EMBRYOLOGY
Bowel Development
- •
Gastrointestinal (GI) tract forms from 1 straight tube
- ○
Foregut : Forms esophagus, stomach, and duodenum
- ○
Midgut : Small intestine and colon up to splenic flexure
- –
Connected to yolk sac
- –
Portion that lengthens and loops around superior mesenteric artery (SMA)
- –
- ○
Hindgut : Descending colon, sigmoid, rectum, and upper anal canal
- –
Caudal end of hindgut terminates in cloaca
- □
Cloaca (Latin for sewer) is common chamber with early communication between the urinary, GI, and reproductive tracts
- □
- –
- ○
- •
Physiologic herniation
- ○
Length of midgut increases rapidly and is greater than body can accommodate so it herniates into base of umbilical cord
- ○
It rotates 90°counterclockwise around axis of SMA and returns to the abdomen after total rotation of 270°
- ○
Abdominal wall closes around base of cord (umbilical ring)
- ○
Physiologic hernia is commonly seen on early 1st trimester scans but the bowel should be back within the abdomen by 12 weeks gestational age
- ○
An omphalocele results from failure to complete physiologic herniation or close umbilical ring
- ○
- •
Rectum forms when urorectal septum divides cloaca into rectum posteriorly and urogenital sinus anteriorly
- ○
Cloacal membrane ruptures by beginning of 8th week, creating anal opening
- ○
Urogenital sinus will divide to form bladder and in females, the vagina
- ○
SCANNING APPROACH AND IMAGING ISSUES
Techniques and Sonographic Appearance
- •
American Institute of Ultrasound in Medicine (AIUM) scan of the abdomen requires documentation of stomach, kidneys, bladder, umbilical cord insertion site, and umbilical cord vessel number
- ○
Diaphragm, esophagus, small intestine, colon, gallbladder, and liver should also be examined but is not required as part of the standard midtrimester scan
- ○
- •
Stomach is seen as a fluid-filled structure in the left upper quadrant and is one of the 1st organs identified
- ○
Document heart and stomach are on same side, and it is anatomic left of fetus (normal situs)
- –
Opposite sides are seen in heterotaxy syndromes
- –
- ○
Changes in size and shape during exam
- ○
Fluid may intermittently be seen to enter the duodenal bulb but should never persist
- –
A persistently dilated duodenum is never normal and suspicious for duodenal atresia
- –
- ○
- •
Fluid must be visualized on both sides of the umbilical cordinsertion in a transverse section of the fetal abdomen
- ○
Stimulation of fetal movement may be necessary to create a more favorable acoustic window, especially in 3rd trimester when the fetal knees are often tucked up against abdominal wall
- ○
- •
Normal cord contains 2 arteries and 1 vein
- ○
May be visible at cord insertion site, but easiest way to confirm is color Doppler showing umbilical arteries on either side of bladder
- ○
- •
Diaphragm appears as a thin, arched, hypoechoic band
- ○
It is imperative that it be completely imaged from front to back, which is best done in the sagittal plane
- ○
If viewed only in the anterior coronal plane, a congenital diaphragmatic hernia (CDH) may be missed
- ○
- •
Esophagus is not normally seen on fetal imaging, but a blind-ending, fluid-filled pouch may be seen in the fetal neck in esophageal atresia
- ○
Use color Doppler to ensure that the fluid-filled structure is between the neck vessels
- ○
- •
Bowel
- ○
In early 2nd trimester, often appears as intermediate echogenicity “filler” between the solid organs, bladder, and stomach; higher frequency transducers may show distinct bowel loops
- ○
Normal meconium-filled colon often prominent near term
- ○
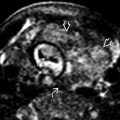
Anal dimple best seen on an axial view of perineum
- –
Anal mucosa is echogenic and surrounded by hypoechoic muscles of the anal sphincter, creating a target or doughnut appearance
- –
- ○
- •
Fetal liver is relatively large and extends across the upper abdomen with the left lobe anterior to stomach
- ○
Major contributor to the abdominal circumference (AC)
- ○
Both portal and hepatic veins seen on color Doppler
- ○
Gallbladder may be seen, especially in the 3rd trimester, and should not be confused with an abdominal cyst
- ○
Approach to the Abdominal Wall
- •
Is the abdominal wall intact?
- ○
Gastroschisis (most common abdominal wall defect) is generally located to the right of the umbilical cord insertion and is not covered by a membrane
- –
Small bowel is the most commonly extruded organ, although stomach, large bowel, and other structures may also be involved
- –
- ○
Omphalocele involves extrusion of bowel into the base of the umbilical cord
- –
Covered by a membrane; umbilical cord inserts on this membrane
- –
May rarely rupture; in these cases, it may be difficult to distinguish from gastroschisis
- –
- ○
Defects may also occur in more unusual locations
- –
Low, suprapubic mass may be associated with bladder or cloacal exstrophy
- □
Both will have absent bladder, but cloacal exstrophy will also have extruded bowel described as appearing like an elephant trunk
- □
- –
Supraumbilical defect associated with diaphragmatic and cardiac abnormality is seen in pentalogy of Cantrell
- –
Other unusual or bizarre abdominal wall defects may be seen in cases of amniotic bands or body stalk anomaly
- –
- ○
- •
Is the fetus freely mobile?
- ○
In body stalk anomaly , the fetus is “stuck” to the placenta, and the umbilical cord is absent or very short
- ○
A fetus entrapped within amniotic bands may also be tethered in one position
- –
Look for strands of membrane or other defects, such as unusual facial or cranial clefts
- –
- ○
Approach to the Gastrointestinal Tract
- •
Is the abdomen normal in size?
- ○
Per AIUM guidelines, the AC is measured at the skin line on a true transverse view at the level of the junction of the umbilical vein, portal sinus, and fetal stomach
- ○
AC is utilized with other biometric parameters to calculate the fetal weight/average gestational age
- ○
AC below the normal range
- –
Generally, the most affected parameter in growth restriction
- –
May also measure small when normal abdominal contents are outside the abdomen (e.g., gastroschisis, omphalocele) or up in the chest (i.e., CDH)
- –
- ○
AC above the normal range
- –
Macrosomic fetus of a diabetic mother
- –
Overgrowth syndromes, such as Beckwith-Wiedemann, may also exhibit increased AC size, primarily due to enlarged kidneys and liver
- –
AC often increased in fetuses with large abdominal masses, dilated bowel, or distended bladder
- –
- ○
- •
Is the stomach normal?
- ○
A fluid-filled stomach should reliably be identified after 14 weeks
- –
If not seen, short-term follow-up required to confirm its presence or absence
- –
Ensure that it is not in an abnormal location, such as within the chest in a CDH
- –
- ○
Small/absent stomach
- –
Esophageal atresia ± tracheoesophageal fistula
- □
Look for blind-ending pouch in neck
- □
Will have significant polyhydramnios by 3rd trimester
- □
- –
May be seen in cases of decreased swallowing (e.g., neurologic disorder)
- –
- ○
Large stomach
- –
Often a transient finding or may be seen in evolving, distal GI obstructions
- –
Double bubble sign (dilated stomach and duodenum) is seen in duodenal atresia
- –
- ○
- •
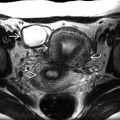
Is there an abdominal mass?
- ○
Masses should be characterized as to their location and appearance (cystic, solid, or complex; vascular or nonvascular) to narrow the differential diagnosis
- ○
Cystic masses in the abdomen are relatively common
- –
Many of these are related to the urinary tract and include cystic kidneys, lower urinary tract obstruction, and ovarian cysts
- –
GI causes include
- □
Bowel atresia : Look for peristalsis
- □
Meconium pseudocyst : Irregular cystic mass, which forms after bowel perforation; look for other sequelae, including peritoneal calcifications
- □
Enteric duplication cyst : Look for gut signature
- □
Mesenteric cysts/lymphangioma
- □
Persistent cloaca occurs when genitourinary tract and colon never separate
- □
- –
- ○
Solid masses are less common; the differential diagnosis starts with the organ of origin
- –
The most common liver mass is a congenital hemangioma , which usually has prominent vascularity
- –
Bulk of a sacrococcygeal teratoma is exophytic but may extend into pelvis/abdomen
- □
Rarely may be only intrapelvic with no external component
- □
- –
Fetus-in-fetu is a mixed solid/cystic mass and is often quite large
- □
Calcifications common; bones and vertebrae may be seen
- □
- –
- ○
- •
Are there calcifications in the abdomen?
- ○
Calcifications on the surface of the liver are actually in the peritoneum
- –
These correlate strongly with intrauterine bowel perforation
- –
Look for associated echogenic or dilated bowel loops, small amounts of ascites, &/or meconium pseudocysts to add weight to this diagnosis
- –
- ○
Calcification in the liver parenchyma concerning for infection, most commonly cytomegalovirus
- ○
Calcifications in the bowel lumen indicate admixture of meconium and urine in the setting of abnormal distal bowel and bladder development
- –
These “meconium marbles” roll within the bowel lumen with peristalsis
- –
Look carefully for the anal dimple to detect associated anal atresia
- –
- ○
- •
Does the bowel appear echogenic?
- ○
A high-frequency transducer may give the false impression of echogenic bowel
- –
Confirm the finding is persistent with a lower frequency transducer (< 5 MHz)
- –
- ○
Bowel is not abnormal unless it is as bright as bone
- ○
Fetal ingestion of blood from a recent bleed is a common benign cause and resolves spontaneously
- ○
Evaluate for pathologic causes, including aneuploidy, infection, cystic fibrosis , and early bowel abnormalities, such as atresia , before the bowel becomes dilated
- ○
May be seen in bowel ischemia in association with severe growth and hemodynamic stress as in twin-twin transfusion
- ○
- •
Is there ascites?
- ○
Care should be taken to differentiate true ascites from pseudoascites , a potential pitfall created by the hypoechoic abdominal wall musculature
- ○
Ascites may be 1st sign of impending hydrops
- –
Look for other evidence of hydrops (pleural and pericardial effusions and skin edema)
- –
- ○
Chest masses may compromise venous and lymphatic return and cause isolated ascites without generalized hydrops
- ○
May also result from perforation of an abdominal viscus , either bowel or bladder
- ○
PHYSIOLOGIC HERNIATION