Abstract
Early recognition and characterization of soft tissue tumors is important for proper fetal and maternal care. Here, we present sonographic, fetal and postnatal MRI, and pathological findings of a rare case of congenital NTRK-rearranged malignant spindle cell sarcoma with TPM3-NTRK1 fusion in a male fetus.
Introduction
NTRK-rearranged spindle cell sarcomas are a rare and aggressive type of soft-tissue sarcoma with an infiltrative growth pattern. This tumor primarily affects children and young adults, favoring the extremities [ ]. This rapidly growing cancer can damage organs during development due to mass effect and direct invasion in a growing fetus and potentially cause dangerous hemorrhage during birth.
Case report
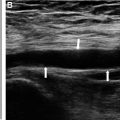
A 25-year-old healthy G2P1001 female presented at 34 weeks gestational age with growth restriction of a male fetus. The pregnancy was previously uncomplicated. There was no family history of congenital malformations, birth defects, chromosomal abnormalities, or learning disabilities. Use of tobacco, alcohol, and illicit drugs during the pregnancy was denied. Maternal labs were normal throughout pregnancy. NIPS genetic screening was declined. At the mother’s 34 week prenatal visit, the abdominal circumference was measured and corresponded to the 1.9% percentile, consistent with fetal growth restriction. This finding prompted a detailed fetal evaluation. Prenatal ultrasound ( Fig. 1 ) showed an exophytic, complex, vascular mass abutting the sacrum with a presumed diagnosis of sacrococcygeal teratoma (SCT) given its location. For further characterization, a fetal MRI was performed at 35 weeks gestation, which showed a heterogeneously enhancing, solid, exophytic pelvic/perineal mass abutting the sacrum ( Fig. 2 ). Many features of the tumor were atypical for a sacrococcygeal teratoma. The mass was more homogenous than expected for a SCT, lacked cystic components that would normally been seen in a SCT, and involved the thigh but without definite involvement of the spine. It was also noted that the rectum was displaced posteriorly by the mass. At that time, alternative differential diagnoses were suggested: fibrosarcoma, rhabdomyosarcoma, myofibroma, and less likely atypical sacrococcygeal teratoma.


The baby was delivered via C-section at 37 weeks and 1 day gestation due to fetal distress. The large left pelvic mass was evident ( Fig. 3 ). A postnatal MRI showed a large, exophytic, heterogeneously enhancing perineal/pelvic mass with infiltrative pattern that encircled the rectum with extension into the left gluteal and inguinal regions ( Fig. 4 ). The mass was isointense to skeletal muscle on T1WI, hyperintense on fluid sensitive sequences, and demonstrated heterogeneous enhancement. The tumor demonstrated mass effect on multiple structures: deviating and tethering of the rectum to the right and stretching it inferiorly; displacing the anus posteriorly; uplifting the bladder; and abutting the base of the penis with no clear fat planes. Lack of spine involvement was confirmed.



Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree