Acute mesenteric ischemia (
AMI) is a therapeutic emergency, requiring prompt intervention to attain a favorable outcome (
1,
2,
3). Despite modern diagnostic and interventional advancements, the mortality associated with
AMI remains high, historically between 60% and 80% (
4), with more recent reports yielding a range of 52% to 70% (
5,
6). However, the reported high mortality rates are likely confounded by the associated comorbidities in this patient population.
The critical nature of this entity warrants a high index of clinical suspicion, particularly in elderly patients with cardiovascular disease or embolic or thrombotic risk factors. Risk factors for
AMI vary depending on the underlying etiology. Common risk factors for thromboembolic causes of
AMI include older age, atherosclerosis, cardiac arrhythmias, dilated cardiomyopathies, severe cardiac valvular disease, recent myocardial infarction, hypercoagulability, and intra-abdominal malignancy (
1). Risk factors for
AMI attributable to venous thrombosis include dehydration, hypotension, portal hypertension, hypercoagulability, abdominal infection, abdominal malignancy, pancreatitis, trauma, and splenectomy (
7). Predisposing factors associated with the development of nonocclusive
AMI include a low flow state, prolonged hypotension, older age with cardiovascular disease, and medications such as vasopressors or digitalis.
The clinical presentation of
AMI is classically described as acute, severe, periumbilical abdominal pain that is out of proportion to physical exam findings,
with up to 25% of patients manifesting peritoneal signs (
8). The presence of peritoneal signs raises concern that the bowel ischemia has progressed to infarction. Anorexia, nausea, vomiting, diarrhea, and hematochezia are common. Unfortunately, the clinical manifestations of
AMI overlap with other, more common clinical entities, such as bowel obstruction, pancreatitis, diverticulitis, and peritonitis. Therefore, the clinical presentation must be considered in the context of the clinical history and patient-specific risk factors, physical examination, and laboratory and radiographic findings.
Although grouped as a common disease process,
AMI reflects a heterogeneous group of entities, which include occlusive and nonocclusive etiologies that involve the arterial or venous systems. Occlusive causes of
AMI consist of superior mesenteric artery (
SMA) embolus,
SMA thrombosis, mesenteric venous thrombosis, and less common entities such as trauma, strangulated hernias, adhesions, intestinal obstruction, cholesterol emboli, and aortic dissection. Nonocclusive etiologies for
AMI include mesenteric arterial vasoconstriction, also known as nonocclusive mesenteric ischemia (
NOMI), which is usually precipitated by a hypotensive event and/or use of vasopressors. Despite resolution of the hypotension or discontinuation of the vasopressors, persistent mesenteric arterial vasoconstriction (diffuse vasospasm) persists, causing bowel hypoperfusion and intestinal ischemia. Other causes of
NOMI include drugs (i.e., cocaine) and vasculitides.
NOMI can also be seen in association with mesenteric venous thrombosis or distal to an
SMA embolus.
Accurate diagnosis of the cause for
AMI is essential because the presentation, management, and prognosis are influenced by the etiology. To illustrate this point, it is well known that
AMI secondary to mesenteric vein thrombosis often has a relatively insidious onset, whereas a patient with an
SMA embolus usually presents with an abrupt and distinct onset of symptoms. Treatment will radically differ in these two comparative examples as well.
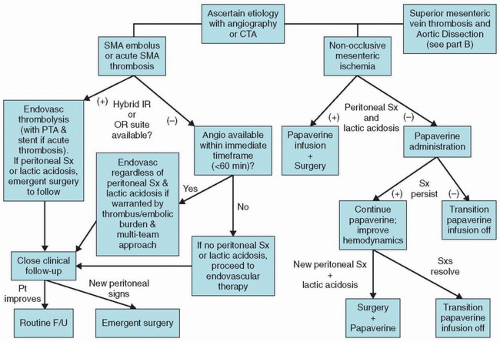
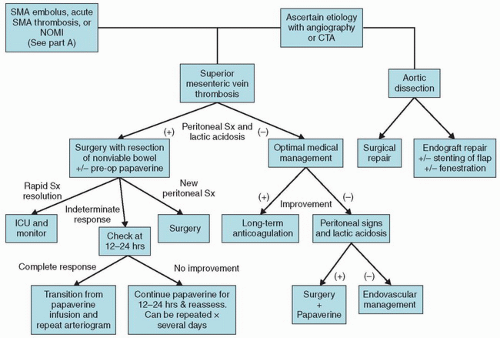
Historically, surgery represented the mainstay of therapy for
AMI, but the treatment algorithm is rapidly evolving into an “endovascular-first” approach at many institutions in an effort to improve patient outcomes (
9). A recent paper showed that the use of endovascular therapy for
AMI has more than doubled from 11.9% in 2005 to 30% in 2009 (
9). There are potential benefits to an endovascular-first approach, including decreased morbidity and mortality, avoidance of general anesthesia and open surgery, more targeted and limited bowel resections, decreased times for revascularization, a reduced need for parenteral nutrition, shortened lengths of stay, and fewer postoperative complications (
2,
9,
10,
11).
Table 9.1 summarizes the differences between the etiologies for
AMI and their management (
8,
7,
12). A treatment algorithm employed at our institutions is demonstrated in
Figure 9.1.