Introduction
A solid familiarity of the anatomy of the upper and lower extremity arteries is required for the evaluation of arterial disease. This chapter provides an overview of the upper and lower extremity arterial anatomy. Normal anatomy, common variants, and major collateral routes are depicted by representative arteriograms and illustrations and supplemented with computed tomography (CT) and magnetic resonance (MR) angiography.
Noninvasive imaging is the preferred modality for the initial diagnosis of peripheral arterial disease. CT, magnetic resonance imaging (MRI), and ultrasound are commonly utilized to evaluate patients with signs and symptoms of extremity arterial occlusive disease. Conventional catheter arteriography, although still considered the gold standard for diagnosis, is typically reserved for the treatment of vascular disease. We present angiographic images in this chapter to display arterial anatomy as they are well suited to depict anatomic detail.
The following terms are used to describe extremity anatomy in this chapter. The arm is the portion of the upper extremity between the shoulder and elbow. The forearm is the portion between the elbow and wrist. The thigh is the portion of the lower extremity between the hip and knee, and the calf is the portion between the knee and ankle.
Upper Extremity
Normal features
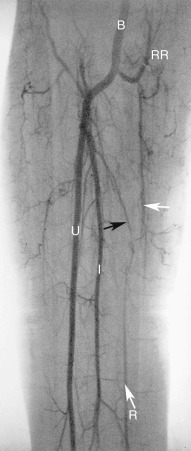
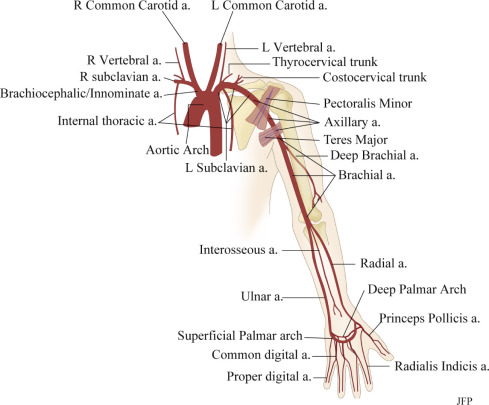
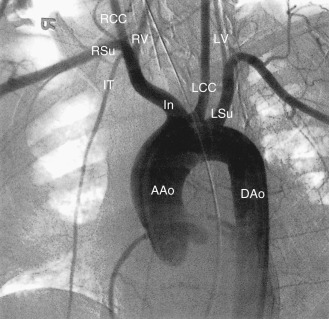
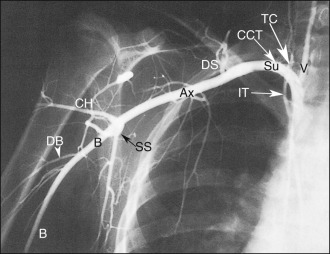
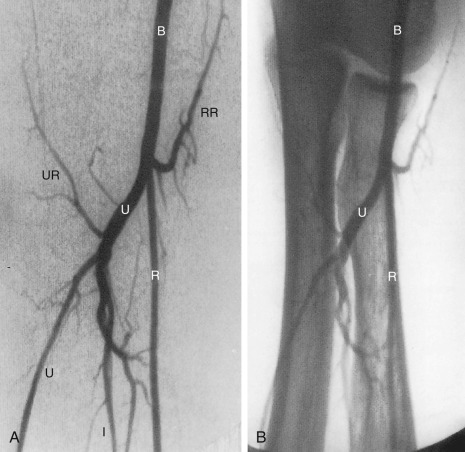
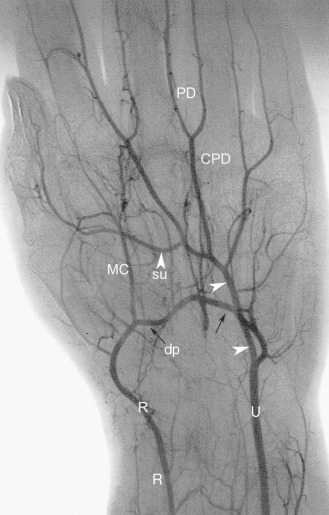
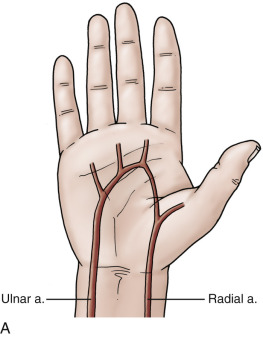
The normal arterial anatomy of the upper extremity is depicted in Fig. 11.1 . Figs. 11.2 to 11.5 are detailed arteriographic views of specific regions of the upper extremity arterial tree, beginning at the aorta and extending to the digits. Please review these figures carefully because their legends provide the instructional content.
Anatomic variants
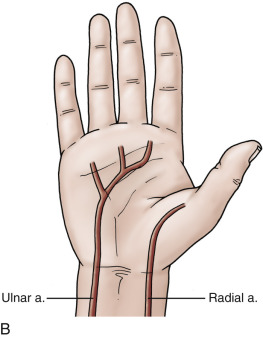
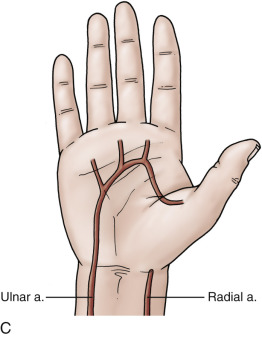
Many anatomic variants can occur in the arterial tree of the upper extremities. The more commonly encountered variants are presented in Table 11.1 . Variations in palmar arch anatomy are commonly seen ( Fig. 11.6 ). Many different potential variations involve both the superficial and deep palmar arches. These variants are important in the evaluation of radial artery anatomy for radial artery harvesting. The most common arrangement is completion of the superficial palmar arch on the radial side. In some individuals, the radial artery fails to communicate with the superficial palmar arch. Familiarity with these variants can prevent confusion and error during duplex examination. An example of an upper extremity anatomic variant is presented in Fig. 11.7 .
| Structure | Variant | Frequency |
|---|---|---|
| Aortic arch and great vessels | Common origin of the right brachiocephalic and left common carotid arteries | 22% |
| Left vertebral artery origin directly from the aorta | 4%–6% | |
| Common origin of both common carotid arteries | <1% | |
| Arm and forearm | Radial artery origin from the axillary artery | 1%–3% |
| Early division of the brachial artery: 1. High origin of the radial artery (see Fig. 11.7 ) 2. Accessory (duplicated) brachial artery | 19% | |
| Ulnar artery origin from the brachial or axillary artery | 2%–3% | |
| Low origin (5–7 cm below elbow joint) of ulnar artery | <1% | |
| Persistent median artery | 2%–4% |
Collateral routes
Many of the branches and tributaries seen in Figs. 11.1 to 11.7 may serve as collaterals when the main arterial trunks of the upper extremity are blocked.
The following is a summary of the more common collateral routes:
- 1.
Obstruction of the proximal subclavian or brachiocephalic arteries:
- a.
collateral flow from cranial and/or neck arteries to the subclavian artery distal to the obstruction (e.g., subclavian steal phenomenon)
- b.
collateral flow from pelvic, abdominal wall, and thoracic wall arteries to the subclavian artery distal to the obstruction
- a.
- 2.
Obstruction of the distal subclavian or axillary arteries:
- a.
collateral flow from the thoracic wall or shoulder region to the axillary artery distal to the obstruction
- a.
- 3.
Obstruction of the brachial artery or its branch vessels:
- a.
collateral flow from the distal arm to the proximal forearm
- b.
collateral flow from the midarm to the distal arm and/or forearm
- c.
retrograde flow filling the palmar arches of the hand
- a.
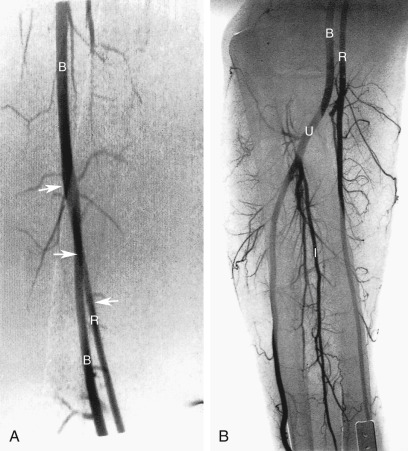
Fig. 11.8 shows an example of collateralization in response to radial artery occlusion.