Aneurysms
ANTERIOR COMMUNICATING (ACOMM) ARTERY ANEURYSMS
KEY FACTS
Represent 30% to 35% of intracranial aneurysms.
Overall incidence of intracranial aneurysms is 2% to 8% of population; risk of bleeding is 1% to 2% per year in previously nonruptured aneurysms.
Aneurysms arising from vessels forming the circle of Willis comprise 90% of all intracranial aneurysms.
Ruptured aneurysms account for 90% of all spontaneous subarachnoid hemorrhage (SAH).
Causes of convexity SAH: older patients = amyloid, venous thrombosis; younger patients = PRES, vasculitis, almost never due to ruptured aneurysm.
>90% of aneurysm ruptures occur between ages of 30 and 70 years.
Aneurysms <5 mm in diameter are unlikely to rupture (critical size: 5 to 7 mm).
Ruptured aneurysms of the AComm artery result in hemorrhage in the gyri recti, anterior inter-hemispheric fissure, septum pellucidum, and frontal horns of lateral ventricles. AComm aneurysms are the most common to show intra-axial hemorrhage (others: middle cerebral artery [MCA], PComm, basilar tip).
Rupture of any intracranial aneurysm results in hydrocephalus in 10% of patients.
There is an association between AComm artery aneurysms and presence of an azygous or fenestrated anterior cerebral artery.
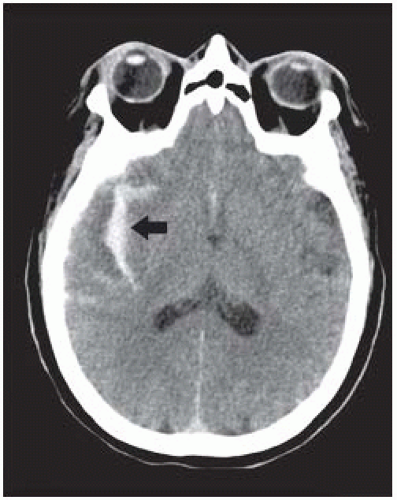
 FIGURE 11-1. Axial noncontrast CT shows acute hemorrhage in the left gyrus rectus with surrounding edema and in the occipital horns of the lateral ventricles. SAH is seen in occipital regions. |
 FIGURE 11-2. Axial CT in the same patient shows SAH along the anterior interhemispheric fissure, septum pellucidum, and lateral ventricles. |
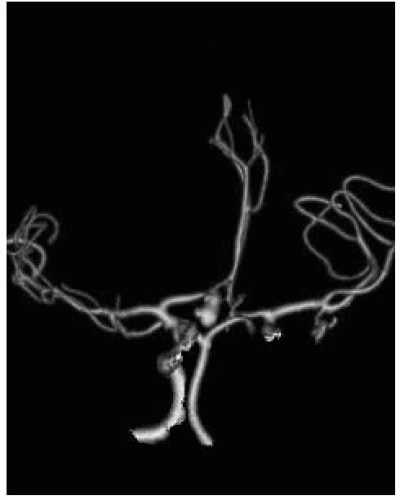 FIGURE 11-3. In the same patient, coronal computed tomography angiography (CTA) shows an aneurysm (arrow) in the region of the AComm artery. (See color insert) |
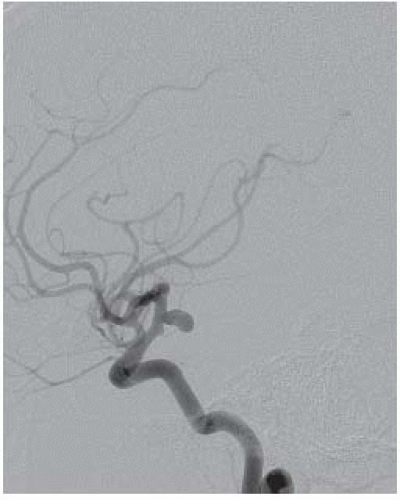
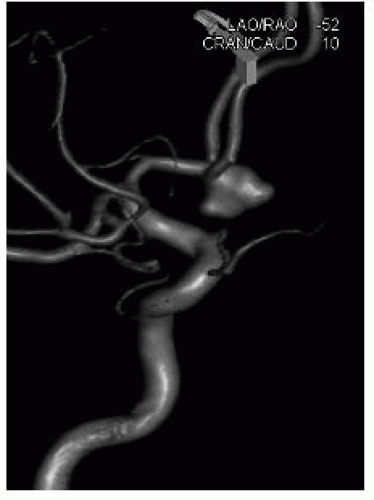 FIGURE 11-4. 3-D digital subtraction angiography (DSA) view, in a different patient, shows an irregular and ruptured AComm aneurysm. (See color insert) |
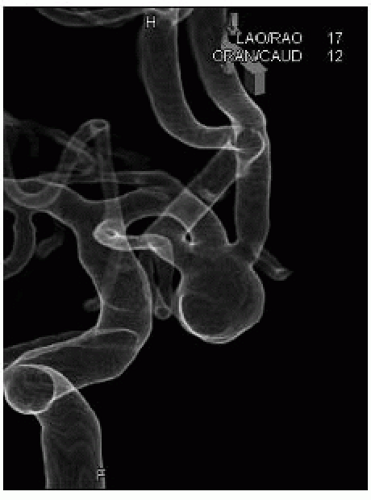 FIGURE 11-5. Translucent 3-D DSA view, in a different patient, shows an AComm aneurysm incorporating several arteries in its base. (See color insert) |
SUGGESTED READING
Salary M, Quigley MR, Wilberger JE Jr. Relation among aneurysm size, amount of subarachnoid blood, and clinical outcome. J Neurosurg 2007;107:13-17.
POSTERIOR COMMUNICATING ARTERY ANEURYSMS
KEY FACTS
Represent 30% to 35% of intracranial aneurysms, may be “mirror-like.”
Present with ipsilateral third cranial nerve palsy and/or SAH.
In ruptured posterior communicating artery aneurysm, SAH tends to be diffuse but may be concentrated in basilar cisterns; they may also bleed into mesial temporal lobe region.
May be difficult to see on CTA, particularly if small and pointing inferiorly.
50% of patients with any ruptured intracranial aneurysm die during the first 30 days that follow the initial hemorrhage.
Almost all intracranial aneurysms are considered to result from hemodynamic stress and not from a congenital cause (only 2% of aneurysms are found in children).
Perimesencephalic bleeds may occur without aneurysm rupture and may be due to tearing of small veins; DSA is usually negative.
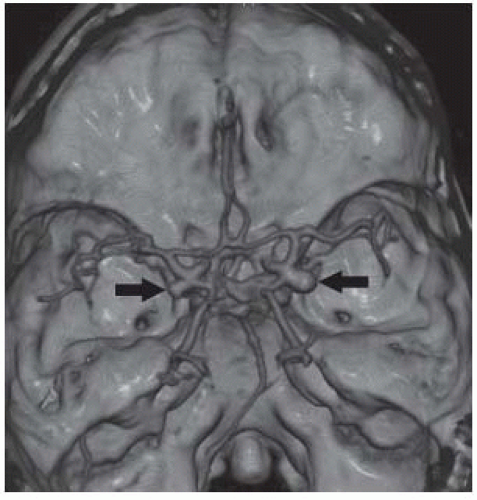 FIGURE 11-6. Top view of CTA shows bilateral posterior communicating artery aneurysms (arrows). (See color insert) |
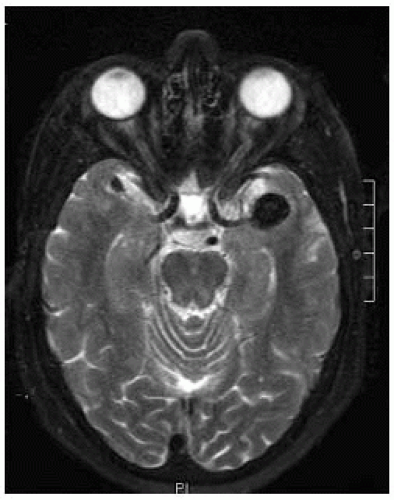
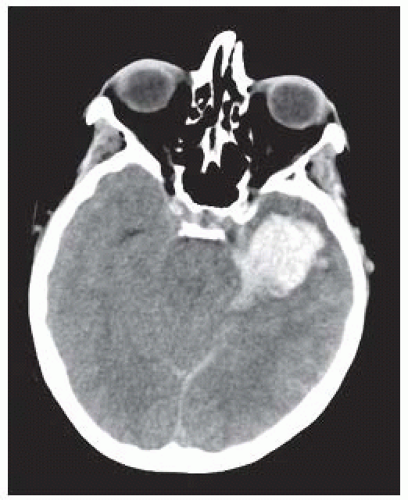 FIGURE 11-8. Axial noncontrast CT shows the left temporal lobe and adjacent perimesencephalic SAH due to ruptured PComm aneurysm. |
SUGGESTED READING
Bahrami S, Yim CM. Quality initiatives: blind spots at brain imaging. Radiographics 2009;29:1877-1896.
Wiebers DO, Whisnant JP, Huston J III, Meissner I, Brown RD Jr, Piepgras DG, et al.; International Study of Unruptured Intracranial Aneurysms Investigators. Unruptured intracranial aneurysms: natural history, clinical outcome, and risks of surgical and endovascular treatment. Lancet 2003;362:90-91.
MIDDLE CEREBRAL ARTERY BIFURCATION ANEURYSMS
KEY FACTS
Represent 20% to 30% of intracranial aneurysms; may be “mirror-like.”
Rupture results in SAH in sylvian fissures, frontal opercula, and basilar cisterns.
Risk of rebleeding from any ruptured intracranial aneurysm is 20% to 50% during the 2 weeks that follow presentation.
Factors associated with increased risk of intracranial aneurysms include fibromuscular dysplasia, polycystic kidney disease, connective tissue disorders, aortic coarctation, and patients with intracranial arteriovenous malformations (AVMs) or hypervascular tumors (GBMs [glioblastoma multiforme], meningiomas), and magnetic resonance angiography (MRA) is beneficial in screening these patients.
MRA detects over 90% of intracranial aneurysms 3 mm or greater in diameter (MRA at 3T may detect smaller ones); CTA may detect those down to 1 mm; CTA may show more aneurysms than catheter angiography, but 3-D rotational catheter angiography still is “gold standard.”
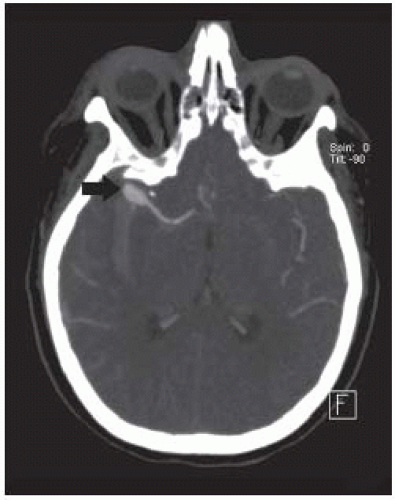 FIGURE 11-10. MIP axial view from CTA in the same patient clearly shows an MCA bifurcation aneurysm (arrow). |
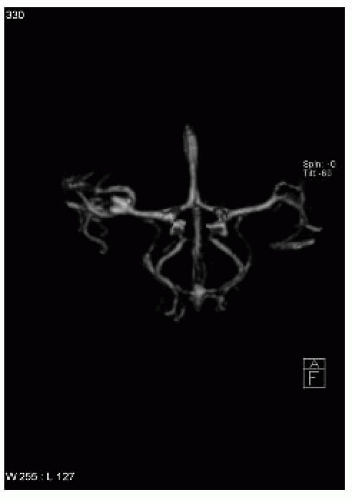 FIGURE 11-11. Surface rendered CTA shows the aneurysm. (See color insert) |
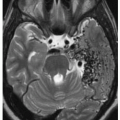
 FIGURE 11-12. Axial noncontrast CT shows an incidental and a partially calcified left MCA aneurysm (arrow). |
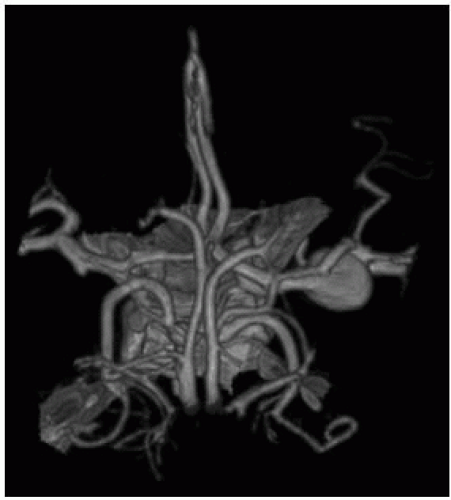 FIGURE 11-14. CTA in the same patient clearly shows the left MCA bifurcation aneurysm. (See color insert) |
SUGGESTED READING
Jabbour PM, Tjoumakaris SI, Rosenwasser RH. Endovascular management of intracranial aneurysms. Neurosurg
Clin N Am 2009;20:383-398. Rinkel GJ. Intracranial aneurysm screening: indications and advice for practice. Lancet Neurol 2005;4:122-128.
BASILAR ARTERY TIP ANEURYSMS