy with temozolomide, the prognosis remains dismal. The median survival for patients with grade IV astrocytomas is approximately 12-15 months [ ]. Current research is focused on exploring targeted therapies, molecular inhibitors, and immunotherapies to improve outcomes for patients with aggressive CNS tumors [ ]. This case highlights the importance of recognizing the clinical presentation of rare pineal astrocytomas and utilizing advanced imaging and surgical techniques to manage these complex cases effectively. Further research is needed to develop innovative therapeutic strategies to address the unmet needs in treating high-grade astrocytomas.
Case presentation
A 37-year-old female presented to the emergency department with altered sensorium and significantly reduced responsiveness. Her family reported a 20-day history of persistent headaches and episodes of projectile vomiting, which were nonbloody. There was no history of fever, trauma, weakness, or any systemic illnesses, including hypertension, diabetes mellitus, tuberculosis, or bronchial asthma. The patient had no prior surgical history or known comorbidities.
On arrival, the patient’s Glasgow Coma Scale (GCS) score was markedly reduced, necessitating intubation for airway protection. Her vital signs were stable, with a blood pressure of 138/90 mmHg, a pulse rate of 110 beats per minute, and an oxygen saturation of 99% on room air. Pupillary responses to light were intact, and there was movement in all 4 limbs. Systemic examinations of the cardiovascular, respiratory, and gastrointestinal systems revealed no significant abnormalities.
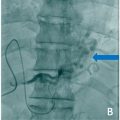
Given the altered sensorium, the patient was referred to the radiology department for neuroimaging. Magnetic resonance imaging (MRI) of the brain demonstrated a solid-cystic lesion in the pineal region, measuring approximately 4 × 2.8 × 4.4 cm. The lesion appeared hypointense on T1-weighted images and heterogeneously hyperintense on T2-weighted and FLAIR sequences. Diffusion-weighted imaging (DWI) showed restricted diffusion, and postcontrast studies revealed heterogeneous enhancement of the lesion Figs. 1 and 2 . A large area of blooming was observed on gradient echo (GRE) sequences, indicative of hemorrhage within the tumor. The lesion extended intraventricularly into the third and fourth ventricles, as well as into the occipital horns of the lateral ventricles bilaterally, causing mass effect and compression of the midbrain. Magnetic resonance spectroscopy (MRS) demonstrated an elevated choline peak and lipid peak with reduced N-acetyl aspartate (NAA), consistent with a neoplastic etiology, likely pineoblastoma with hemorrhage Figs. 3 and 4 .