Abstract
Rationale and Objectives
Accurate assessment of fetal head station (FHS) is crucial during labor management to reduce the risk of complications and plan the mode of delivery. Although digital vaginal examination (DVE) has been associated with inaccuracies in FHS assessment, ultrasound (US) evaluation remains dependent on sonographer expertise. This study aimed at investigating the reliability and accuracy of an automatic approach to assess the FHS during labor with transperineal US (TPU).
Materials and Methods
In this prospective observational study, 27 pregnant women in the second stage of labor, with fetuses in cephalic presentation, underwent conventional labor management with additional TPU examination. A total of 45 2D B-mode TPU acquisitions were performed at different FHS, before performing DVE. The FHS was assessed by the algorithm (FHS aut ) on TPU images and by DVE (FHS dig ). The sonographic assessment of FHS by expert sonographer (FHS exp ) on the same TPU acquisition used for the automatic measurement served as gold standard. The performance and accuracy were assessed through Spearman’s ρ , the coefficient of determination ( R 2 ), root mean square error (RMSE), and Bland–Altman analysis.
Results
A strong correlation between FHS aut and FHS exp ( ρ = 0.97, p < 0.001) and a high coefficient of determination ( R 2 = 0.95) were found. A lower correlation with FHS exp ( ρ = 0.66, p < 0.001) and coefficient of determination ( R 2 = 0.52) was found for DVE. Moreover, the RMSE reported higher accuracy of FHS aut (RMSE = 0.32 cm) compared to FHS dig (RMSE = 0.97 cm). Bland–Altman analysis showed that the algorithm performed with smaller bias and narrower limits of agreement compared to DVE.
Conclusion
The proposed algorithm can evaluate FHS with high accuracy and low RMSE. This approach could facilitate the use of US in labor, supporting the clinical staff in labor management.
Introduction
The correct evaluation of fetal head position and station is essential in the management of labor, as inaccurate assessment of these parameters can increase the risk of maternal and fetal complications. Typically, digital vaginal examination (DVE) is the standard method for assessing fetal head station (FHS). However, several studies [ ] have shown the inaccuracy of digital examination compared to ultrasound (US) evaluation [ ], with reported error rates ranging from 20% to 70%. The inaccuracy could become even worse in cases of abnormal head position when the clinical staff need to pay closer attention. Furthermore, additional studies have documented elevated risks of infections and injuries associated with the DVE procedure [ ]. In recent decades, the use of intrapartum US has played a key role in investigating labor progression, providing crucial insight into fetal descent and position through a safe and noninvasive procedure [ ]. For example, Dall’Asta et al. [ ] demonstrated how sonographic assessment of fetal head flexion can be a valuable tool in predicting labor outcomes and potentially reducing unnecessary cesarean deliveries.
Furthermore, the possibility to detect the FHS is pivotal in the clinical routine, since it facilitates the prognostication of the delivery mode [ ].
Nevertheless, the effectiveness of intrapartum US strictly relies upon sonographer experience, as the identification of different anatomical structures is prone to intra- and interobserver variability [ , ]. A recent study from Mappa et al. [ ] has shown how, although US can be more accurate than clinical evaluation in assessing fetal position and station, its use remains limited.
A promising strategy to address the aforementioned limitations could be the development of computational methods for automating the measurement of labor progression indicators [ ], such as the FHS. In this context, the group of Casciaro et al. [ ] introduced the first noninvasive and automatic approach for measuring labor progression with transperineal US (TPU) examinations. Over time, this approach has undergone further refinement and specialization to measure various parameters, including the angle of progression (AoP) [ , ], the head-to-perineum distance (HPD) [ ], and the extent of AoP and HPD during the pushing [ ]. In particular, HPD is an indirect measurement of FHS, which can be performed only by TPU (and not by DVE) and for this reason, it is still poorly used in clinical routine, especially by midwives. The present study measured directly the FHS value, which currently is by far the most adopted fetal parameter for the assessment of labor progression, especially because it can be measured by both TPU or DVE and therefore it is largely used not only by gynecologists but also by midwives. Therefore, the objective of this study was to investigate the accuracy of the methodology developed as a kind of “proof of concept” by Casciaro et al. [ ] for the automated assessment of the FHS during the second stage of labor using TPU [ ]. The approach of Casciaro et al. [ ] relied on the automatic identification and segmentation of key anatomical references required for measuring the FHS (i.e., pubic symphysis, infrapubic plane, and fetal head) on TPU images acquired during the second stage of labor. In this study, a software application has been fully developed, equipped with an appropriate GUI, and integrated in a dedicated certified medical device. This operation has improved the acquisition procedure, bringing to a higher operator-independence and user-friendliness of the device. Furthermore, the algorithm has been optimized to work with standardized 224 × 224 images provided by the dedicated device and validated in order to assess its performance. The algorithm evaluation was conducted by comparing the automatic evaluation of FHS provided by the algorithm (FHS aut ) with the assessment of an expert physician, considered the gold standard. Specifically, the physician’s assessment of the FHS (FHS exp ) was performed on TPU scan, following the International Society of Ultrasound in Obstetrics and Gynecology (ISUOG) Practice Guidelines [ ]. Moreover, the assessment of FHS performed by digital palpation (FHS dig ) was also compared to the gold standard aiming to investigate the accuracy of the traditional method. To our knowledge, this study is the first example of automatic calculation of FHS from TPU images integrated in a medical device that can be used in the clinical routine.
Methods
Patients
The presented work was a prospective cohort study conducted at the Policlinic of Bari in Italy between February 2021 and December 2021. The study obtained ethical approval by the Independent Ethical Committee on December 2020. A nonconsecutive series of uncomplicated singleton term pregnancies (37 wk of gestation or more) in active labor, with fetuses in cephalic presentation and no documented fetal malformations, previous Caesarean section, or contraindications to vaginal birth, were recruited for the purposes of this study. The participating patients underwent the conventional labor management routine according to standard local procedures, and informed consent was obtained prior to enrolment. In particular, the sample size ( n = 40) has been calculated by using the following equation and adding the 10% drop-out rate: <SPAN role=presentation tabIndex=0 id=MathJax-Element-1-Frame class=MathJax style="POSITION: relative" data-mathml='n=(Z2·σ2)/E2′>?=(?2·?2)/?2n=(Z2·σ2)/E2
n = ( Z 2 · σ 2 ) / E 2
, where the z-score corresponding to the level of confidence is Z = 1.96; the standard deviation estimation is σ = 1.7 cm; and the maximum desired distance between the estimation of the manual FHS estimation mean and the automatic one E = 0.55. The mean age of patients was 32.3 (SD = 4.9).
During the second stage of labor, US scans were carried out first for every patient, followed by vaginal inspections immediately after.
An investigator, who was blinded to the clinical findings and not involved in the patient’s clinical management, was responsible for performing the US examination each time.
US system and acquisitions
The US acquisitions were performed using a portable US device consisting of a tablet PC equipped with a 3.5-MHz convex transducer, named SensUS Touch (Amolab srl, Lecce, Italy; https://www.amolab.it/en/obstetrics/accessories/ ).
The medical device was equipped with innovative software developed specifically for the automatic calculation of the FHS from TPU 2D B-mode images. For research purposes, the software was customized to process the images offline, ensuring that it did not influence any decisions regarding labor management.
Each patient underwent the first acquisition session at the beginning of the second stage of labor, and the subsequent scans were performed at different fetal stations, within 1 min after the peak intensity of the uterine contraction.
The number of sonographic scans carried out for each patient ( Table 1 ) depended on the value of FHS detected in the first acquisition and on the total duration of the second stage of labor. The medical staff determined the time interval between subsequent acquisitions to monitor the level of the fetal head in the birth canal throughout the entire labor process. Generally, a US scan was performed whenever the clinician deemed it necessary to visualize the position of the fetal head. To avoid the acquisition of too similar images in different time instants, it is preferrable that two consecutive acquisition slots are separated by at least 2 contractions.
| Cohort ( n .) | 27 | ||
|---|---|---|---|
| Maternal age (y) | 32.3 (4.9) [25.6–36.4] | ||
| Ethnicity | Caucasian | ||
| Epidural | Nulliparous | ||
| Patients with 1 US scan | 12 | 9/12 | 3/12 |
| Patients with 2 US scan | 12 | 6/12 | 10/12 |
| Patients with 3 US scan | 3 | 0/3 | 3/3 |
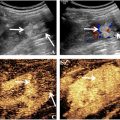
To accurately assess the FHS using US, transperineal acquisition was performed in the midsagittal plane by positioning the probe between the labia to visualize specific anatomical landmarks (the pubic symphysis, the infrapubic plane, and the fetal skull) necessary for the correct evaluation of the FHS [ ]. The FHS was measured as the distance between the ischial spine level and the deepest presenting edge of the fetal skull along the head direction. Since the ischial spine level is not visible on TPU, it was indirectly estimated as the line located 3 cm below the infrapubic line, which represents a fixed anatomical relationship [ ]. The infrapubic line was determined as the perpendicular line to the symphysis axis, passing through the distal point of the symphysis ( Fig. 1 ).

The FHS measurements in this study were recorded in centimeters (cm), according to the classification system proposed by the American College of Obstetricians and Gynecologists [ , ].
The B-mode acquisition was set to a duration of 5 s with a frame rate of 8 frame/s (40 frames per clip). The acquired images were stored in a local database for subsequent offline segmentation.
Assessment of FHS exp by manual segmentation of US images (gold standard)
An expert sonographer, blinded to the algorithm outcome, selected a reference image for each acquisition to perform the image segmentation by manually contouring the anatomical landmark structures required for calculating the FHS. The sonographic assessment of FHS followed the description provided in the previous paragraph, as proposed by Tutschek et al. [ ], and adhered to the ISUOG Guidelines [ ].
The FHS value obtained through manual segmentation of TPU images by the expert sonographer served as the gold standard in this study. The same expert gynecologist conducted both the scans for all participants and the FHS assessments, in two separate study sessions.
