Central Venous Access Management
Jamie B. Arton
Mitchell Smith
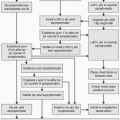
Maintaining lumen patency and preventing catheter-related bloodstream infections (CR-BSIs) or central line-associated bloodstream infection (CLABSIs) are the goals of proper line care for both peripherally inserted central catheters (PICC) and central venous catheters (CVCs). Vascular access devices are cited as the main cause of health care-associated bloodstream infections. Rates of infection vary by line type, insertion location, number of lumens, and tunneling (1).
There are approximately 15 million CVC days in United States intensive care units (ICUs) per year. The average rate of CR-BSIs is 5.3 per 1,000 catheter days or 80,000 infections (2,3). Estimates of associated mortality range from 0% to 35% if the study is controlled for illness severity (4,5,6). The cost of treating a CR-BSI ranges from $34,000 to $56,000 per individual and between $296 million and $2.3 billion for the health care system (5,7,8).
In addition to the ICU setting, central venous access is also frequently used in the outpatient oncology setting, where patients are immunosuppressed secondary to chemotherapy treatment and have a higher likelihood of developing a central line infection. Infections of all types are a significant cause of morbidity and mortality in oncology patients (9). One of the major risk factors determined from multivariate analysis is inflammation at CVC insertion site (10). Gram-positive cocci are 14% more frequently isolated in the blood cultures of neutropenic oncology patients (10).
Herein, the authors discuss the Centers for Disease Control and Prevention (CDC) guidelines for Category I (IA: strongly recommended for implementation and strongly supported by well-designed experimental, clinical, or epidemiologic studies; IB: strongly recommended for implementation and supported by some experimental, clinical, or epidemiologic studies and a strong theoretical rationale, or an accepted practice [e.g., aseptic technique] supported by limited evidence) and Category II (suggested for implementation and supported by suggestive clinical or epidemiologic studies or a theoretical rationale) evidence for the post-insertion care of CVCs (11).
Flushing
Anticoagulants such as heparin are used to maintain the patency of catheters by preventing intraluminal thrombosis. There is a lack of clinical evidence for or against using heparin flushes in central lines, which is noted by many of the evidence-based guidelines for catheter care (12). A systematic review published by Mitchell et al. (12) found weak evidence for the use of heparin flushes in reducing the incidence of catheter occlusion. Risks of using heparin flushes include heparin-induced thrombocytopenia (HIT), allergic reactions to heparin, and chemical contaminants. No current studies have been done that are sufficiently powered to assess the risk of HIT




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree