Abstract
Bone infarcts, also called avascular necrosis of the knee or osteonecrosis, are defined as the anoxic death of the bone parts caused by interrupted blood supply and can occur in any bone of the body. It is most associated with trauma, sickle cell disease, steroid intake, alcohol abuse, gout, and liver cirrhosis. The most affected lower limb sites are the head of the femur, medial femoral condyle and talus. We present a case of a 38-year-old female with a history of working long standing hours a day, found to have avascular necrosis of the lateral femoral condyle of the distal femur on magnetic resonance imaging of the knee, which is a rare condition.
Introduction
A reduction in the blood supply to the bone results in bone loss, which causes infarction of the bone and is known as avascular necrosis (AVN). The most common location for the AVN to develop are the head of the femur, medial femoral condyle and talus. The course of AVN progresses through various stages pathophysiologically. Initially, the AVN can be painless, but with the progression of the disease, the pain increases. With further progression of the disease, the joint and the affected bone collapses, which impairs the normal functioning of the joint and causes severe pain. The pain increases with weight bearing. Radiography is the first line of investigation, with magnetic resonance imaging (MRI) being the imaging modality of choice. The management can be medical or surgical depending on the stage of the disease and symptoms of the patient , .
Case presentation
A 38-year-old female residing in a third-tier city in central India came to the orthopedic outpatient department (OPD) with complaints of progressive pain in the lateral aspect of the right knee joint for the past 4 weeks. The pain has progressed to such an extent that it was limiting her daily activities. She works in a beauty parlor and has a profession which involves working with long standing hours of a minimum of 12 hours daily. She is a mother of 2 children, which were through vaginal delivery. There is no history of trauma, alcohol, or drug intake. She is not a known case of the COVID-19 virus and has never taken any steroids. She is not a known case of any systemic disease and has not visited the hospital before for any complaints. The family history is not significant, and she did not undergo any surgical procedures. On examination, she had tenderness in the lateral aspect of the knee joint with some swelling around the joint. The pain was exacerbated as she stood up from a sitting position and on weight-bearing on the affected side. The lab parameters showed an increase in the WBC count, granulocytes and red cell distribution width (RDW), as shown in Table 1 .
| Investigation | Patient | Reference values |
|---|---|---|
| Hemoglobin | 13.4 | 12.1-15.2g/dl |
| MCHC | 35.6 | 32-36g/dl |
| MCV | 87.6 | 80-100fl |
| MCH | 28.3 | 27-33pg |
| Total RBC count | 5.2 | 4.3-6.2 cells/mcl |
| Total WBC count | 9600 | 4000-11000 cells/microliter |
| Total platelet count | 330000 | 150000-400000 g/dl |
| HCT | 42 | 36%-44% |
| Granulocytes | 9.3 | 1.5-8.5 × 10^9/L |
| RDW | 16.7 | 12.2%-16.1% |
| APTT | 28 | 21-35 seconds |
| Prothrombin time | 12.1 | 10-13 seconds |
| INR | 1.0 | <1.2 |
| Urea | 13 | 5-20 mg/dl |
| Creatinine | 0.9 | 0.6-1.1 mg/dl |
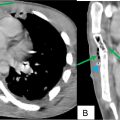
The X-ray showed osteopenia on the distal end of the femur. On the imaging of the knee joint using magnetic resonance imaging, a geographical area of altered signal intensity was visualized in the lateral femoral condyle of the femur having an irregular peripheral rim of hypo intensity on T1 weighted imaging, double line sign and rim sign with bone marrow oedema and minimal joint effusion on T2 weighted imaging and proton density fat-suppressed imaging sequences suggesting avascular necrosis of the lateral femoral condyle as shown in Fig. 1 . The articular cartilage appeared normal.