KEY FACTS
Terminology
- •
Acute inflammatory process of pancreas with variable involvement of other local tissues and remote organs
- ○
Interstitial edematous pancreatitis, necrotizing pancreatitis
- ○
Acute pancreatic fluid collection ± infection
- ○
Acute necrotic collection ± infection
- ○
Imaging
- •
Focal or diffuse enlargement of pancreas
- ○
In mild pancreatitis, sonographic signs may be subtle or normal
- ○
- •
Blurred pancreatic outline/margin: Pancreatic edema and peripancreatic exudate
- •
Heterogeneous echotexture due to intrapancreatic necrosis or hemorrhage
- •
Collections: Anechoic peripancreatic fluid; fluid within pancreatic parenchyma or containing debris
- •
Presence of gas suggests infection/bowel fistula unless secondary to interventional procedure
- •
CECT best in late phase to delineate extent of inflammation and detect necrosis and complications
- •
MR best to detect choledocholithiasis or in patients who cannot undergo CECT
- •
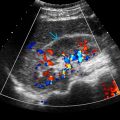
Color Doppler to evaluate for vascular complications: Venous thrombosis, arterial pseudoaneurysms
Top Differential Diagnoses
- •
Infiltrating pancreatic carcinoma
- •
Lymphoma and metastases
- •
Autoimmune pancreatitis
- •
Perforated duodenal ulcer
- •
“Shock” pancreas
Pathology
- •
Interstitial edematous pancreatitis or acute hemorrhagic pancreatitis
Clinical Issues
- •
Usually young and middle-aged groups, M > F
- •
Acute-onset epigastric pain, often radiating to back
- •
Tenderness, fever, nausea, vomiting, ↑ amylase/lipase
- •
Risk factors: Alcohol, gallstones, metabolic, infection, trauma, drugs, ERCP
- •
Hereditary pancreatitis or congenital ductal anomalies
- •
Diagnosis based on presence of at least 2 out of 3 of following: Abdominal pain consistent with pancreatitis, lipase or amylase level > 3x upper limit of normal, imaging findings consistent with acute pancreatitis
- •
Hyperglycemia, increased lactate dehydrogenase, leukocytosis, hypocalcemia, fall in hematocrit, rise in blood urea nitrogen
- •
Revised Atlanta classification of acute pancreatitis: Early phase < 1 week, late phase > 1 week
Scanning Tips
- •
Ultrasound most useful to rule out cholelithiasis in acute pancreatitis
 is hypoechoic but normal in size. The pancreatic duct
is hypoechoic but normal in size. The pancreatic duct  is normal. A small amount of peripancreatic fluid
is normal. A small amount of peripancreatic fluid  is noted.
is noted.
 is enlarged and hypoechoic. Peripancreatic fat planes
is enlarged and hypoechoic. Peripancreatic fat planes  are blurred due to inflammation.
are blurred due to inflammation.
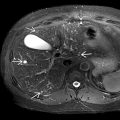
 is enlarged and heterogeneous with segmental areas of decreased echogenicity
is enlarged and heterogeneous with segmental areas of decreased echogenicity  from necrosis. There is peripancreatic fluid
from necrosis. There is peripancreatic fluid  .
.
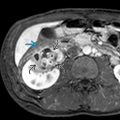
 in the common bile duct
in the common bile duct  , the cause of necrotizing pancreatitis.
, the cause of necrotizing pancreatitis.