Radiology of the Breast: Introduction
Imaging of the breast is undertaken as part of a comprehensive evaluation of this organ, integrating the patient’s history, clinical signs, and symptoms. Radiography of the breast is known as mammography, or radiomammography. When used periodically in asymptomatic patients, this is called screening mammography. When imaging is targeted to patients with signs or symptoms of breast cancer, it is referred to as diagnostic breast imaging and usually is a tailored evaluation consisting of some combination of mammography and other techniques described later. Using the integrated approach, it is often possible to make an accurate diagnosis nonoperatively, and treatment may be individualized according to each patient’s needs. The primary purpose of breast imaging is to detect breast carcinoma. A secondary purpose is to evaluate benign disease, such as cyst formation, infection, implant complication, and trauma.
Before the 1980s, when breast imaging was much less widely used, the proportion of surgery for benign breast disease was higher, and treatment for breast carcinoma was initiated at later stages of the disease than at present. Breast imaging has increased the detection of tumors smaller than those found on clinical breast examination and has enabled patients to avoid unnecessary surgery.
The outcome of earlier diagnosis and treatment, however, is yet to be proven. Mortality from breast cancer has remained fairly stable for several decades in spite of the introduction and popularization of screening mammography. Debate continues as to the efficacy of routine breast screening in certain age groups. It is almost universally acknowledged that women over 50 years of age benefit from periodic screening mammography. Several large population studies have shown a decrease in mortality of around 30% in this group. However, controversy continues concerning the value of screening mammography for women under the age of 50 years. Because breast cancer has a lower prevalence in this age group, the impediment to mass screening is largely economic; that is, the number of lives saved relative to dollars spent must be justified. Another difference is that in younger women the breast parenchyma is more often dense and nodular. This condition decreases the sensitivity for detection for carcinoma and leads to more false-negative and false-positive results.
Besides a decrease in mortality, a second benefit of earlier diagnosis is that patients with breast carcinoma are afforded more treatment options; lumpectomy with radiation therapy is an option to mastectomy in many patients.
Mammography has been in common use since about 1980, and breast ultrasonography has been the most often used adjunctive technique during this time. The major contribution of ultrasonography has been its effectiveness in distinguishing cystic lesions from solid masses. Sonography has, therefore, helped to avoid unnecessary surgery, because asymptomatic simple cysts do not require intervention. Ultrasonography, together with mammography, is also used to help characterize solid lesions as benign, indeterminate, or suspicious.
Magnetic resonance (MR) imaging of the breast can be used in selected patients. Image-guided needle biopsy of the breast has become the first-line procedure for diagnosis of indeterminate lesions of the breast, with surgical biopsy being reserved for special cases. Nuclear medicine and contrast injection studies (ductography) are occasionally used under special circumstances with specific indications.
Technique and Normal Anatomy
The film-screen mammogram is created with x-rays, radiographic film, and intensifying screens adjacent to the film within the cassette; hence the term film-screen mammography. The digital mammogram is created using a similar system, but replacing the film and screen with a digital detector.
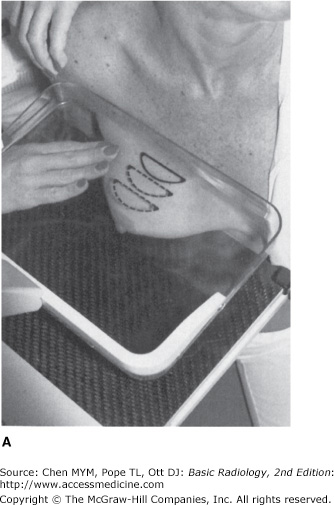
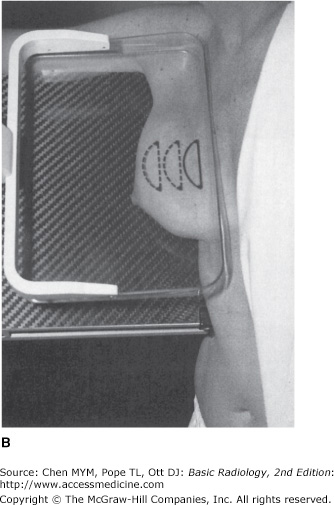
The routine examination consists of two views of each breast, the craniocaudal (C-C) view and the mediolateral oblique (MLO) view, with a total of four films. The C-C view can be considered the “top-down” view, and the MLO an angled view from the side (Figures 5-1, 5-2). The patient undresses from the waist up and stands for the examination, leaning slightly against the mammography unit. The technologist must mobilize, elevate, and pull the breast to place as much breast tissue as possible on the surface of the film cassette holder. A flat, plastic compression paddle is then gently but firmly lowered onto the breast surface to compress the breast into as thin a layer as possible. This compression achieves both immobilization during exposure and dispersion of breast tissue shadows over a larger area, thereby permitting better visual separation of imaged structures. Compression may be uncomfortable, and may even be painful in a small proportion of patients. However, most patients accept this level of discomfort for the few seconds required for each exposure, particularly if they understand the need for compression and know what to expect during the examination. Mammography has proved to be more cost-effective, while maintaining resolution high enough to demonstrate early malignant lesions, than any other breast imaging technique. In its present state of evolution, however, the sensitivity of radiomammography ranges from 85% to 95%.
Sensitivity is limited by three factors: (1) the nature of breast parenchyma, (2) the difficulty in positioning the organ for imaging, and (3) the nature of breast carcinoma.
Very dense breast tissue may obscure masses lying within adjacent tissue. Masses are more easily detected in a fatty breast.
A technologist performing mammography must include as much breast tissue as possible in the field of view for each image. The x-ray beam must pass through the breast tangentially to the thorax, and no other part of the body should intrude into the field of view, so as to not obscure any part of the breast. This requires both a cooperative patient and a skilled technologist. If a breast mass is located in a portion of the breast that is difficult to include in the image, mammography may fail to demonstrate the lesion. Also, because of these practical considerations, routine mammography is not performed in markedly debilitated patients.
Some breast carcinomas are seen as well-defined rounded masses or as tiny, but bright, calcifications, and are easily detected. Others, however, may be poorly defined and irregular, mimicking normal breast tissue. Rarely, still others may have no radiographic signs at all.
For these reasons, it must be remembered that mammography has significant limitations in detection of carcinoma. It cannot be overemphasized that any suspicious finding on breast physical examination should be evaluated further, even if the mammogram shows no abnormality. Occasionally, additional imaging may reveal an abnormality, but if not, short-term close clinical follow-up or biopsy is warranted.
Normal breast is composed mainly of parenchyma (lobules and ducts), connective tissue, and fat. Lobules are drained by ducts, which arborize within lobes. There are about 15 to 20 lobes in the breast. The lobar ducts converge upon the nipple.
The lobules are glandular units and are seen as ill-defined, splotchy opacities of medium density. Their size varies from 1 to several millimeters, and larger opacities result from conglomerates of lobules with little interspersed fat. The breast lobes are intertwined and are therefore not discretely identifiable. This parenchymal tissue is contained between the premammary and retromammary fascia.
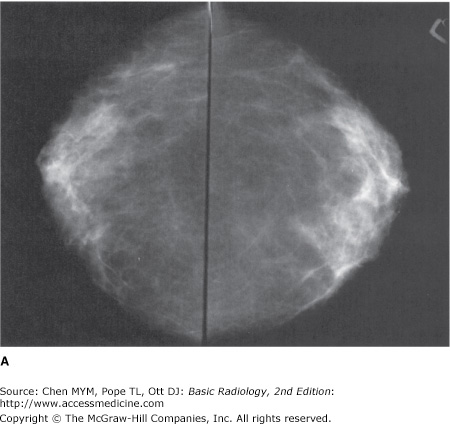
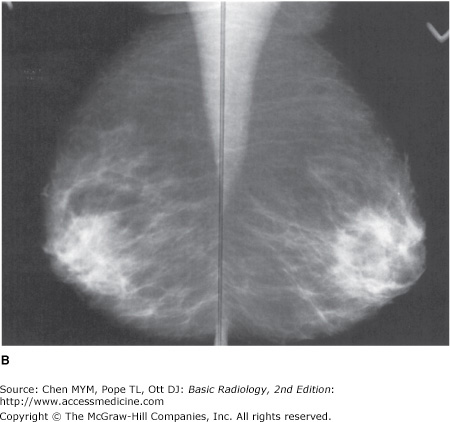
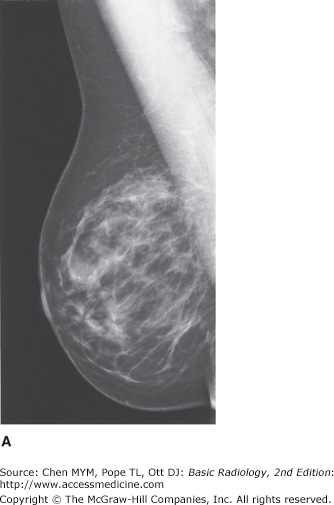
The amount and distribution of glandular tissue are highly variable. Younger women tend to have more glandular tissue than do older women. Glandular atrophy begins inferomedially, and residual glandular density persists longer in the upper outer breast quadrants. However, any pattern can be seen at any adult age (Figure 5-3).
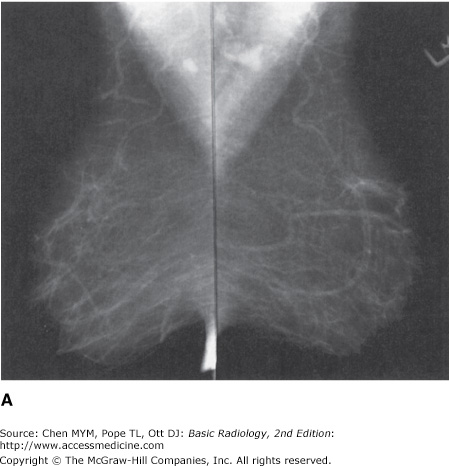
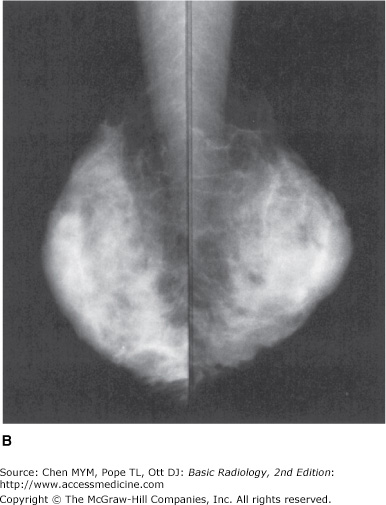
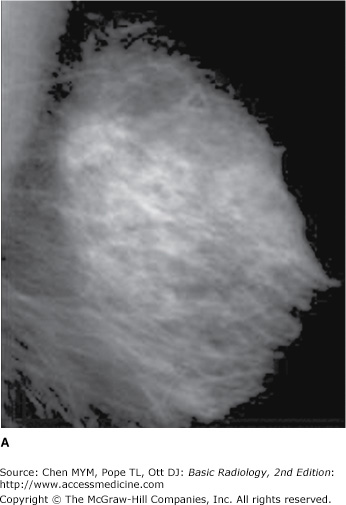
Figure 5-3.
(A) Normal mammograms of fatty breasts. (B) Normal mammograms of dense breasts. Note the extreme variation of the normal breast parenchymal pattern between patients. A small carcinoma would be much more difficult to detect in the patient with dense breasts than in the patient with fatty breasts.
Along with glandular elements, the parenchyma consists of ductal tissue. Only major ducts are visualized mammographically, and these are seen in the subareolar region as thickened linear structures of medium density converging on the nipple.
Trabecular structures, which are condensations of connective tissue, appear as thin (<1 mm) linear opacities of medium to high density. Cooper’s ligaments are the supporting trabeculae over the breast that give the organ its characteristic shape, and are thus seen as curved lines around fat lobules along the skin-parenchyma interface within any one breast (Figure 5-4).
The breast is composed of a large amount of fat, which is lucent, or almost black, on mammograms. Fat is distributed in the subcutaneous layer, in among the parenchymal elements centrally, and in the retromammary layer anterior to the pectoral muscle (Figure 5-4).
Lymph nodes are seen in the axillae and occasionally in the breast itself (Figure 5-4).
Veins are seen traversing the breast as uniform, linear opacities, about 1 to 5 mm in diameter (Figure 5-4).
Arteries appear as slightly thinner, uniform, linear densities and are best seen when calcified, as in patients with atherosclerosis, diabetes, or renal disease.
Skin lines are normally thin and are not easily seen without the aid of a bright light for film-screen mammograms. Various processing algorithms with digital mammography allow better visualization of the skin.
The standard mammogram (along with appropriate history-taking) makes up the entire screening mammogram. The indication for this examination is the search for occult carcinoma in an asymptomatic patient. Physical examination by the patient’s physician, known as the clinical breast examination (CBE), is an indispensable element in complete breast screening. Although the American Cancer Society no longer recommends routine breast self-examination (BSE), particular attention should be paid to lumps identified by the patient as new or enlarging. Such patients should be referred for diagnostic mammography. Table 5-1 includes guidelines for frequency.
Age group | Examination | Frequency |
|---|---|---|
20 to 39 | Breast self-examination | Optional |
Clinical breast examination | Every 3 years | |
40 and older | Breast self-examination | Optional |
Clinical breast examination | Annual | |
Mammography | Annual | |
High risk (>20% lifetime risk) | MRI | Annual |
Moderate risk (15% to 20%) | MRI | Talk with doctor about possible annual examinations |
Risk <15% | MRI | Not recommended |
The diagnostic mammogram begins with the two-view standard mammogram. Additional maneuvers are then used as appropriate in each case, dictated by history, physical examination, and findings on initial mammography. Indications for diagnostic mammography are (1) a palpable mass or other symptom or sign (eg, skin dimpling, nipple retraction, or nipple discharge that is clear or bloody), and (2) a radiographic abnormality on a screening mammogram. Additionally, patients with a personal history of breast cancer may be considered in the diagnostic category.
Other projections, magnification, and spot compression may be used to further evaluate abnormalities. These techniques provide better detail and disperse overlapping breast tissue so that lesions are less obscured.
Patients with breast implants require specialized views to best image residual breast tissue because the implants obscure large areas of the breast tissue with routine mammography. These specialized views (Eklund, “push-back,” or implant displacement view) displace the implants posteriorly while the breast tissue is pulled anteriorly as much as possible.
Growing availability and affordability of computing power has led to the development of computer-aided detection (CAD). CAD utilizes complex algorithms to analyze the data from a mammogram for suspicious calcifications, masses, and architecture distortion. It then flags these areas so that the interpreting radiologist can give these areas special attention. Several studies show increased cancer detection when CAD is applied, and sensitivity and specificity continue to improve as these algorithms are refined.
The indications for ultrasonography are (1) a mammographically detected mass, the nature of which is indeterminate, (2) a palpable mass that is not seen on mammography, (3) a palpable mass in a patient below the age recommended for routine mammography, and (4) guidance for intervention. Ultrasonography is a highly reliable technique for differentiating cystic from solid masses. If criteria for a simple cyst are met, the diagnosis is over 99% accurate. Although certain features have been described as indicative of benign or malignant solid masses, this determination is more difficult to make and less accurate than the determination of the cystic nature of a mass.
A limitation of ultrasonography is that it is very operator-dependent. Also, it images only a small part of the breast at any one moment. Therefore, an overall inclusive survey is not possible in one image, and lesions may easily be missed.
The skin, premammary and retromammary fasciae, trabeculae, walls of ducts and vessels, and pectoral fasciae are well seen as linear structures. The glandular and fat lobules are oval, of varying sizes, and hypoechoic relative to the surrounding connective tissue (Figure 5-5).
Simple cysts are anechoic (echo-free) and have thin, smooth walls. Increased echogenicity is seen deep to cysts (enhanced through-transmission). Most solid masses are hypoechoic relative to surrounding breast tissue.
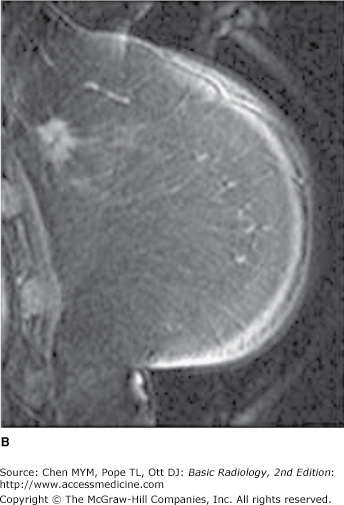
The role of MRI in mammography continues to expand, with common applications including (1) staging of and surgical planning for breast tumors, (2) searching for a primary tumor in patients who present with cancerous axillary lymph nodes, (3) evaluating tumor response to neoadjuvant chemotherapy, (4) differentiating tumor recurrence from posttreatment changes in patients with previous breast-conserving surgery and radiation, (5) screening of high-risk patients, (6) evaluating implants, and (7) evaluating difficult (dense or fibrous) breasts. In addition, the technology for MR-guided breast biopsies is increasingly available.
The patient lies prone on the scanner table, and a specialized coil surrounds the breasts. Depending on the clinical question, a varying number of pulse sequences are performed to evaluate the breasts or the composition of a suspicious lesion. Scan times can range from 30 minutes to over an hour.
MRI can show whether a lesion is solid or contains fat or fluid. Dynamic scanning after administration of intravenous contrast shows whether structures enhance and at what rate. Cancers classically enhance rapidly with subsequent “wash-out.” For instance, a lesion that enhances relatively rapidly on dynamic exam (think neovascularity) is more concerning for malignancy. If more than one suspicious lesion is identified, the relative proximity of these lesions can determine whether a patient would be a good candidate for lumpectomy rather than mastectomy. The wide field of view allows staging by evaluating the axillary and internal mammary nodes. Figure 5-6 shows an enhancing cancerous tumor.
Although MRI is quite sensitive (good for detecting disease), it is relatively nonspecific. This is due to the overlapping imaging characteristics of both benign and malignant processes. Like cancer, some benign breast structures show enhancement, although usually with a slower rate.
Because of the relatively low specificity, screening with MRI is best used in patients with a higher probability of disease. The 2007 American Cancer Society recommendations include annual MRI breast screening of patients with a lifetime risk of 20% or greater.
Tissues are differentiated by their pattern of change on different pulse sequences. The skin, nipple and areola, mammary fat, breast parenchyma, and connective tissue are normally seen, in addition to the anterior chest wall, including musculature, ribs and their cartilaginous portions, and portions of internal organs. Small calcifications are not visible, and small solid nodules may not be detected. Cystic structures are well seen. Normal implants appear as cystic structures with well-defined walls. Their location is deep to the breast parenchyma or subpectoral, depending on the surgical technique that was used to place the implants. Internal signal varies and depends on implant contents, either silicone or saline.
Ductography, or galactography, uses mammographic imaging with contrast injection into the breast ducts. The indication for use is a profuse, spontaneous, nonmilky nipple discharge from a single duct orifice. If these conditions are not present, the ductogram is likely to be of little help. The purpose is to reveal the location of the ductal system involved. The cause of the discharge is frequently not identified. Occasionally, an intraluminal abnormality is seen, but findings have low specificity.
The patient lies in supine position while the discharging duct is cannulated with a blunt-tipped needle or catheter under visual inspection and with the aid of a magnifying glass. A small amount of contrast material (usually not more than 1 mL) is injected gently by hand into the duct. Several mammographic images are then made. The procedure requires about 30 minutes and is not normally painful.
Just deep to the opening of the duct on the nipple, the duct expands into the lactiferous sinus. After a few millimeters, the duct narrows again and then branches as it enters the lobe containing the glands drained by this ductal system. The normal caliber of the duct and its branches is highly variable, but normal duct walls should be smooth, without truncation or abrupt narrowing. With high-pressure injection, the lobules, as well as cystically dilated portions of ducts and lobules, may opacify.
The indications for needle aspiration and biopsy of breast lesions are varied and are variably interpreted by radiologists and referring physicians. Two categories are discussed here.
The first indication is aspiration of cystic lesions to confirm diagnosis, to relieve pain, or both. Nonpalpable cysts require either ultrasound or mammography to be seen. A fine needle (20- to 25-gauge) usually suffices to extract the fluid. The cystic fluid is not routinely sent for cytology unless it is bloody.
The second indication concerns solid lesions. Needle biopsy is used in this case (1) to confirm benignity of a lesion carrying a low suspicion of malignancy mammographically, (2) to confirm malignancy in a highly suspicious lesion prior to initiating further surgical planning and treatment, and (3) to evaluate any other relevant mammographic lesion for which either follow-up imaging or surgical excision is a less desirable option for further evaluation.
Guidance for needle biopsy can be accomplished with stereotactic mammography, ultrasound, and MR. Imaging modality for needle guidance is selected on the basis of lesion characteristics, availability of technology, and personal preference of the radiologist. Ultrasound and mammography are the most commonly used techniques.
Large core biopsy (typically 14-, 11-, or 8-gauge) has been shown to be more accurate for nonpalpable lesions than fine needle aspiration (20-gauge or smaller) and is often combined with vacuum assistance to further increase tissue yield.
Mammographic guidance is most easily and accurately performed with a stereotactic table unit. Lesions of only a few millimeters can be successfully biopsied. With stereotactic tables, the patient lies prone with the breast protruding through an opening in the table surface. A needle is mechanically guided to the proper location in the breast with computer assistance. The entire procedure requires 30 minutes to 1 hour.
When a nonpalpable breast lesion must be excised, imaging is used to guide placement of a needle into the breast, with the needle tip traversing or flanking the lesion. Either ultrasonographic or mammographic guidance can be used, and the choice again depends on lesion characteristics and personal preference. Once the needle is in the appropriate position, a hook wire is inserted through the needle to anchor the device in place. This prevents migration during patient transport and surgery. After needle placement, the patient is taken to the operating theater for excision of the lesion by the surgeon.
When a lesion is excised from the breast, a surgical specimen can be radiographed to document that the mammographic abnormality was removed. This practice is routinely followed with needle-localized lesions, but palpable lesions excised may also be radiographed to confirm that the specimen contains an abnormality that may have been present on the mammogram.
Technique Selection
As with other organ systems, the task of the referring physician with regard to breast imaging is to determine which patients may benefit from these studies and which are the appropriate studies to order. To do this, the physician first categorizes the patient as asymptomatic or symptomatic. (1) Asymptomatic patients: As a group, these patients will benefit from routine screening mammography performed according to published national guidelines. A particular patient may require an individualized program for specific reasons: for example, a 30-year-old asymptomatic woman whose mother died of breast cancer at age 35 may justifiably begin yearly screening mammography. (2) Symptomatic patients: These are women who have any of the following signs or symptoms: a new or enlarging breast lump, skin changes (primarily dimpling), nipple retraction, eczematoid nipple changes, bloody or serous nipple discharge, and focal pain or tenderness. Diagnostic mammography is indicated in these patients. If the patient is under 35 years of age, the examinations may be differently tailored than for older patients. Consultation with the breast imager may be helpful in determining a suitable evaluation plan in any patient for whom the usual guidelines are not helpful.
If a diagnostic study is needed, a standard two-view mammogram is obtained first. The need for further studies will be determined by the results of the mammogram. Whether ultrasonography or another modality is needed is best decided by the person interpreting the films, provided that he or she has the necessary clinical information available. For example, it is imperative that the location and description of a suspected mass be made known to the radiologist so that a specific search can be made for a lesion.