Abstract
Objective
The purpose of this study was to evaluate and compare the swallow-related muscles and bones movement patterns during swallowing quantitatively by B+M-mode ultrasound, and to investigate its application value in dysphagia.
Methods
Sixty elderly stroke patients with dysphagia (patient group) and sixty healthy elderly individuals (control group) were enrolled in this study. M-mode ultrasound was utilized to measure the radial displacement and duration of tongue and geniohyoid muscle movements. B-mode ultrasound was employed to assess hyoid bone displacement and the distance of hyoid-larynx approximation. Ultrasound parameters were compared between the two groups. Logistic regression was used to identify the optimal parameters with independent predictive value. The predictive efficacy of each parameter for dysphagia was evaluated using ROC curve analysis.
Results
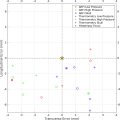
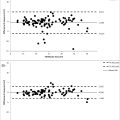
Both intraindividual and interindividual variations were observed in the B+M-mode imaging traces during the three swallows. Significant differences were found in the average radial displacement and duration of tongue and geniohyoid muscle movements, hyoid bone displacement, and hyoid-larynx approximation distance between the two groups (all p < 0.001). The radial displacement of the tongue and geniohyoid muscle, hyoid bone displacement, and hyoid-larynx approximation distance were lower in the patient group compared to the control group, while the duration of tongue and geniohyoid muscle movements was higher in the patient group. Logistic regression selected the radial displacement of the tongue, the duration of geniohyoid muscle movement, and the hyoid-larynx approximation distance as significant predictors. The combined model demonstrated excellent predictive performance with an AUC of 0.994 and good model fit ( p < 0.001).
Conclusion
The B+M-mode ultrasound offers a rapid and safe technique for the preliminary evaluation of swallowing movements. It can serve as a quantitative and noninvasive method for the clinical screening of dysphagia.
Introduction
Dysphagia is an independent predictor of an unfavorable prognosis within three months poststroke [ , ]. Approximately 49% of stroke patients are referred to rehabilitation centers due to dysphagia and malnutrition [ ]. Dysphagia following a stroke can lead to numerous complications, including aspiration pneumonia, dehydration, malnutrition, prolonged hospital stays, and increased mortality rates [ , ], which severely impact patient prognosis and quality of life, and can even be life-threatening. Various methods have been employed to track and detect swallowing function. Among these, the videofluoroscopic swallowing study (VFSS) is considered the gold standard for evaluating swallowing and dysphagia [ , ]. This method utilizes conventional X-rays to monitor the movement of radiopaque barium through the upper gastrointestinal tract in real time. However, its use is limited by the risk of radiation exposure and aspiration, making repeated evaluations challenging. Ultrasound offers a promising alternative, capable of accurately assessing dysphagia severity and grade [ , ]. Additionally, ultrasound avoids damage to the muscles and bones involved in swallowing, thus reducing the incidence of dysphagia during head and neck treatments [ ]. As a simple, safe, nonradiative, noninvasive, and easily repeatable technique, ultrasound holds significant promise for the assessment of swallowing function.
The use of ultrasound imaging technology for evaluating dysphagia in rehabilitation and clinical diagnosis has gained popularity in recent years. Its application in treatment is also increasingly widespread. Previous studies [ , , ] typically selected only one or two indicators to evaluate swallowing function, without assessing the movement or coordination of the oral cavity and larynx. Swallowing is a complex physiological process requiring the coordinated movement of several muscles and bones in the mouth, pharynx, larynx, and esophagus [ , ]. Proper oral and laryngeal coordination is crucial for normal swallowing movements [ , ]. Evaluating the coordinated movements of these structures is essential for assessing swallowing function. However, there were no criteria for ultrasound assessment of dysphagia. We used ultrasound to measure the indicators related to swallowing movement in our study. We compared the results of indicators between the two groups to investigated whether it has diagnostic significance in evaluating dysphagia. We established a model to evaluate the diagnostic efficacy of each parameter, tried to establish a reference range for the quantitative ultrasound assessment of dysphagia.
Materials and methods
Participants
The prospective study was approved by the Ethics Committee of the First Affiliated Hospital of Henan University of Chinese Medicine (Reference No: 2022HL-466). Informed consent was obtained from all subjects. Between December 2021 and December 2022, sixty stroke patients with dysphagia (29 males, 31 females) and sixty healthy elderly individuals (32 males, 28 females) were recruited for this study. Participants in both groups were aged between 60 and 80 years. Inclusion criteria for the patient group: Stroke was defined according to the criteria established by the World Health Organization based on imaging evidence obtained from computed tomography (CT) or magnetic resonance imaging (MRI). Patients with dysphagia were confirmed by VFSS. Exclusion criteria for the patient group: Patients who were unable to cooperate with the examination; patients with congenital oral malformations or a history of orthodontic surgery; patients with other diseases, aside from stroke, that could cause dysphagia; patients who were too difficult to cooperate with swallowing. Exclusion criteria for the control group: Subjects with complaints or a history of swallowing difficulties, or any medical conditions that might affect deglutition. Descriptive characteristics of the two groups are shown in Table 1 .
| Patients Group ( n = 60) | Control Group ( n = 60) | Z Value | p Value | |
|---|---|---|---|---|
| Gender (male/female) | 29/31 | 32/28 | 0.298 | 0.585 |
| Age (years) | 71.19 ± 5.98 | 70.69 ± 3.22 | −0.684 | 0.495 |
| Height (cm) | 165.20 ± 5.10 | 164.82 ± 6.24 | −0.446 | 0.999 |
| Weight (kg) | 61.08 ± 8.07 | 62.24 ± 7.46 | 0.656 | 0.319 |
Ultrasonographic examination
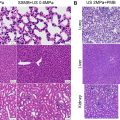
The ultrasonic inspection and image analysis of all subjects were conducted by the same qualified operator. The machine used in our study was equipped with a 3.5-MHz curved-array transducer (35C50EB Convex Array, Mindray Resona R9, Shenzhen, China). All images were analyzed manually. Participants were inspected while sitting in a comfortable position and facing forward. The transducer was placed in the midsagittal plane in the submental area, between the anterior border of the hyoid bone and the posterior border of the mandibular symphysis. The transducer was slid to the larynx for measuring the hyoid-larynx approximation distance, while other parameters were detected in the midsagittal plane in the submental area. Appropriate pressure was applied to ensure the stability of the images. The M-mode scan line was located 2 cm away from the tip of the hyoid bone ( Fig. 1 ). Participants were asked to swallow 5 ml of water three times at an interval of 1–2 minutes between each swallow, with their heads remaining in a neutral position. The radial displacement and duration of tongue and geniohyoid muscle movement, hyoid bone displacement, and hyoid-larynx approximation distance ( Figs. 2–7 ) were recorded and evaluated during swallowing using B+M-mode ultrasonography. The measurements were repeated three times for each participant to obtain the average value for statistical analysis ( Figs. 3 , 4 , & 6 ).





Videofluoroscopic swallowing study
Additionally, all subjects underwent Videofluoroscopic Swallowing Study (VFSS) examination prior to ultrasound examination. VFSSs were conducted at our institute using fluoroscopic equipment with a remote control and a high-resolution super-VHS recorder at a rate of 30 frames per second. The patient was positioned in a sitting posture with the head naturally upright, and fluoroscopy was performed in both anteroposterior and lateral positions. During the examination, participants ingested 5 mL of thin barium sulfate, and the entire swallowing process was videotaped. Upon the onset of aspiration, the examination was halted, and postural drainage was administered. Two radiologists, trained in dysphagia diagnosis and treatment, analyzed the video images and reached a consensus. Abnormal features were documented, and dysphagia was diagnosed. Participants were instructed to avoid head swinging during swallowing and to maintain a natural neck posture.
Evaluation of the swallowing process: (1) Oral phase: The ingestion, chewing, and formation of food boluses in the patient’s mouth were observed. Evaluation criteria included the rate of oral food intake, number of chews, and size and shape of the food bolus. (2) Pharyngeal phase: Muscle movements in the throat were observed, focusing on laryngeal elevation, pharyngeal contraction, and epiglottis closure. Additionally, attention was paid to the presence of food residues in the throat, such as residue and aspiration. (3) Esophageal phase: The progression of food through the esophagus was observed, with evaluation criteria including esophageal peristalsis and presence of esophageal residues. Esophageal dilation was also noted, including the degree and duration of dilation.
Statistical analysis
SPSS software (SPSS Statistics 26.0; SPSS Inc., Chicago, IL, USA) was utilized for statistical analyses. Normality of data distribution was assessed for all variables. Normally distributed continuous variables were presented as mean ± standard deviation (SD), while non-normally distributed variables were expressed as median (interquartile range). The independent samples t-test was performed to determine the difference between the two groups. Logistic regression was used to screen out statistically significant parameters ( p < 0.05) to establish the model by MedCalc software, by stepwise regression analysis (MedCalc Software, Ostend, Belgium). Receiver operating characteristic (ROC) curve analysis was performed to assess the predictive value of each parameter for dysphagia, with the area under the curve (AUC) compared using the DeLong test. Statistical significance was defined as p < 0.05.
Results
Descriptive characteristics of subjects
The descriptive characteristics of the subjects are presented in Table 1 . No statistically significant differences were observed between the two groups in terms of sex, age, height, and weight ( p > 0.05).
The analysis of the repeatability of the operator
Intraclass correlation coefficient was used to analyze the repeatability of three measurements by the same operator. ICC of the swallowing-related indicators was in Table 2 . The ICC of all indicators was greater than 0.75 (all p < 0.001). The results showed that three measurements by the same operator had good repeatability.