Angioplasty and Stenting for Chronic Venous Disease
Raj P. Shah
Michael J. Hallisey
Primary balloon angioplasty of the venous system has high technical failure and short-term reocclusion rates. The use of venous stents improves long-term patency by preventing elastic recoil. The one exception to this high failure rate of primary venous percutaneous transluminal (balloon) angioplasty (PTA) may be in patients with previous central venous catheters who are not on chronic hemodialysis; in these patients, balloon angioplasty alone may provide significant improvement. A technique that is useful and feasible in treating venous stenoses is ultrahigh-pressure balloon PTA. Ultrahigh-pressure PTA may provide prolongation after venous angioplasty, especially in the outflow of hemodialysis grafts. Percutaneous cutting balloon (PCB) angioplasty is a technique that is useful for certain types of highly scarred or resistant stenoses. However, PCB angioplasty should be used as a backup to suboptimal primary balloon PTA due to higher complication rates and the fact that it may be more painful than conventional balloon PTA.
Indications
Patient with symptoms resulting from
1. Superior vena cava (SVC) obstruction from malignant and benign causes (1,2). SVC syndrome is most common with thoracic malignancy (80% to 90%), usually secondary to bronchogenic carcinoma.
2. Subclavian and brachiocephalic vein stenoses secondary to prior indwelling central venous catheters
3. Recurrent subclavian vein stenoses in patients with Paget-Schroetter or thoracic outlet syndrome after the patient have undergone resection of the first rib and/or head of the clavicle (3).
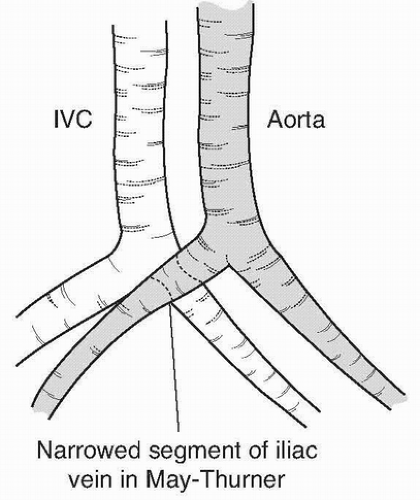
4. Iliofemoral vein/inferior vena cava (IVC) obstructions: May-Thurner or Cockett syndrome (Fig. 37.1) (4). Stents should be used when there is residual obstruction after balloon PTA and extrinsic compression of IVC (e.g., by enlarged caudate lobe of liver or nodular compression).
6. Budd-Chiari syndrome. Endovascular treatment has become the treatment of choice due to minimal trauma and fast recovery.
7. Portal vein stenoses or occlusions
8. Chronic venous occlusion: Chronic, occlusive deep venous thrombosis (DVT) and postthrombotic syndrome (PTS); consider endovascular intervention after maximizing medical management.
9. Pulmonary vein stenosis: There are published reports of venous angioplasty successfully treating pulmonary vein stenosis following lung transplant. However, further studies are required to validate safety and long-term efficacy.
10. Multiple sclerosis (MS): Various reports in the peer-reviewed published literature describe a potential relationship between the abnormal venous circulation termed chronic cerebrospinal venous insufficiency (CCSVI) and MS. Current evidence on the efficacy of percutaneous venoplasty for CCSVI for MS is inadequate in quality and quantity. Therefore, this procedure should only be used in the context of research.
Contraindications
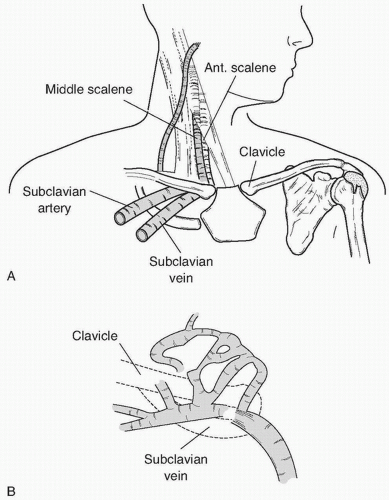
1. Paget-Schroetter syndrome (effort thrombosis): Transient, intermittent traumatic extrinsic compression of the subclavian vein between the subclavius muscle and the costocoracoid ligament, causing local inflammation and occlusive thrombosis.
2. Thoracic outlet syndrome: Entrapment of the subclavian vein at its exit from the thorax between the first rib and clavicle. This disorder is not due to an endoluminal abnormality.
Note: Primary stent placement and balloon PTA is contraindicated in these patients. The underlying pathology is not endoluminal; therefore, angioplasty and/or stenting may complicate the treatment which requires thrombolysis followed by surgery. Moreover, stenting of these segments leads to repetitive compressive trauma to the stent and reocclusion. Surgical resection of the compressive lever (first rib or head of the clavicle) should be initially performed (Fig. 37.2). Stenting should be reserved for those patients who have previously undergone first rib resection for Paget-Schroetter or benign vein obstruction and have resistant or repeated failures with balloon PTA.
Preprocedure Preparation
1. Review of patient history for:
a. Previous central line insertion
b. Weightlifting or heavy arm exercise
c. Previous intrathoracic surgery
d. Malignancy
2. Review thoracic computed tomography (CT) scan to assess if there is a mass causing compression of the SVC.
3. For patients with a venous stenosis near other vascular or enteral structures, it is important to do a preprocedure CT scan before cutting balloon can be used to ensure that the adjacent structures are not damaged.
4. Stop all oral intake overnight.
5. Obtain laboratory parameters: creatinine, international normalized ratio (INR), prothrombin time (PT), partial thromboplastin time (PTT), platelets, and hematocrit.
6. If the stenosis is in the upper extremity of a patient who is not on hemodialysis, bilateral upper arm intravenous access is obtained prior to patient arrival in the interventional suite.
7. For patients with laryngeal edema or shortness of breath, who are unable to lie flat for the procedure, intubation and general anesthesia may be required.