Presurgical evaluation aims to localize the seizure onset zone (SOZ) for a tailored resection. Interictal [ 18 F]fluorodeoxyglucose PET is now an established test to lateralize and/or localize the SOZ, particularly if MR imaging is negative or if the noninvasive assessment shows discrepancies. PET can show hypometabolic areas associated with SOZ and the potential altered metabolic brain networks. It is very sensitive, and this is increased if images are read coregistered to the patient’s MR imaging. PET hypometabolic intensity and pattern show prognostic value.
Key points
- •
[ 18 F]fluorodeoxyglucose ([ 18 F]FDG) PET is an established imaging modality for the lateralization and the localization of the seizure onset zone (SOZ) during the presurgical evaluation of focal drug resistant epilepsy.
- •
[ 18 F]FDG PET is used to image interictal brain metabolism. The SOZ has reduced metabolism that may extend through the associated brain network.
- •
Interpretation mostly relies on the visual assessment of PET images, which should be superimposed on MR imaging. Analysis can be supported using semi-quantitative statistical methods and new artificial intelligence-based methods.
- •
Results from the literature show that [ 18 F]FDG PET is highly accurate. In temporal and extratemporal lobe epilepsy, [ 18 F]FDG PET adds lateralizing or localizing data in 60% to 90% of patients.
- •
Other PET tracers that focus on the molecular mechanisms of epilepsy are used in research.
Introduction
Epilepsy is a chronic brain disease characterized by recurrent epileptic seizures. Its worldwide lifetime prevalence is estimated to be 7.6 per 1,000 persons. The disease is associated with an increased risk of morbidity and mortality and can severely affect the patients’ quality of life. Epilepsy is categorized into focal, generalized, combined focal and generalized, and unknown types— focal epilepsy being the most frequent type. Etiologic groups include structural (with abnormalities visible on structural neuroimaging), genetic, infectious, metabolic, immune, and unknown.
The clinical management of drug-resistant epilepsy (DRE) is primarily pharmacologic, using antiseizure medication (ASM). However, approximately one-third of the patients experience DRE leading to a low quality of life and poor cognitive and psychosocial outcomes. In patients with focal DRE, surgery has been shown to be superior to medical therapy. If deemed feasible (source of the epilepsy located and outside of eloquent brain area), it can completely eliminate seizures in a variable proportion of patients (approximately 65%) and can also be used as a palliative therapy by decreasing the seizure frequency.
Presurgical evaluation aims to localize the seizure onset zone (SOZ) for a tailored resection. Mandatory investigations are a long-term video scalp electroencephalogram (EEG) to record typical seizures, interictal scalp EEG, and high-resolution MR imaging. The latter is crucial, but even 3T MR imaging only allows visualization of the epileptogenic lesion in approximately 65% of patients with DRE. Therefore, supplementary nuclear medicine imaging procedures, such as ictal single-photon emission computed tomography (SPECT) or PET are used. In particular, [ 18 F]fluorodeoxyglucose ([18F]FDG) PET can lateralize or localize the SOZ in 32% to 77% of cases when the MR imaging is negative (nonlesional patient). PET has a strong prognostic value in MR imaging-positive and -negative patients. Among the latter, PET-positive cases have a better surgical outcome that can be similar to MR imaging-positive cases, for example, in temporal lobe epilepsy (TLE). If noninvasive presurgical assessment does not allow to plan the surgery, invasive video EEG recording with depth electrodes is used (stereo-electroencephalography, [SEEG]) to directly record seizures inside the brain. Electrode placement can be guided by the PET. ,
In this article, we first review the [ 18 F]FDG PET literature for DRE focal epilepsy as it is the only PET examination that is currently and widely used clinically with more than 40 years of experience. We will then examine other PET tracers that are commonly used in research.
[ 18 F]Fluorodeoxyglucose PET
[ 18 F]Fluorodeoxyglucose PET as a Molecular Imaging Technique in Epilepsy
Physiologically, glucose is the primary energy source of the brain, and it is primarily consumed in the synaptic region. PET using a glucose analog, deoxyglucose, labeled with the positron emitter fluorine 18 ( 18 F) is used to estimate the cerebral glucose consumption. The [ 18 F]FDG is trapped in the cell, and at least 30 to 40 min is required to reach a steady state. It is important to note that during that time brain metabolism is assumed to remain stable as it is the case in the interictal state. Imaging protocols are described in the consensus guidelines. , ,
The epileptogenic focus is expected to show reduced metabolism compared to other brain areas, although the pathophysiology has not yet been fully elucidated and appears multifaceted. Hypometabolism usually extends beyond the SOZ and encompasses the entire irritative zone (ie, the SOZ and subsequent neural networks implicated in the generation of interictal paroxysms) but there is a hypometabolism gradient between the non-involved zone and the propagation zones and the epileptogenic focus, as well as, when present, the lesion. Hypometabolism is also influenced by the interval from the last seizure, epilepsy duration and seizure frequency, and ASM.
The kinetics of [ 18 F]FDG appear unsuitable for measuring transient neuronal activity, such as ictal metabolism that usually lasts between 30 seconds and 2 minutes, and is highly hypermetabolic. Another technique, the brain perfusion SPECT, can image ictal state. However, unexpected seizures before interictal acquisition rarely appear to hamper [ 18 F]FDG PET reporting.
[ 18 F]Fluorodeoxyglucose PET Analysis
Interpretation of [ 18 F]FDG PET imaging is mostly based on visual assessment to detect, localize, and quantify altered [ 18 F]FDG uptake suggesting lateralization and localization of the suspected SOZ. PET should be superimposed on a recent MR imaging as this substantially improves the PET anomaly detection rate and allows guiding of MR imaging reinterpretation to identify structural lesions initially overlooked. The yield seems further improved with PET and MR imaging acquired simultaneously through hybrid PET–MR imaging, especially in extra-temporal lobe epilepsy (ETLE). It is of note that hypometabolism outside the suspected SOZ follows the propagation paths; so, a pattern of hypometabolism can be described. For example, in TLE, ipsilateral frontal and insular hypometabolism may be observed because of altered neuronal networks. Thus, the interpretation should be correlated with the results of clinical and electrophysiologic examinations. In addition to analyzing the cerebral cortex metabolism, the basal ganglia, thalamus, and cerebellum metabolisms should also be carefully analyzed; for example, ipsilateral thalamic hypometabolism can be used as an indicative marker of seizure focus lateralization in TLE.
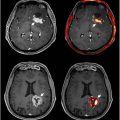
In addition to visual analysis, statistical or quantitative methods have been developed to detect the location of the suspected SOZ. In the research setting, the main tool is statistical parametric mapping (SPM) adapted to single subject analysis. Visual analysis of PET alone and SPM appears complementary, and commercially available alternatives to SPM have also been found useful, , but PET read coregistered with MR imaging seems to outperform SPM. SPM relies on a voxel-by-voxel t-test analysis in a common space between the patient’s PET image and a group of controls. Diagnostic accuracy can be reduced if PET acquisition and reconstruction are different, or if adults are used as controls for children. It outputs a z-score map, which can be thresholded on a specific P -value and a minimal cluster size of voxel to highlight statistically abnormal voxels ( Fig. 1 ). For visually negative PET, the z-score map should be thresholded with liberal P -values and restrictive cluster sizes. Another common useful quantitative analysis relies on asymmetry measurement to lateralize the SOZ. Increasingly complex methods are emerging to improve anomaly detection. For instance, anomaly detection methods based on machine learning or deep-learning have been proposed , including methods to facilitate this detection by enhancing the image quality before conducting any analysis, using anatomy-guided PET reconstruction or deep-learning. In addition, new hardwares such as dedicated brain PET or total-body PET with an improved sensitivity and resolution opens new perspectives for image processing. It facilitates obtaining absolute regional metabolic rate of glucose. Whether it impacts the diagnostic performance and clinical management needs to be further evaluated. ,

Clinical Application
The main clinical indication for [ 18 F]FDG PET is the presurgical work-up of focal DRE, as described in guidelines, in adults and children. This complements electroclinical assessment and structural MR imaging.
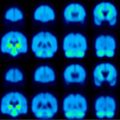
Temporal lobe epilepsy in adults
Among TLE, mesial temporal sclerosis is the primary cause (approximately 60% of cases), visible on MR imaging as hippocampal sclerosis (HS). In [ 18 F]FDG PET, unilateral temporal hypometabolism (as shown in Fig. 2 ) or asymmetric bitemporal hypometabolism is visible in 60% to 90% of the patients with TLE allowing lateralization and aiding localization of the SOZ. , , Interestingly, temporal hypometabolism is reported to be found in positive (95%),equivocal (69%), and negative MR imaging (84%) patients and in drug-resistant TLE. Hypometabolism usually affects the mesial and/or lateral temporal cortex and is usually more extensive than the SOZ. Extratemporal hypometabolism is found in more than one-fifth of the patients, most frequently in the ipsilateral frontal lobe and ipsilateral insula. The distinct pattern of hypometabolism may reflect distinct propagation pathways among TLE, with good concordance with the electro-clinical pattern and SEEG.

The hypometabolism has a prognostic value as a more severe hypometabolism in the SOZ, a pattern with no hypometabolism beyond the SOZ, and the extent of the removed hypometabolic area are associated with a better surgical outcome. This prognostic value does not depend on the MR imaging result as MR imaging-negative/PET-positive cases, concordant with EEG findings, have a similarly good surgical outcome to MR imaging-positive patients, regardless of whether intracranial SEEG is performed. ,
Abnormalities found using [ 18 F]FDG PET scans alone can influence clinical decision-making in approximately 60% of the patients. , Among these patients, it led to the recommendation of direct surgical resection in approximately one-third, help to plan electrode placement for invasive SEEG in approximately half, and one-fifth of the patients were excluded from surgery because it was deemed not feasible (discordance between PET findings with EEG and/or MR imaging findings or diffuse hypometabolism). Additionally, presence of hypometabolism reduced the likelihood to undergo further evaluation.
Extratemporal lobe epilepsy in adults
In ETLE, MR imaging alone is slightly, more often, less contributive than in TLE, but the diagnostic performance of [ 18 F]FDG PET interpreted with MR imaging seems to be similar; PET is reported to be able to localize the SOZ in up to 80% of the patients with ETLE in a prospective study that included patients with frontal (n = 28), parietal (n = 7), occipital (n = 3), multilobar (n = 4), and lateral and posterior temporal (n = 2). The performance of [ 18 F]FDG PET may vary according to the lobe studied, but it is to be noted that the studies that report this did not interpret these images along with MR imaging, and therefore, the values may also be underestimated. For instance, in frontal lobe epilepsy, the second most common form of partial epilepsy, PET interpreted alone was positive in 36% to 52% of MR imaging-negative patients. , In parietal epilepsy, PET alone interpreted using SPM did not lateralize or localize any of the 5 MR imaging-negative patients studied. In occipital epilepsy, PET alone allowed lateralization in 83% but localization in 33% of MR imaging-negative patients. Lastly, in operculo-insular epilepsy, which is difficult to treat, in about half of the patients, FDG-PET alone may show a focal or a regional hypometabolism. It is important to know that the visual assessment of [ 18 F]FDG PET can sometimes be misleading in ETLE as hypometabolism may extend or be more prominent in the temporal lobe. , It is suspected to reflect a remote epileptic dysfunction.
Overall, in ETLE, abnormalities found using [ 18 F]FDG PET scans alone influence decision-making in about half of the patients. Among these, for approximately two-thirds of the patients, this helped to plan electrode placement for invasive SEEG, and one-third of the patients were excluded from surgery because it was deemed not feasible. ,
We now focus on focal cortical dysplasia (FCD), a developmental malformation which is the most studied ETLE etiology using [ 18 F]FDG PET. This malformation, preferentially located in the frontal lobe can be hard to visualize on approximately one-third of the MR imaging. , When coregistered with normal or equivocal MR imaging, PET can show focal or regional hypometabolism corresponding to FCD in more than 80% of the patients, , as illustrated in Fig. 3 . Clinically, PET positivity translates into reducing the need for invasive monitoring but also the resected area through contribution to the delineation of the dysplastic cortex in up to two-thirds of MR imaging-positive cases. With regards to surgical outcome, 2 PET parameters have a positive prognostic value: the presence of a focal hypometabolism in MR imaging-negative patients and congruence of hypometabolism with SEEG.

Pediatric Focal Epilepsy
A recent multicountry guideline consensus underlined the use of [ 18 F]FDG PET in pediatric focal epilepsy. In contrast to adults, focal seizures in children are more likely to originate from areas outside the temporal lobe and from different etiologies, mainly cortical malformations and tumors. PET had a clinical impact on approximately two-thirds of the patients by excluding or modifying surgery.
FCD is the predominant etiology for epilepsy surgery in pediatric candidates. As in adults, [ 18 F]FDG PET can show hypometabolism in equivocal or normal brain MR imaging and can guide MR imaging second reads. , PET can help to delineate the extent of the lesion and guide in depth electrode planning. The surgical outcome was as good for patients who were only PET-positive as for those whose lesions were also MR imaging-visible in a group of 103 patients with 31 children.
TLE in children differs from that in adults. Its prevalence is lower (10%–20% vs 60%), and the most frequent etiologies are tumors and malformations of cortical development and not HS. As expected, in lesional epilepsy, the ability of PET to lateralize and localize (at the lobar level) is high.
Metabolism and Cognitive Function
Interictal [ 18 F]FDG PET metabolism correlates with cognitive functions. In unilateral TLE, extratemporal hypometabolism involving the mesial frontoparietal network and partly overlapping with the default mode network could be associated with cognitive impairment. Interictal hypometabolism in the insular cortex may correlate with emotional symptom or somesthetic symptoms during seizure. In children, aggressive behavior is associated with bilateral anterior frontal and temporal neocortical metabolism abnormalities.
Interictal state [ 18 F]FDG PET metabolism is also predictive of postsurgical cognitive function. In TLE, bitemporal hypometabolism was associated with higher risk of postoperative memory decline. A high asymmetry index between the temporal lobes in left dominant hemisphere patient is associated with a lower postoperative verbal memory deficit.
NONFLUORODEOXYGLUCOSE PET tracers
NonFluorodeoxyglucose (FDG) PET tracers have mainly been explored in research settings. They target various pathophysiologic and neurotransmission pathways.
Gamma-aminobutyric Acid Receptor
Gamma-aminobutyric acid (GABA-A) is the main inhibitory neurotransmitter. The most used PET GABA-A receptor complex ligand is [ 11 C]flumazenil (FMZ) that binds to the benzodiazepine site. The uptake of FMZ is reduced in HS and vascular lesions but can be elevated in and around regions of dysgenesis. A recent meta-analysis showed similar sensitivities and specificities for FMZ and [ 18 F]FDG PET. FMZ PET could add value in TLE with HS to precisely delineate the SOZ in bitemporal epilepsy to confirm the bilateral origin and in unilateral cryptogenic frontal lobe epilepsy.
Alpha-[11C]methyl-L-tryptophan
Alpha-[ 11 C]methyl- l -tryptophan Alpha-[ 11 C]methyl- l -tryptophan tracer uptake seems to be a consequence of the activation of the kynurenine pathway, which allows the synthesis of quinolinic acid, a substance with proconvulsant properties. Interictally, it is elevated only the in epileptogenic tubers of patients with tuberous sclerosis (TSC1 and TSC2) and in dysplastic cortex.
Serotonin Receptor Ligands
The 5-hydroxytryptamine 1A (5-HT 1A ) receptor is a subtype of serotonin receptors located in presynaptic and postsynaptic regions mainly of limbic areas. It can be imaged with the agonists [ 11 C]WAY100635 and [ 18 F]FCWAY or the selective antagonist [ 18 F]MPPF. In TLE, a decrease in 5-HT 1A receptor density in the SOZ is common.
Dopamine Neurotransmission
Dopamine may play a role in the control of the seizure and could also be involved in the pathophysiology of epilepsy. Dopamine neurotransmission was investigated through different targets with generally reduced uptake in various types of epilepsy using [ 18 F]FDOPA, a levodopa analog, [ 18 F]fallypride, a dopamine D2/D3 receptor antagonist, [ 11 C]raclopride, a D2 receptor antagonist ligand, and [ 11 C]SCH23390, a D1-receptor antagonist ligand, and [ 11 C]PE2I a dopamine transporter ligand.
N-methyl-DD-aspartate Receptors
Glutamate is the principal excitatory neurotransmitter in the central nervous system and binds to glutamate receptors including N-methyl- d -aspartate (NMDA). Glutamate exhibits a release pattern that is slightly before, and concurrent with the occurrence of epileptic seizures. [ 18 F]GE-179 binds to the open NMDA receptor ion channel and in patients with focal epilepsies, a global increase as well as some relative focal increases has been demonstrated. ,
α-amino-3-hydroxy-5-methyl-4-isoxazole Propionic Acid Receptors
Binding to the glutamate α-amino-3-hydroxy-5-methyl-4-isoxazole propionic acid receptor (AMPAR) was increased in the epileptogenic focus. [ 11 C]K-2 PET imaging could quantify the density of AMPARs in vivo and localize epileptogenic foci in patients with TLE.
Neuroinflammation
Experimentally, seizures have shown to induce a rapid and significant inflammatory reaction, which peaks 2 wks after the initial insult but persists into the chronic phase. The translocator protein (TSPO) present in glial cells and astrocytes is overexpressed during inflammation. An increase in TSPO PET signal was observed in mesial temporal epilepsy and other focal epilepsies, such as FCD. A recent comparison of the second-generation TSPO PET tracers [ 18 F]DPA-714 and [ 18 F]FDG in presurgical assessments suggested that they could help localize the SOZ in FDG-negative patients.
Synaptic Density
PET tracers that bind to synaptic vesicle glycoprotein 2A such as [ 11 C]UCB-J and [ 18 F]SynVesT-1 were developed to measure the density of synapses in humans. They depicted synaptic loss in the SOZ of patients with TLE with medial temporal lobe sclerosis and FCD type 2.
Summary
Interictal [ 18 F]FDG PET is now an established test for presurgical assessment to lateralize and/or localize the SOZ, particularly if MR imaging is negative or if the noninvasive assessment shows discrepancies. PET can show hypometabolic areas associated with SOZ and the potential altered metabolic brain networks. It is very sensitive, and this is increased if images are read coregistered to the patient’s MR imaging. Analysis can be supported using semiquantitative statistical methods and new artificial intelligence-based methods. Additionally, PET hypometabolic intensity and pattern show prognostic value. Other PET tracers are mainly discussed in terms of their use to study the molecular mechanisms of epilepsy.
Clinics care points
- •
[18F]fluorodeoxyglucose ([ 18 F]FDG) PET should be acquired in the interictal state.
- •
[ 18 F]FDG PET images should be superimposed on the MR imaging images for visual interpretation.
- •
[ 18 F]FDG PET reported performances are particularly high in temporal lobe epilepsy and focal cortical dysplasia.
- •
[ 18 F]FDG PET affects surgical decision-making in about half of the patients.
- •
[ 18 F]FDG PET is most useful in patients with inconclusive or discordant initial noninvasive presurgical evaluations.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree