Chronic low back pain represents a leading cause of global disability, but can often be complex in etiology, with multiple pain generators contributing to patient discomfort. Anterior column low back pain involves the vertebral bodies and discs, with the vertebral body endplates now known to be a significant pain generator. Vertebrogenic low back pain secondary to irritation of the basivertebral nerve presents as axial discomfort, worse with forward flexion, and with concomitant Type I or II Modic changes on MRI. Minimally invasive basivertebral nerve radiofrequency ablation has emerged as an effective intervention for managing anterior column back pain. In this article, the authors present a comprehensive approach to identifying and treating vertebrogenic low back pain through image guided basivertebral nerve ablation. We outline the patient presentation and diagnostic workup, followed by a detailed procedural guide including equipment requirements, technique execution, and potential technical challenges and complications.
Introduction
Chronic low back pain (CLBP) is one of the most prevalent causes of disability worldwide, affecting approximately 30 million people in the United States alone and resulting in substantial healthcare costs and decreased productivity. , , In fact, there is an estimated 60%-85% lifetime prevalence of CLBP in the US, which represents the leading cause of work absenteeism for persons 30-64 years of age.
Axial, or central, lower back pain can be complex to diagnose with multiple pain generators involved, including the facet joints, medial branch nerves, discs, and vertebral bodies. Classifying CLBP into anterior column and posterior column pain can aid in identifying pain generators, though there may be overlapping sources of discomfort. Regarding anterior column axial back pain, nociceptors within the annulus fibrosus of degenerating discs are known pain generators, however, there is emerging evidence suggests that vertebral endplates are a significant source of pain.
The vertebrogenic model of axial back pain is supported by histologic findings of nociceptive nerve proliferation at the vertebral endplates of degenerative discs. The basivertebral nerve (BVN) enters each vertebral body posteriorly through the basivertebral foramen, then arborizes to send nerve fibers to both the superior and inferior endplates. Facet rhizotomy or medial branch radiofrequency ablation addresses posterior column back pain but does not target the BVN. Additionally, open surgical fixation of the lumbar spine in the setting of degenerative disease without an anatomic abnormality or radiculopathy has variable reported pain reduction, limited to 1 year. The reported revision rates range between 9% and 45% due to a variety of etiologies including age, bone density, implant/graft complication, degeneration, and postlaminectomy syndrome. , ,
The central position of the BVN, as well as its role in transmitting pain signals from the degenerating endplates, make it an ideal target for radiofrequency ablation. Basivertebral nerve ablation (BVNA) has emerged as a promising minimally invasive treatment modality for vertebrogenic lower back pain, with a well-studied safety profile and sustained long-term results. ,
Clinical evaluation of the patient with vertebrogenic low back pain
Evaluating vertebrogenic pain requires correlating clinical symptoms with imaging findings indicative of interosseous changes and damage at the vertebral endplate(s). Clinical presentation is commonly axial low back pain generally described as deep, aching, and burning in quality. Some patients may also describe periods of mild pain with occasional flares and can occasionally designate a laterality to their pain. Patients often endorse seated position, forward flexion, and/or change from seated to standing position as aggravating factors. Furthermore, patients may have a documented history of degenerative disc disease with pain that has been refractory to conservative management with nonsteroidal anti-inflammatory drugs, physical therapy, chiropractic therapy, massage therapy, or a multitude of other nerve injections and ablations such as epidural steroid injections (ESI) or medial branch nerve ablation. On physical exam, patients may endorse tenderness to palpation at the vertebral level in question, though this is not specific nor sensitive to the diagnosis of vertebrogenic pain and may reflect paraspinal muscular strain or spasm. The pain may also be reproduced with flexion-based movements where stress is placed on the anterior column during exam. Additionally, documentation of a patient’s Oswestry Disability Index (ODI) is important, and even required by some commercial insurance carriers.
The diagnosis of vertebrogenic pain is confirmed with cross-sectional imaging evidence of degeneration of the intervertebral disc and at the vertebral endplate(s). MRI findings may include disc space narrowing, vertebral body endplate irregularity and sclerosis, as well as subchondral cystic changes. More specific endplate changes are strongly correlated with abnormalities in the adjacent bone marrow, designated Modic changes.
Three types of Modic changes can be evaluated on T1 and T2 weighted MRI, though currently, Modic Type I and/or Type II are necessary to diagnose vertebrogenic back pain. Type I Modic changes demonstrate T1 hypointensity and T2 hyperintensity on MRI, indicating edema and inflammation ( Fig. 1 A-B). Type II Modic changes are characterized by hyperintense signal on both T1 and T2 weighted MRI sequences, indicating fatty infiltration of the bone marrow ( Fig. 1 C-D). Finally, Type III Modic changes are evidenced by endplate hypointensity on T1 and T2 weighted MRI sequences, consistent with osseous sclerosis.

Type I and II Modic changes strongly support a diagnosis of vertebrogenic pain. For patients that cannot obtain an MRI, computer tomography (CT) can adequately detect degenerative changes at the vertebral endplate but are not specific for Modic type changes. Alternatively, nuclear medicine bone scintigraphy with Technetium 99m-methyl diphosphonate (99mTc MDP) followed by single photon emission computed tomography (SPECT) may demonstrate increased radiotracer uptake at the endplates ( Fig. 2 C), consistent with inflammation visualized in Modic I changes ( Fig. 2 A-B).

Indications and contraindications for the procedure
In the United States, basivertebral nerve ablation is generally indicated for chronic lower back pain lasting more than 6 months, failure of nonsurgical management, and evidence on MRI of Modic type I and/or II changes at 1 or more vertebral bodies for levels L3-S1. Contraindications include pregnancy, skeletal immaturity, active local or systemic infection, electronic implants, severe cardiac or pulmonary compromise, ablation zone that is <10 mm from the spinal canal, vertebral compression fracture, prior lumbar surgeries, radicular pain, spinal stenosis, uncorrectable coagulopathy, and active infection. ,
Equipment needed
At the time of this writing, there is currently 1 FDA-approved device for BVNA – Intracept System by Boston Scientific, Minneapolis, MN). This is packaged as a disposable kit with both diamond-tip and beveled introducers, curved cannula assembly which encompasses a J-stylet for maneuverability once inside the vertebral body, straight stylet, and radiofrequency probe.
Procedural steps
The procedure is performed using conscious sedation or general anesthesia per institutional protocol based on patient and/or clinician preference. The patient is placed in the prone position and a “bump” or pillow is placed underneath to achieve optimal lumbar extension. Arms are ideally positioned at the head to avoid C-arm collision in the lateral view.
Sterile preparation of the thoracolumbar region is performed with the area draped in usual sterile fashion. Preprocedural antibiotics are administered, typically 2 grams of IV cefazolin.
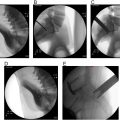
Using fluoroscopic guidance, the targeted spinal segment is identified. To ensure proper selection, the operator counts the lumbar segments from the sacrum, correlating the target level with preprocedural imaging. The C-arm is positioned to visualize the vertebral body in the anterior-posterior (AP) and lateral plane. The C-arm is rotated in the craniocaudal dimension to square off the superior endplate of the target level followed by rotation to obtain an oblique view with the facet centered at the midpoint of the vertebral body, typically 25-50 degrees. The pedicle is identified along the superolateral aspect of the facet and the skin superficial to this point is marked.
Local anesthesia is injected at the skin entry site using 1-2 mL 1% lidocaine, and the local anesthesia is carried down to bone and periosteum with a 3.5-inch 22G spinal needle with administration of an additional 1-2 mL 1% lidocaine. A skin incision is then made with a 10 or 11 blade. Under fluoroscopic guidance the introducer cannula is guided through the skin, subcutaneous tissue, and paraspinal muscle until contact is made with the pedicle periosteum. This can be accomplished with either a beveled or diamond tip straight stylet depending on operator preference.
At this point, adjustments in needle trajectory are made before further advancement into the pedicle. Once an appropriate trajectory is confirmed, the cannula is carefully advanced through the pedicle in a “down the barrel” fashion into the posterior border of the vertebral body ( Fig. 3 A-B). AP, lateral, and oblique views are obtained intermittently to ensure the medial border of the pedicle is not violated. The introducer of the cannula is advanced just past the posterior border of the vertebral body keeping the cannula itself at the posterior border of the vertebral body on lateral view. Subsequently, the introducer needle is removed and is replaced with the curved cannula assembly and nitinol J-stylet.