Abstract
This chapter focuses on how radiologists are paid by government (Medicare, Medicaid) and private insurers, the history behind the current payment system, and ideas of how this payment system may be changing in the near future. The importance of accurate coding and billing, the potential value of clinical decision support, and some basic definitions and concepts of billing, collections, and accounting in radiology are discussed.
Keywords
Clinical decision support (CDS), CMS, CPT coding, fee-for-service (FFS), ICD-10, MACRA, Medicare, RBRVS, third-party payers, value-based payment
Dominant Payers in American Healthcare
Most healthcare costs, roughly 72% by current estimates, are paid by third-party payers. Insured patients still have out-of-pocket expenses, for example, to meet copayments and deductibles, depending on the actuarial value of their plan. Approximately 12% of the US population is uninsured, or self-pay ( Fig. 16.1 ).
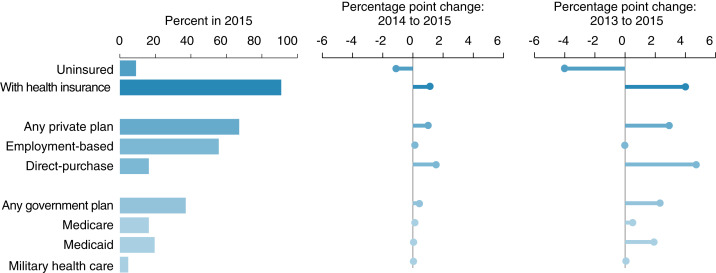
Third-party payers include private insurance, Medicare, and Medicaid. The majority of the funds, roughly 45%, are contributed by several private insurers, followed by Medicare (28%) and Medicaid (21%). However, Medicare is the largest single payer, larger than any single private insurer. This is important because private insurers tend to follow Medicare regarding decisions about which services to cover and, in particular, how much to pay for technology.
Medicare Reimbursement for Imaging
The government-administered Medicare and Medicaid programs were established in 1965 as part of the Social Security Act. These programs are administered by the Centers for Medicare and Medicaid Services (CMS) in the US Department of Health and Human Services.
Medicare reimburses healthcare providers for services deemed “reasonable and necessary for the diagnosis or treatment of illness or injury or to improve the functioning of malformed body member.” The level at which Medicare reimburses providers for imaging services depends on where the imaging is performed. In CMS’s view, there are essentially two settings where imaging services are rendered:
- 1.
Outpatient physician practices/independent facilities
- 2.
Hospitals
Medicare further divides hospital services into inpatient and outpatient services performed in hospitals.
Medicare may pay for imaging prospectively, via capitation, but in general, Medicare reimbursement is mostly rooted in fee-for-service (FFS) payments, which is a specified fee paid for a defined unit of work, such as interpreting a computed tomography (CT) scan. Under FFS, the more units of work that are completed, the greater the reimbursement. This is the basis of the Physician Fee Schedule (PFS), which is how imaging performed in outpatient physician practices/independent facilities is reimbursed.
Evolution of Payment Under Medicare/Medicaid
When it was initially created, Medicare’s FFS payment system set fees according to what was considered a usual, customary and reasonable (UCR) fee. Under the UCR system, physicians’ charges were based on what the billing physician usually charged for a given service (usual), on what was commonly charged by their peers (customary), or anchored to what private insurance paid (reasonable). UCR had many limitations. Under UCR, the charges were arbitrary and varied widely. The prices set had no basis in the supply-demand schema seen in other markets because healthcare, for multiple reasons, is not a free market. For example, proceduralists, such as urologists, received disproportionately higher reimbursements than physicians such as internists, who did nonprocedural/cognitive work.
This all changed in 1992 when a team led by health economist William Hsiao devised a much more granular method for fair reimbursement known as the resource-based relative value scale (RBRVS).
Resource-Based Relative Value Scale
The Omnibus Reconciliation Act of 1989 mandated the use of the RBRVS by 1992, and this system is now the sole means of determining physician payments for all third-party payers. The RBRVS is a granular method of reimbursement used by Medicare, which attempts to compensate physicians fairly for the skill, risk, and unit cost of their work by a scale known as the relative value unit (RVU). The scale is relative—how one service is valued against another—making RBRVS a unified scale for all physician payments for all services across all medical specialties.
The RVU is divided into two components: technical and professional. The final reimbursement is calculated by using a single monetary conversion factor. The professional component, the component related to the physician’s work, has three parts.
- 1.
Physician work
- 2.
Malpractice expense
- 3.
Practice expense
Practice expenses may be direct or indirect. Direct practice expenses include salaries of support staff, cost of disposables, and costs related to durable equipment. Direct practice expenses are determined by both the Relative Value Scale Update Committee (RUC) and CMS. Indirect practice expenses, or overhead, are expenses not directly related to individual patient care. Indirect practice expenses vary from specialty to specialty. The indirect practice expenses are determined by surveys. There are several modifications, including the following:
- 1.
Cost of living: geographic practice cost index
- 2.
Malpractice expenses
Factors that affect practice expense for imaging include:
- 1.
Technology utilization assumption rate: duration of equipment usage
- 2.
Equipment depreciation rate
For example, echocardiography (Current Procedural Terminology [CPT] code 93306) has a technical component of 3.75 RVUs (which covers costs related to staff time, disposables, and depreciation costs), a professional component of 1.3 RVUs, and practice expense of 0.48 RVU. The technical component is paid to the physician, or physician group, if they own and operate the equipment, or to the hospital if the hospital owns and operates the equipment.
In the future, however, it has become clear that Medicare will increasingly move away from FFS and RVU-based reimbursements, preferring to shift physician payment into systems based on quality, value, and outcomes of care provided (i.e., value-based purchasing), rather than merely paying physicians a standard level of reimbursement for defined units of work (volume-based payment). Although some health economists and policymakers feel that the days of FFS payment are soon drawing to a close, many experts maintain that the ultimate result of current reforms will be a hybrid payment system blending elements of traditional FFS and value-based payment systems and that such a mixture of payment models will endure for the foreseeable future, such that FFS payment based on the RBRVS will never be entirely eliminated.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree