Scope of Diagnostic Imaging: Introduction
For almost half a century following the discovery of x-rays by Roentgen in 1895, radiologic imaging was mainly based on plain and contrast-enhanced radiography. Those images were created by exposing film to an x-ray beam attenuated after penetrating the body. The production of x-rays and radiographic images is described in the next chapter. In the recent half century, diagnostic radiology has undergone dramatic changes and developments. Conventional angiography, nuclear medicine, ultrasonography, and computed tomography (CT) were developed between 1950 and 1970. Magnetic resonance (MR) imaging, interventional radiology, and positron emission tomography (PET) were developed later. Conventional radiology, including contrast-enhanced radiography and CT, uses ionizing radiation created from x-ray equipment. Nuclear medicine uses ionizing radiation that is emitted from injected or ingested radioactive pharmaceuticals in various parts of the body. Ultrasonography and MR imaging modalities use sound waves and magnetism, respectively, rather than ionizing radiation.
Radiologic subspecialties have been developed based on organ systems, modalities, and specific fields. Organ-oriented subspecialties of radiology include musculoskeletal, breast, neurologic, abdominal, thoracic, cardiac, gastrointestinal, and genitourinary imaging. Modality-oriented subspecialties comprise nuclear medicine, interventional, ultrasonography, and MR imaging. Specific field subspecialties include pediatric and women’s imaging. Functional and metabolic imaging methods are now being used clinically, with genetic and molecular marker imaging expected in the future.
This chapter is intended to provide an overview of a variety of modalities in diagnostic radiology and basic knowledge regarding radiologic image-based diagnosis. Specific modality settings in each field and diagnostic interpretation for the use of these modalities in evaluating various organ systems are described in subsequent chapters.
Conventional Radiography
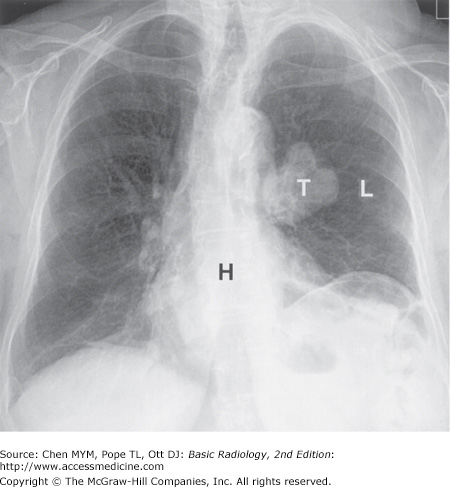
Conventional radiography refers to plain radiographs that are generated when x-ray film is exposed to ionizing radiation and developed by photochemical process. During development, the metallic silver on the x-ray film is precipitated, rendering the latent image black. The amount of blackening on the film is proportional to the amount of x-ray radiation exposure. Plain radiography relies on natural and physical contrast based on the density of material through which the x-ray radiation must pass. Thus, gas, fat, soft tissue, and bone produce black, gray-black, gray, and white radiographic images, respectively, on film (Figure 1-1).
Although other image modalities such as CT, ultrasonography, and MR imaging are being used with increasing frequency to replace plain radiographs, conventional radiography remains a major modality in the evaluation of chest, breast, bone, and abdominal diseases.
Computed radiography (CR) or digital radiography is presently replacing conventional screen-film combination techniques. The most common CR technique, photostimulable phosphor computed radiography (PPCR), uses a phosphor-coated plate to replace the film-screen combination. When a cassette containing the phosphor-coated plate is exposed to x-rays, the phosphor stores the absorbed x-ray energy. The exposed cassette is then placed in a PPCR reader that uses a laser to stimulate release of electrons, resulting in the emission of short-wavelength blue light. The brightness of the blue light is dependent on the amount of absorbed x-ray photon energy. This luminescence generates an electrical signal that is reconstructed into a gray-scale image, which may be displayed on a monitor or printed as a hard copy. Digital images generated from PPCR are capable of being transmitted through a picture archiving and communications system (PACS), similar to other digital images acquired from CT or MR facilities. PPCR is better than plain radiography in linear response to a wide range of x-ray exposure. However, PPCR provides less spatial resolution than plain radiography. Another CR technique that is being developed uses an amorphous selenium-coated plate, which directly converts x-ray photons into electrical charges.
Fluoroscopy uses a fluorescent screen instead of radiographic film to view real-time images generated when an x-ray beam penetrates through a certain part of the body. An image intensifier absorbs x-ray photons and produces a quantity of light on the monitor. The brightness of the image is proportional to the number of incident photons received. Fluoroscopy is a major modality used to examine the gastrointestinal tract. For example, fluoroscopy can be used to follow the course of contrast materials through the gastrointestinal tract, allowing the evaluation of both structure and function. Spot filming or video recording may be used synchronously with fluoroscopy to optimally demonstrate pathology. Fluoroscopy is also used to monitor catheter placement during angiography and to guide interventional procedures. In recent years, digital detectors (such as charge-coupled devices, CCDs) have begun to replace video cameras on fluoroscopy units.
Conventional tomography produces an image of one intended area by blurring structures superimposed on both sides of a focus plane. This technique, however, has been largely replaced by CT.
Mammography uses a film-screen combination technique to evaluate breast lesions for the early detection of breast carcinoma. A mammographic unit is installed with a special x-ray tube and a plastic breast-compression device. A standard mammogram obtains views in two projections, producing craniocaudal (CC) and mediolateral oblique (MLO) images of the breast. Additional images of the breast in other projections, such as mediolateral (ML) views, and using diagnostic techniques such as magnification and/or spot compression views may also be obtained to further characterize potential pathologic findings. Ultrasonography (US) is also used in breast imaging as a complementary modality to further characterize breast pathology. Several image-guided breast interventional procedures, such as preoperative needle placement for lesion localization and core needle biopsy using stereotactic ultrasound or MR guidance, are widely available.
Contrast materials are used to examine organs that do not have natural inherent contrast with surrounding tissues. Contrast media are commonly used to evaluate the gastrointestinal tract, the urinary tract, the vascular system, and solid organs. Contrast media used in MR imaging are described in the MR modality section.
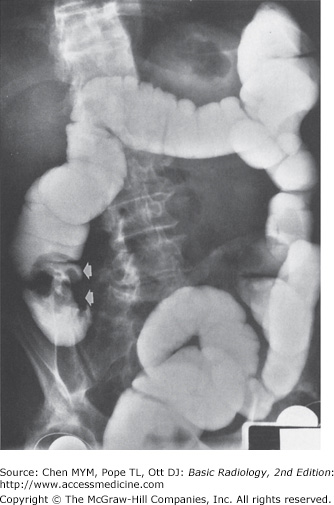
Barium suspension is still used daily in the examination of the gastrointestinal tract. Barium suspension is a safe contrast media that provides high imaging density on upper gastrointestinal (UGI) series, small-bowel studies, and evaluation of the colon. Both single-contrast and double-contrast techniques may be used to evaluate the gastrointestinal tract (Figure 1-2). In the single-contrast study, barium suspension is administered alone. In the double-contrast study, both barium and air are introduced to delineate the details of the mucosal surface, which facilitates the identification of superficial lesions in the bowel lumen. In the UGI double-contrast study, air is introduced into the bowel lumen by administering oral effervescent agents. For double-contrast evaluation of the lower GI tract with barium enema, air is introduced into the bowel lumen via direct inflation with a small pump through a rectal catheter. Small-bowel contrast studies include peroral, enteroclysis, and retrograde techniques. The peroral small-bowel study is performed by feeding barium suspension to the patient and recording the progress of contrast through the small bowel. Enteroclysis is performed by placing a catheter in the proximal jejunum and infusing barium suspension through the catheter. Enteroclysis is preferred for evaluating focal small-bowel lesions or the cause of small-bowel obstructions. Retrograde small-bowel examination is performed by retrograde reflux of barium suspension into the small bowel during barium enema or via direct injection through an ileostomy.
Water-soluble contrast media are commonly used for angiography, interventional procedures, intravenous urography, and enhancement of CT. All water-soluble contrast media are iodinated agents that are classified as high or low osmolar, ionic or nonionic, and monomeric or dimeric in chemical nature. The iodine atoms in contrast medium absorb x-rays in proportion to the concentration in the body when radiographed. The most common water-soluble contrast media are the high osmolar ionic contrast agents (diatrizoate and its derivatives). Low osmolar contrast media include ionic (meglumine ioxaglate) and nonionic (iohexol, iopamidol, ioversol, iopromide) monomers, as well as nonionic dimers (iodixanol). Low osmolar contrast media have an overall lower incidence of adverse reactions, including nephrotoxicity and mortality, than high osmolar ionic agents; however, lower osmolar agents are also three to five times more expensive.
The occurrence and severity of adverse reactions after administration of iodinated contrast material are unpredictable. These reactions are categorized as mild, moderate, or severe based on degree of symptoms. Mild adverse reactions include nausea, vomiting, and urticaria that do not require treatment. The incidence of mild adverse reactions may be less if using a lower osmolality contrast agent. Moderate reactions include symptomatic urticaria, vasovagal events, mild bronchospasm, and/or tachycardia that requires treatment. Severe and life-threatening reactions, such as severe bronchospasm, laryngeal edema, seizure, severe hypotension, and/or cardiac arrest, are unpredictable and require prompt recognition and immediate treatment.
Contrast-induced nephropathy (CIN) is characterized by renal dysfunction after intravenous administration of iodinated contrast material. There is no standard definition of CIN. Findings with CIN include percent increasing serum creatinine from baseline (such as 20% to 50%) or increasing absolute serum creatinine above baseline (such as 0.5 to 2.0 mg/d) within 24 to 48 hours (or in 3 to 5 days). The incidence of CIN is variable. Patients with renal failure or underlying renal diseases are several times more likely to develop CIN than those with normal renal function following the administration of iodinated contrast material.
Water-soluble contrast agents are used in the gastrointestinal tract when barium suspension is contraindicated, when perforation is suspected, when surgery is likely to follow imaging, when confirmation of percutaneous catheter location is necessary, and when gastrointestinal opacification is required during abdominal CT evaluation. Unlike barium suspension, water-soluble contrast agents are readily absorbed by the peritoneum if extraluminal extravasation occurs, but provide less image density. High osmolar water- soluble contrast agents may cause severe pulmonary edema if aspirated. High osmolar contrast agents may also cause fluid to shift from the intravascular compartment into the bowel lumen, resulting in hypovolemia and hypotension, which is less likely to occur with low osmolar water-soluble contrast media.
Intravenous urography (IVU) uses ionic or nonionic water-soluble contrast agents to evaluate the urinary tract. Renal excretion/concentration of intravenously administered iodinated contrast material opacifies the kidneys, ureters, and bladder approximately 10 minutes postinjection. Intravenous urography has been largely replaced over the past decade by unenhanced helical CT evaluation. IVU, however, remains useful for the evaluation of subtle uroepithelial neoplasms and other diseases of the renal collecting system, and it can provide additional information that complements data from cross-sectional image modalities. Additional contrast-enhanced imaging examinations of the genitourinary system include cystography, voiding cystourethrography, and retrograde urethrography to evaluate the bladder and urethra.
Hysterosalpingography is primarily used to evaluate the patency of fallopian tubes and uterine abnormalities in patients with infertility. Hysterosalpingography is also used for postsurgical evaluation and to define anatomy for reanastomosis procedures.
Hysterosalpingography is performed by inserting a catheter into the uterus and subsequently injecting water-soluble contrast medium (some institutions prefer oil-based iodine contrast) to delineate the uterine cavity and the patency of the fallopian tubes. A fluoroscopic spot image is taken once contrast medium fills the uterus and fallopian tubes, but before spillage into the peritoneum. A second image is taken after fallopian tube spillage appears. A transcervical recanalization of obstructed fallopian tube has been introduced to improve the fertility rate.
Angiography is the study of blood vessels following intra-arterial or intravenous injection of water-soluble contrast agents. A series of rapid exposures is made to follow the course of the contrast medium through the examined blood vessels. Angiographic images are recorded by standard or digital imaging, and/or stored digitally.
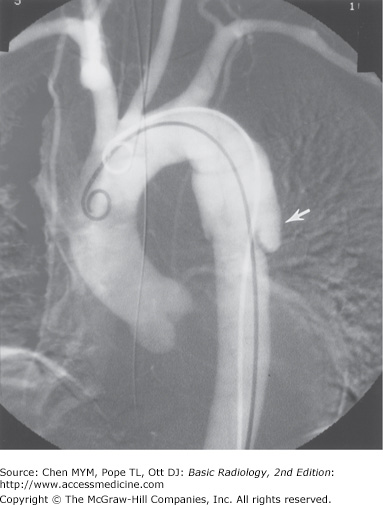
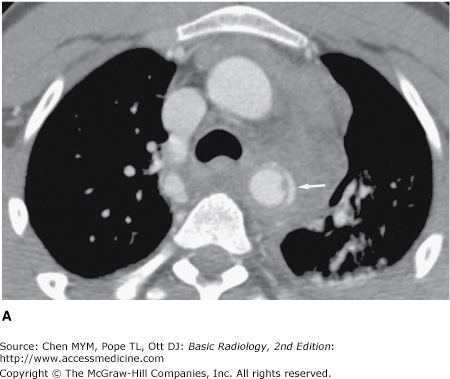
Thoracic aortography is performed when there is suspicion of traumatic aortic injury, dissection (Figure 1-3), or atherosclerotic aneurysm, and to evaluate cerebral and upper extremity vascular disease. Multidetector CT has largely replaced conventional aortography as the initial modality to evaluate aortic trauma (Figure 1-4). Conventional aortography, however, remains important in specific settings, such as planning endovascular stent graft therapy and assessing small branch vessel injuries in stable patients. Abdominal aortography is used to evaluate vessel origins in vascular occlusive disease or prior to selective catheterization. Abdominal aortography is also used for vascular mapping prior to aneurysm repair or other intra-abdominal surgery. Coronary angiography is most commonly performed to evaluate coronary occlusion. Pulmonary angiography is used in patients who are suspected of having pulmonary embolus, especially in the setting of equivocal results on ventilation-perfusion imaging. Inferior venacavography is performed to evaluate for caval occlusion from venous thrombosis, obstruction or compression by retroperitoneal lymphadenopathy, or fibrosis. Inferior venacavography is also performed to evaluate the configuration of the inferior vena cava before filter placement. In recent years, conventional angiography has been replaced by CT angiography and MR angiography.
Less commonly used contrast studies include myelography (evaluating disk herniation and spinal cord compression), fistulography (sinus tracts for abscesses and cavities), sialography (evaluating the salivary glands for ductal obstruction or tumor), galactography (assessing the breast ductal system), and oral cholecystography, cholangiography (evaluating the biliary tree), and lymphangiography (assessing lymph nodes and lymph channels for malignancies).
Computed tomography, an axial tomographic technique, produces source images that are perpendicular to the long axis of the body (Figure 1-5
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree