Abstract
Intussusception is a common cause of bowel obstruction in children, typically occurring in those under 3 years old and often idiopathic. Secondary intussusception is less common in pediatric patients and usually involves a pathological lead point. Appendiceal intussusception is rare, occurring in only 0.01% of appendectomy specimens, and can mimic other acute abdominal conditions, making preoperative diagnosis challenging. We report a case of a 7-year-old male who presented with a 3-day history of crampy right lower quadrant pain and nonbilious vomiting. Ultrasound revealed an ileocolic intussusception with a suspected pathological lead point. Further imaging identified a distended, non-compressible appendix within the intussusceptum, leading to a diagnosis of secondary ileocolic intussusception due to acute appendicitis. Hydrostatic reduction was initially successful, but the patient developed recurrent intussusception within 24 hours. Surgical exploration confirmed McSwain type 3 appendiceal intussusception, necessitating manual reduction and appendectomy. The patient recovered well postoperatively. Clinicians should maintain a high index of suspicion for appendiceal pathology in older children with intussusception, and thorough imaging evaluation is essential. Early recognition of an inflamed appendix as the lead point is critical to prompt appropriate surgical intervention, ultimately preventing further complications. This case contributes to clinical practice by emphasizing the need for tailored diagnostic and therapeutic strategies in managing rare, complex presentations of intussusception.
Introduction
Intussusception is one of the most common causes of acute abdominal pain in children. It occurs mostly in those under 3 years of age, with the highest incidence between 5 and 10 months old [ ]. It occurs when a segment of the bowel (the intussusceptum) telescopes into an adjacent segment (the intussuscipien), leading to bowel obstruction, ischemia, and potential perforation if left untreated [ ]. The condition is idiopathic in approximately 90% of pediatric cases, often attributed to lymphoid hyperplasia in the terminal ileum acting as a lead point [ ]. However, in older children and adults, secondary intussusception is more common and is usually caused by a pathological lead point. Common lead points include Meckel’s diverticulum, polyps, and lymphoid hyperplasia. Rarely, appendiceal pathology can also act as a lead point [ ].
Appendiceal intussusception is an exceptionally uncommon condition, with an estimated incidence of 0.01% among patients undergoing appendectomy [ ]. It involves the appendix invaginating into the cecum, which can mimic various acute and chronic abdominal disorders, rendering preoperative diagnosis challenging [ , ].
Here, we present a case of ileocolic and appendiceal intussusception in a child, with acute appendicitis as the pathological lead point.
Case presentation
A 7-year-old male presented with a 3-day history of crampy right lower quadrant abdominal pain and nonbilious vomiting. Over the first 2 days, his pain was intermittent and relatively mild, but it progressively worsened by the third day, prompting his family to seek medical care. On arrival, his vital signs were as follows: temperature 37.5°C, heart rate 110 beats per minute, respiratory rate 20 breaths per minute, and blood pressure 102/68 mmHg. Physical examination revealed localized tenderness in the right lower quadrant.
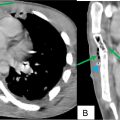
Laboratory tests showed a normal white blood cell count (WBC) with a left shift. C-reactive protein (CRP) was mildly elevated at 12 mg/L, while procalcitonin was unavailable. An abdominal ultrasound performed on presentation identified an ileocolic intussusception in the subhepatic region, characterized by a target sign ( Fig. 1 ). Due to the patient’s atypical age for idiopathic intussusception, a lead point was suspected. Further imaging revealed a distended, noncompressible appendix invaginating into the cecum as part of the intussusceptum, alongside the terminal ileum ( Figs. 2 A and B). This led to a diagnosis of secondary ileocolic intussusception with acute appendicitis as the lead point.


Later that same day, the surgical team initially attributed appendiceal edema to entrapment within the intussusception and opted for hydrostatic reduction, which was successful. A postreduction ultrasound demonstrated persistent dilatation and noncompressibility of the appendix, but the patient showed no immediate complications at that time.
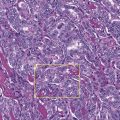
The following day, the patient returned with recurrent abdominal pain, and repeat ultrasound confirmed recurrent ileocolic intussusception, again involving the inflamed appendix. Surgical exploration was undertaken, revealing both an inflamed, distended appendix and ileocolic intussusception. The appendix was found invaginating into the cecum, consistent with McSwain type 3 appendiceal intussusception ( Fig. 3 ). Manual reduction of both the ileocolic and appendiceal intussusceptions was performed, followed by appendectomy. The patient recovered well postoperatively.