Assessment of FHS aut by automatic segmentation of US images (algorithm evaluation)
In the present work, the B-mode images were analyzed and processed using a fully automatic algorithm capable of identifying specific landmarks, namely the pubic symphysis, the infrapubic line, and the fetal skull, to assess the FHS during the second stage of labor. The B-mode images were acquired by expert sonographers following to the ISUOG Guidelines [ ], as previously described.
The algorithm automatically calculated the FHS, as detailed in a previous work [ ]. In particular, the FHS was calculated as the distance along the head direction between the ischial line and a parallel line tangent to the deepest presenting edge of the fetal skull [ ], as represented in Figure 1 .
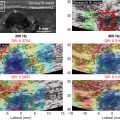
The algorithm for processing the US images (224 × 224-pixel size) involved the following steps ( Fig. 2 ):
- 1)
Image validation. Analyzing the gray level to verify the presence of specific anatomical landmark and discard low-quality images, that is, low differential signal-to-noise ratio: if after applying a low-pass filter, the differential signal-to-noise ratio between the area of interest (i.e., where the symphysis and the head are located) and the background is less than 5, that image is discarded. In particular, the signal-to-noise ratio is defined as the ratio of the average of the object pixels minus the average of the background pixels divided by the standard deviation in that area.
- 2)
Detection of pubic symphysis. Automatically identifying the landmark bone structures derived from the first acquisition session or using pattern tracking methods derived from subsequent acquisition sessions through morphological filters; specifically, the algorithm applies a series of morphological operations to isolate and enhance relevant anatomical structures within the US images:
- I.
Median filter application : This low-pass filter is applied to the US image to attenuate “salt and pepper” noise while maintaining the critical edges necessary for segmentation;
- II.
Morphological evaluation : By applying quantitative cut-off criteria such as pixels clusters area (area must be greater than 500), eccentricity >0.94, or the length of the pubic symphysis bone along its longitudinal axis (between 50 and 100 pixels). If no clusters satisfy these cut-off criteria, the US image is discarded. Moreover, hole-filling operation is applied to ensure a clear and continuous structure.
- III.
Centroid localization : The so-selected pixel cluster is then used to obtain the coordinates of the weighted centroid from the image;
- IV.
Orientation and axis detection : Principal axis of the pubic symphysis is determined from morphological parameters such as orientation, length of the major axis, and pixel area.
- I.
- 3)
Geometrical and morphological check of pubic symphysis. To ensure the accuracy of the segmented pubic symphysis, a validation step is performed. This includes the verification of the structure’s orientation and alignment, using global geometric consistency checks. In particular, the eccentricity of the cluster must be between 0.3 and 0.9, indicating a sufficiently elongated structure. The orientation angle of the major axis should be within 10°–45° relative to the horizontal axis. In addition, the dimension of the cluster area representing the pubic symphysis must be greater than 500 pixels and the mean pixel gray-level intensity must be between 70 and 160 on a scale of 0–255, with a standard deviation not exceeding 40.
- 4)
Fetal head detection. Automatically identifying the landmark bone structures derived from the first acquisition session and using pattern tracking methods derived from subsequent acquisition sessions through morphological filters:
- I.
Median filter application : Step 2-I (above detailed) is applied to both upper and lower fetal head structures;
- II.
Local thresholding : Step 2-II (above detailed) is applied to both the upper and lower fetal head structures, with slight adjustments to the previously established cut-off criteria: selecting the pixel cluster with area larger than 600 pixels, an eccentricity greater than 0.90, and a fetal head structure length within the range of 30 and 70 pixels.
- III.
Distance transform calculation and morphological processing : Step 2-III (above detailed) is applied to both upper and lower fetal head structures.
- IV.
Fusion of segmented regions : Segmented regions of the fetal head are fused using a region-growing algorithm to ensure a coherent and continuous structure, facilitating accurate measurement of the fetal head’s dimensions;
- V.
Radius and center of fetal head: The radius and center of the fetal head are calculated using the Hough Transform.
- VI.
Fetal head direction: An ellipsoid fitting method is applied to estimate the direction of the fetal head as the direction of the longest ellipse axis;
- I.
- 5)
Geometric and pixel-based validation of fetal head . The purpose of this step is to verify that the radius and area of the detected circumference fall within a predefined range of values. In particular, the radius of the detected fetal head circumference must be between 30 and 70 pixels and while the area of the identified region must be greater than 600 pixels. Additionally, the algorithm assesses the gray level values within the circumference on the original US image: if a high-intensity pixel cluster, indicative of bone structure, is found inside a circumference with the same center as the one identified in step 4-V but with a radius reduced by 30% (to minimize border noise), the image is discarded. If no such structure is found, the algorithm stores all relevant information for FHS calculation.
- 6)
Co-registration of coordinates for pubic symphysis and fetal head . Identifying the mutual position of the anatomical references;
- 7)
Identification of reference lines . Identifying the pubic symphysis distal point based on the symphysis recognition performed in step 3, which subsequently allows for the determination of the reference lines, including the infrapubic line and the ischial line. Finally, identifying the line tangent to the most external edge of the fetal skull.
- 8)
FHS. Measuring the distance along the head direction between the inferred ischial spines level and the deepest presenting bony part.