Abstract
Spinal dysraphisms (SDs) are characterized by a heterogeneous range of congenital spinal anomalies that arise from derivative disturbances in neural tube development. Closed spinal dysraphism, a variant, is less common and typically has a subtle clinical presentation. Timely and correct diagnosis is essential to avert chronic complications. We describe a 12-year-old boy who presented with progressively worsening bladder and bowel incontinence since early childhood. On clinical examination, he was found to have swelling of the sacral region, gross motor impairment, and a slim physique. MRI showed hydro/syringomyelia, tethered cord, lipomeningocele, spina bifida in the sacral region, chronic cystitis and dural ectasia. These test results were consistent with the diagnosis of closed spinal dysraphism. This case highlights the need to consider urinary incontinence and sacral anomalies as manifestations of closed spinal dysraphism. Neuroimaging plays a key role in diagnosis, and especially MRI is the gold standard in detecting detailed structural abnormalities. To improve patient outcomes and quality of life, this paper emphasizes the intricacy of closed spinal dysraphism and the necessity of multidisciplinary management and early intervention.
Introduction
Spinal dysraphisms (SDs) are a collection of disorders of the spinal cord and the spine and are classified as congenital disabilities. These include various kinds of malformations of the spinal cord, which are due to the failure of mesenchymal, bony, and neural tissue to close along the midline. These defects take place during the period of 2-6 weeks of embryonic life [ ]. SDs, part of a category of neural tube defects, occur at a population frequency of somewhere between 1 and 3 in every 1000 live births [ ]. Burmese children with spinal malformations resulting from disruptions of secondary neurulation also tend to have anorectal or urogenital defects, reflecting the fact that the cloaca is in close embryological scanty with the caudal mass that later develops into the lumbosacral region [ , ]. Also, these children often have upper gastrointestinal or respiratory tract malformations because the notochord is involved in the development of the neural tube and the thoracoabdominal viscera [ ]. Radiological imaging, in conjunction with the appropriate history and clinical findings, is crucial in confirming the diagnosis of SDs and therefore requires complex knowledge of the embryology of the spinal cord. MRI has evolved over time and remains as a noninvasive tool at hand for diagnosis of SDs [ ]. Here under we present a case of an adolescent boy with bladder- bowel incontinence who came to our centre for further evaluation.
Case report
A 12-year-old boy was referred for evaluation of progressively worsening loss of bladder and bowel control. His evacuations had been spontaneous since childhood, and there had been no prior history of retention. His past obstetric history was significant for an FTND (full-term normal delivery) with a 3.5 kg birth weight without NICU admission. On physical examination, a 2 × 2 cm swelling was observed in the lower back.
The swelling on the patient’s lower back has increased in size, now measuring 3 × 3 cm. During physical examination, the patient was noted to have a lean build, with a weight of 40 kg and a height of 145 cm, resulting in a BMI of 18, which is on the lower end of the normal range (18.5-24.9). The patient was unable to walk properly, exhibiting a limp in the left leg, indicating gross motor impairment. However, fine motor milestones for the hands were normal, and language and social milestones were achieved up until age, though the patient exhibited slow and hesitant responses. The patient is not currently enrolled in school due to issues with bowel and bladder incontinence.
On general physical examination (GPE), the patient’s heart rate (HR), blood pressure (BP), respiratory rate, and temperature were all within normal limits. The patient was oriented to time, place, and person, and was able to answer general questions and perform simple tasks with their hands. On abdominal examination, there was tenderness in the lower abdomen. On local examination of the back, a well-defined swelling was noted over the lower sacral region, covered with skin. The swelling was nonmobile, soft to touch, and mildly tender, with an approximate size of 2 × 2 cm.
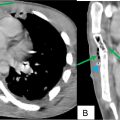
On MRI, there is a long segment intramedullary, multiseptated, T2 hyperintensity seen in the cervico-thoracic and lumbar cord measuring 37.4 cm from the mid body of C2 to upper-end plate of L3 vertebra, with spinal cord expansion and effacement of anterior and posterior subarachnoid space in the cervical and dorsal parts, with a maximum diameter of 12.3 mm at C5-C6 disc level suggestive of hydro/ syringomyelia ( Fig. 1 ).

In these images also we can see that the multiseptated syringomyelia extends all the way up to the lower endplate of L3 where the conus medullaris is ending, and the filum terminal appears attached to the posterior part of the dural sac suggestive of tethered cord. There is no evidence of tonsillar herniation, ruling out Chiari malformation and the visualized sagittal sections of the brain appeared normal ( Fig. 1 ).
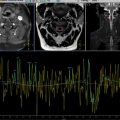
In the coronal sections of the sacrum, there is asymmetry of the sacrum with the right end being normal while the left end shows some defect in the lower part ( Fig. 2 ). There was also high signal fluid containing large bowel on the left side.


Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree