TERMINOLOGY
Abbreviations
- •
Inferior vena cava (IVC)
Definitions
- •
“Proximal” and “distal” in arterial and venous systems apply to position of arterial and venous segment in relation to heart (rather than direction of flow)
- •
Aneurysm: Focal increase in caliber of artery with diameter of dilated segment measuring at least 1.5x > adjacent unaffected segments
GROSS ANATOMY
Overview
- •
Abdominal aorta
- ○
Enters abdomen at T12 level, bifurcates at L4
- ○
Level of origins of major branches: Celiac axis (T12), superior mesenteric artery (SMA) (L1), renal arteries (L1/2), IMA (L3), common iliac arteries (L4)
- ○
- •
IVC
- ○
Blood from alimentary tract passes through portal venous system before entering IVC through hepatic veins
- ○
Begins at L5 level with union of common iliac veins
- ○
Leaves abdomen via IVC hiatus in diaphragm at T8 level
- ○
IVC tributaries correspond to paired visceral and parietal branches of aorta
- ○
IVC development has complex embryology
- –
Various anomalies common (up to 10% of population), especially at and below level of renal veins
- –
All are variations of persistence/regression of embryologic sub- and supracardinal veins
- –
- ○
IMAGING ANATOMY
Overview
- •
Not all branches of abdominal aorta and tributaries of IVC can be well seen on ultrasound examination
- •
Major arterial branches of abdominal aorta seen on ultrasound
- ○
Celiac artery, common hepatic artery, splenic artery, SMA, inferior mesenteric artery (IMA), renal arteries, common iliac arteries
- ○
- •
Major venous tributaries draining into IVC
- ○
Common iliac veins, renal veins, hepatic veins
- ○
Internal Contents
- •
Abdominal aorta
- ○
Normal peak systolic velocity (PSV): 60-110 cm/s
- ○
Spectral Doppler waveform
- –
Upper: Narrow, well-defined systolic complex with forward flow during diastole
- –
Mid: Reduced diastolic flow
- –
Distal: Absent diastolic flow, similar to lower limb arteries
- –
- ○
Normal caliber: 15-25 mm
- –
Upper: 22 mm above renal arteries
- –
Middle: 18 mm below renal arteries
- –
Lower: 15 mm above bifurcation
- –
- ○
Best imaging plane: Both transverse and longitudinal
- ○
- •
Celiac axis
- ○
Normal PSV: 98-105 cm/s
- ○
Spectral Doppler demonstrates low-resistance flow with high end-diastolic velocities
- ○
Flow velocity not dependent on food intake
- ○
Normal caliber: 6-10 mm
- ○
Best imaging plane: Transverse plane to show typical T-shaped bifurcation
- ○
- •
Common hepatic artery
- ○
Normal PSV: 70-120 cm/s
- ○
Spectral Doppler shows low-resistance flow characteristics with large amount of continuous flow in diastole
- ○
Normal caliber: 4-10 mm
- ○
Best imaging plane
- –
Start transverse midline to follow common hepatic artery to right of T-shaped bifurcation from celiac axis
- –
Gastroduodenal artery may be seen to arise from common hepatic artery along anterosuperior aspect of pancreas; thereafter, common hepatic artery becomes proper hepatic artery
- □
Proper hepatic artery normal PSV: 60-100 cm/s
- □
- –
- ○
- •
Splenic artery
- ○
Normal PSV: 70-110 cm/s
- ○
Spectral Doppler shows typically turbulent flow due to tortuosity of vessel
- ○
Normal diameter: 4-8 mm
- ○
Best imaging plane
- –
Transverse midline approach shows proximal portion of artery wall
- –
Intercostal through spleen, using it as acoustic window; useful for showing distal splenic artery around hilum
- –
- ○
- •
SMA
- ○
Normal PSV: 97-142 cm/s
- ○
Spectral Doppler demonstrates high impedance flow with low diastolic velocities during fasting due to relative vasoconstriction
- ○
End-diastolic velocity increases typically 30-90 minutes after meals due to vasodilation of mesenteric branches
- ○
Normal caliber: 5-8 mm
- ○
Best imaging plane
- –
Longitudinal midline approach best for evaluation of SMA blood flow
- –
Transverse plane useful for identifying short anteriorly directed stump; shows dot-like appearance, surrounded by distinctive triangular mantle of fat
- –
- ○
- •
IMA
- ○
Normal PSV: 93-189 cm/s
- ○
Spectral Doppler demonstrates high impedance flow with low diastolic velocities during fasting due to relative vasoconstriction
- ○
End-diastolic velocity increases after meal due to vasodilation of mesenteric branches
- ○
Normal caliber: 1-5 mm
- ○
Best imaging plane: Transverse plane following line of aorta; origin of IMA arises from below origins of renal arteries and may be anterior or slightly to left of midline
- ○
- •
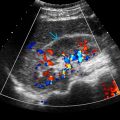
Renal arteries
- ○
Normal PSV: 60-140 cm/s, not > 180 cm/s
- ○
Spectral Doppler demonstrates open systolic window, rapid systolic upstroke occasionally followed by secondary slower rise to peak systole with subsequent gradual diastolic delay but with persistent forward flow in diastole
- ○
Normal caliber: 5-8 mm
- ○
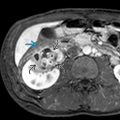
Best imaging plane
- –
Transverse anterior midline approach best for identification of origins of renal arteries
- –
Posterolateral approach using kidneys as acoustic window useful for visualization of distal portions of renal arteries
- –
- ○
- •
Common iliac arteries
- ○
Normal spectral Doppler shows characteristic triphasic waveform
- –
Initial high-velocity peak forward-flow phase resulting from cardiac systole
- –
Brief phase of reverse flow in early diastole
- –
Low-velocity forward flow in diastole
- –
- ○
Normal caliber: 8-12 mm
- ○
Best imaging plane: Transverse anterior approach and oblique anterior approach along long axis of iliac arteries
- ○
Stenosis causing 1-19% diameter reduction
- –
Triphasic waveform with minimal spectral waveform broadening
- –
PSV increase < 30% relative to adjacent proximal segment; proximal and distal waveform remain normal
- –
- ○
Stenosis causing 20-49% diameter reduction
- –
Triphasic waveform usually maintained, though reverse flow component may be diminished
- –
Spectral broadening prominent with filling in of area under systolic peak
- –
PSV increase 30-100% relative to adjacent proximal segment; proximal and distal segment remain normal
- –
- ○
Stenosis causing 50-99% diameter reduction
- –
Monophasic waveform with loss of reverse flow component, forward flow throughout cardiac cycle
- –
Extensive spectral broadening
- –
PSV increase > 100% relative to adjacent proximal segment
- –
Distal waveform monophasic with reduced systolic velocity
- –
- ○
Occlusion
- –
No flow, preocclusive thump may be heard proximal to site of obstruction
- –
Distal waveforms are monophasic with reduced systolic velocities
- –
- ○
- •
IVC
- ○
Normal PSV: 44-118 cm/s
- ○
Spectral Doppler shows slow flow that varies with respiration and cardiac pulsation
- ○
Normal caliber: 5-29 mm during quiet inspiration
- ○
Best imaging plane: Both transverse and longitudinal
- ○
- •
Common iliac veins
- ○
Spectral Doppler shows 5 normal characteristics
- –
Spontaneous flow, phasic flow, flow ceases with Valsalva maneuver, flow augmentation with distal compression, unidirectional flow toward heart
- –
- ○
Best imaging plane: Transverse anterior approach and oblique anterior approach along long axis of iliac veins
- ○
- •
Renal veins
- ○
Normal PSV: 18-33 cm/s
- ○
Right renal vein relatively short and drains directly into IVC
- ○
Left renal vein runs a slightly longer course; receives left gonadal vein, usually courses anterior to aorta before joining IVC
- ○
Spectral Doppler of right renal vein mirrors pulsatility of IVC
- ○
Spectral Doppler of left renal vein may show only slight variability of flow velocities consequent upon cardiac and respiratory activity
- ○
Normal caliber: 4-9 mm
- ○
Best imaging plane: Transverse anterior approach
- ○
- •
Hepatic veins
- ○
Normal PSV: 16-40 cm/s
- ○
Spectral Doppler shows triphasic waveform due to transmitted cardiac activity
- ○
Best imaging plane: Transverse/oblique subcostal approach with cranial angulation
- ○
ANATOMY IMAGING ISSUES
Imaging Recommendations
- •
Use 2- to 5-MHz transducer
- •
Fasting for 12 hours recommended to reduce interference by bowel gas; satisfactory Doppler signal for aorta and IVC can be obtained in up to 90% of patients
- •
Imaging patient in morning after overnight fast most convenient protocol
- •
Lateral decubitus position and graded compression to displace intervening bowel gas may be useful
- •
Angle correction crucial in spectral Doppler assessment
- •
Detailed delineation of branches of aorta and IVC better assessed on CTA or MRA
- •
Digital subtractive angiography usually reserved for when intervention may be required (e.g., embolization of mesenteric artery branches in gastrointestinal bleed, renal artery stenting, etc.)
Imaging Approaches
- •
Proximal aorta can be scanned either from an anterior epigastric approach or right coronal approach
- •
Midaorta can be scanned either from a midanterior abdominal approach or by placing the patient in the left lateral decubitus or the right lateral decubitus position, which will allow partial visualization of aorta in the region of the kidney
- •
Distal aorta can be scanned from inferior anterior abdominal window or a coronal approach
- ○
A coronal approach allows visualization of the distal aorta and both common iliac arteries simultaneously
- ○
- •
Because there is usually no gap between the spine and aorta, when measuring the longitudinal aorta in anterior-posterior dimension, ensure that the spine is not included in the measurement; the aorta wall and spine are both very echogenic and may be difficult to delineate
Imaging Pitfalls
- •
Bowel gas, patient body habitus, and operator dependence are main factors contributing to suboptimal ultrasound examination of aorta and IVC
AORTA AND INFERIOR VENA CAVA