Central Venous Access—Tunneled
Sidney Regalado
Brian Funaki
Long-term central venous (CV) access devices are composed of tunneled catheters and subcutaneous chest ports. Tunneled catheters are used for weeks to months (or even years) and are most commonly placed for chemotherapy, total parenteral nutrition (TPN), plasmapheresis, and hemodialysis. Implantable subcutaneous ports are used for access if the indication remains for months to years. Most commonly, ports are placed for chemotherapy. Generally speaking, tunneled catheters are easier/quicker to place and exchange but have a higher risk of infection and are more lifestyle-limiting (overall cosmetic appearance and ease of hygiene) when compared to subcutaneous ports. All of these devices can be removed when they are no longer needed (1).
Indications (2)
1. Administration of chemotherapy, TPN, blood products, intravenous medications, and fluids
2. Performance of hemodialysis and plasmapheresis (Chapter 33)
Preprocedure Preparation
Preprocedure preparation is similar to the placement of temporary CV access catheters described in the prior chapter. Notable differences are described below.
1. In addition to local anesthesia, patients often require conscious sedation. Patients must remain nil per os (NPO) for 6 hours, or per institutional protocol.
2. Guidelines to coagulation parameters should be followed to prevent bleeding complications (3). Tunneled CV access and subcutaneous ports are considered to be procedures with moderate risk of bleeding.
a. Routine international normalized ratio (INR) should be obtained in all patients. INR goal is less than 1.5.
b. Partial thromboplastin time (PTT) is recommended in patients receiving intravenous unfractionated heparin. Normal range is 25 to 35 seconds. PTT should be less than 1.5 times control.
c. Platelet count not routinely recommended, but transfusion is recommended for counts less than 50,000 per µL. Others utilize a platelet count ≥25,000 per µL (4).
d. Plavix is withheld for 5 days before procedure. Aspirin not withheld.
e. Low-molecular-weight heparin (therapeutic dose) should be withheld for one dose before procedure.
3. Prophylactic antibiotics before central line placement is controversial because several studies support and refute their utility (5). If prophylaxis is desired for tunneled catheter or port placement, 1 g cephazolin or 600 mg clindamycin can be administered within 45 minutes of skin incision.
Procedure
1. General considerations
a. All tunneled catheters and ports are placed in a fluoroscopy suite.
b. The skin is sterilized with a 2% chlorhexidine-based preparation. Standard surgical scrub protocol for the operator includes hand scrubbing, gloves, mask, cap, and gown.
c. Local anesthesia with 1% lidocaine is used for all line placements.
d. Conscious sedation with fentanyl citrate and midazolam hydrochloride is routinely administered. The nurse must continuously monitor vital signs.
e. Choice of device. As with temporary catheters, the smallest catheter size and minimum number of lumens to satisfy the indication for the access is important to decrease thrombotic complications. Power injectable devices permit their use for contrast injection during computed tomography (CT) examination.
f. Guidance technique
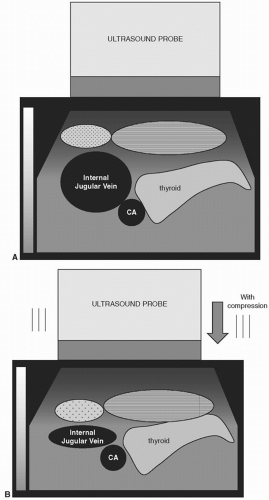
(1) Ultrasound (US) guidance is always recommended for venipunctures.
(2) Fluoroscopic guidance is used for visualization of guidewires, catheters, and venography.
g. Choice of vein
(1) The jugular veins are the preferred access site for tunneled catheters and subcutaneous ports. Subcutaneous ports can be placed through an arm vein, similar to a peripherally inserted central catheter (PICC); however, arm ports are associated with higher risk of complications such as thrombosis (1).
(2) Femoral veins are less optimal sites of venous access because there is an increased risk of infection and worse patency (1,6).
(3) When conventional veins are exhausted, nonconventional access is considered.
2. Tunneled central venous catheters
a. For women with large breasts, the breast should be taped inferiorly to prevent excessive retraction (with cephalad catheter-tip movement) when the patient resumes an upright posture.
b. The placement of tunneled catheters using conventional veins is essentially the same for all indications. Access to the jugular vein is made similarly to nontunneled access (Fig. 29.1A-C).
d. The intended subcutaneous path of the tunnel is anesthetized with lidocaine using a long needle and preferably a single skin entry.
e. A skin nick is made in the chest wall at the desired catheter entry site so as to create a subcutaneous tunnel of 8 to 10 cm in length, and a tunneling device is advanced through this nick toward the neck venotomy site making a gentle curve in the tract (Fig. 29.1E). Some devices have a preformed curve.
f. An appropriately sized peel-away sheath is placed through the jugular access over the existing stiff 0.035-in. wire.
g. The tunneled catheter is pulled through the tunnel so that the proximal retention cuff is at least 2 cm within the entry to the tunnel (Fig. 29.1F).
h. Then the catheter is briskly advanced through the jugular peel-away sheath positioning the tip at the superior vena cava/right atrium (SVC/RA) junction (Fig. 29.1G). Avoid air embolism.
i. The neck venotomy site is closed with skin glue (Dermabond, Ethicon, Mokena, IL) or a suture.
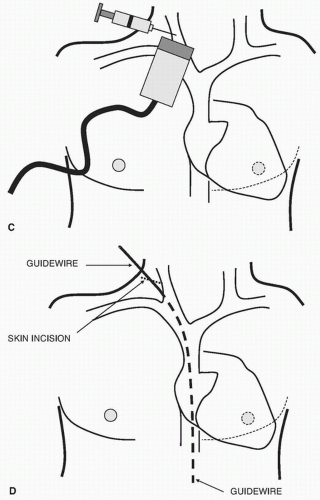 FIGURE 29.1 • (Continued) C: Ultrasound guidance for skinny needle puncture of RIJV. D:
Get Clinical Tree app for offline access
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree


|