Musculoskeletal Imaging: Introduction
When Wilhelm Conrad Roentgen discovered the x-ray in November 1895, he investigated it thoroughly, testing its ability to penetrate various inanimate objects and observing its effects on fluorescent screens and photographic film. He gazed in amazement at the image of the bones of his own hand as he allowed the new rays to penetrate his flesh. He made a photographic x-ray image of a hand (reportedly his wife’s) and sent prints of it together with his paper describing the new phenomenon to a carefully selected list of scientific colleagues.
By mid-February 1896, Roentgen’s paper had not only been published but also reprinted in other scientific journals including the American journal Science. Scientists everywhere repeated Roentgen’s simple experiments and confirmed the truth of his discovery. Within a year, x-rays were in widespread use for medical purposes—chiefly for imaging of the skeleton.
Since Roentgen’s time, many new imaging techniques have been developed that allow radiologists to see the muscles and other soft tissues of the musculoskeletal system as well as the bones and to evaluate the amount of metabolic activity in the bones and soft tissues. These techniques make skeletal imaging an exciting area of radiology that can enhance patients’ quality of life. The techniques can also be very expensive, however. This chapter is intended to introduce you to musculoskeletal imaging techniques and to suggest efficient ways to use them that will help you to make correct diagnoses without excessive cost. Naturally, the suggestions made in these pages must be tailored to the needs of individual patients.
Techniques
Conventional radiographs are the most frequently obtained imaging studies. They are chiefly useful for evaluation of the bones, but useful information about the adjacent soft tissues may also be obtained. Gas in the soft tissues may be a clue to an open wound, ulcer, or infection with a gas-producing organism. Calcifications in the soft tissues can indicate a tumor, myositis ossificans, or systemic disorders such as scleroderma or hyperparathyroidism.
To get the most information possible from conventional radiographs, you should carefully choose the study to be ordered. At most hospitals and clinics, standardized sets of views have been developed that are routinely obtained together for evaluation of specific body areas in certain clinical settings. It is useful to know what will routinely be obtained when a certain set of films is ordered. Radiographs of the ankle, for example, usually include a straight frontal view of the ankle, a frontal view obtained with approximately 15 degrees internal rotation of the ankle (the mortise view), and a lateral view. There will be some variation among institutions, however. At a minimum, two views at right angles to one another should be obtained when a fracture or dislocation is suspected, because such injuries are notorious for being very subtle or even invisible in one projection, even when they are glaringly obvious in another view (Figure 6-1). Radiographs should be focused on the anatomic area being evaluated, free of overlapping, extraneous anatomy (Figure 6-2). If the knee is the site of trouble, do not order views of the entire tibia and fibula; you will be disappointed with the visualization of the knee. This principle must be abandoned more or less in young children and mentally impaired individuals who may not be able to localize their symptoms well, and also in trauma victims with so many injuries that the relatively minor ones may be overlooked.
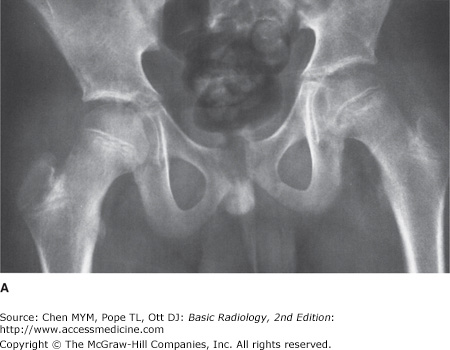
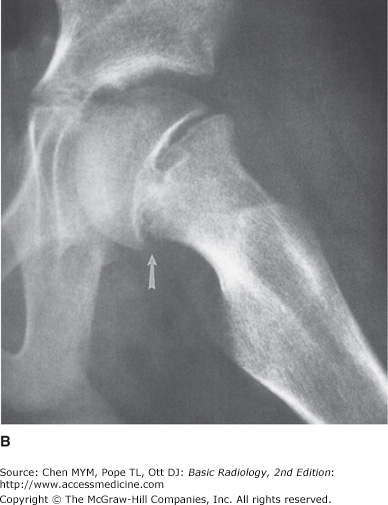
Figure 6-1.
(A,B) Slipped capital femoral epiphysis. (A) Anteroposterior (AP) radiograph of the pelvis. There are signs of a fracture through the physis of the left proximal femur: that femoral epiphysis is less well mineralized than the one on the right, the lucent line demarcating the physis is slightly widened, and the alignment of the edges of the epiphysis and metaphysis is abnormal. These signs are relatively subtle and could be easily missed. (B) Frog-leg lateral view of the left hip. This view, a lateral of the proximal femur, is much more obviously abnormal. Along the posterior edge of the femur, the cortices of the epiphysis and metaphysis should be flush but are instead offset by approximately 5 mm (arrow).
Figure 6-2.
(A,B) Phalangeal fracture. AP (A) and lateral (B) radiographs of the hand. This young man was first evaluated for trauma to the ring finger with frontal and lateral views of the whole hand. On the lateral view, all fingers other than the thumb are overlapped. No fracture was found. (C,D) AP and lateral radiographs of the finger. The patient returned 2½ months later, complaining that his finger still hurt. This time radiographs were coned more closely to the finger and care was taken on the lateral view to image the ring finger separately from the others. In that view the intra-articular fracture of the proximal aspect of the middle phalanx is quite obvious (arrow). It is far more subtle on the frontal view.
In addition, when the radiographs will be studied by a consulting radiologist, it is helpful to provide a succinct yet accurate history pinpointing your clinical concerns. Simply indicating the site of injury will improve the likelihood that a subtle fracture will be discovered.
A conventional radiograph of a normal bone will show a smooth, homogenous cortex surrounding the medullary space. The cortex will be thicker along the shaft (diaphysis) of long bones and thinner in small, irregular bones such as the carpal and tarsal bones and at the ends of long bones (Figure 6-3). Exceptions are the normal roughening of the cortex at tendon and ligament insertion sites and the normal interruption of the cortex at the site of the nutrient arteries. Naturally these occur at predictable places that differ from bone to bone. Within the medullary space of normal bone are trabeculae. These are visible in radiographs as thin, crisp white lines that are arranged not randomly but in predictable patterns that enhance the stress-bearing capability of the bone. It is beyond the scope of this chapter to address the appearance of each bone.
Figure 6-3.
Normal metacarpals. PA radiograph of the second and third metacarpals of a 36-year-old woman. The cortex is thick and homogenously white in the mid shaft of the metacarpal. It becomes progressively thinner as it approaches the ends of the bones. At the articular surfaces, the cortex has been reduced to a thin, yet distinct, white line.
When questions arise concerning whether a particular appearance is normal or abnormal, several solutions are possible. Two books, Keats’s Normal Variants and Kohler’s Borderlands, are very useful in helping to distinguish the normal from the abnormal (see suggested reading). Correlation with the results of the history and physical examination may also be helpful. Finally, comparison with the patient’s prior radiographs or with a radiograph of the opposite extremity may also help (Figure 6-4). Comparison views of the opposite extremity are especially helpful in children, in whom the open physes and accessory centers of ossification may vary considerably from individual to individual but tend to vary less from side to side than among different people.
Figure 6-4.
(A,B) Nutrient canal. (A) PA radiographs of the small finger. The smooth white cortex of the radial side of the proximal phalanx of the small finger is interrupted by a thin, obliquely oriented dark line (arrow). The soft tissues are swollen, and there is tenderness in this area. How can you distinguish this nutrient canal from a fracture? It is in a typical location for a nutrient canal. Its borders are smooth and sclerotic, not jagged. For definitive proof, delve into the patient’s film folder. (B) The same lucency was present 2½ years earlier. In this case, the soft-tissue swelling was due to cellulitis after a cat bite.
Any soft-tissue area that can be pulled away from the skeleton and placed between the compression paddle and detector may be imaged with mammographic technique. In extremity imaging, mammographic technique is occasionally used to search for small calcifications or foreign bodies in the soft tissues.
Fluoroscopy plays an important role in evaluation of joint motion. It is often used by orthopedic surgeons to monitor placement of hardware. It may be of assistance in positioning patients for unusual or difficult conventional radiographic views.
Tomography (either conventional complex-motion tomography or computed tomography [CT]) has two major uses in skeletal imaging. The first is evaluation of fracture fragment position. CT provides excellent delineation of fractures (Figure 6-5). Multislice scanners, which have become commonplace since about 2005, acquire data in blocks and can depict anatomy in any plane with the same resolution and accuracy that previously was possible only in the axial plane. In this way, a fracture may be evaluated in multiple planes of section, usually sagittal and coronal as well as axial. The decision to use CT for fracture evaluation should be based on whether the study will change treatment or will be of sufficient help in operative planning to justify the additional radiation and expense. Scapular fractures, for example, are often treated conservatively, but orthopedic surgeons differ on treatment of fractures that extend into the glenoid or involve the scapular spine. Some believe these benefit from internal fixation; others do not. Tomographic evaluation of these structures will be more useful to a surgeon who would use internal fixation selectively than to one who would use conservative therapy on all scapular fractures.
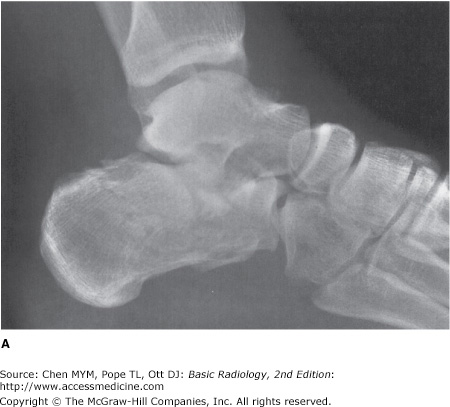
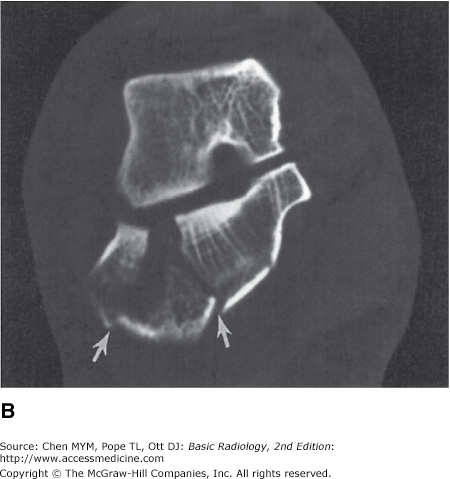
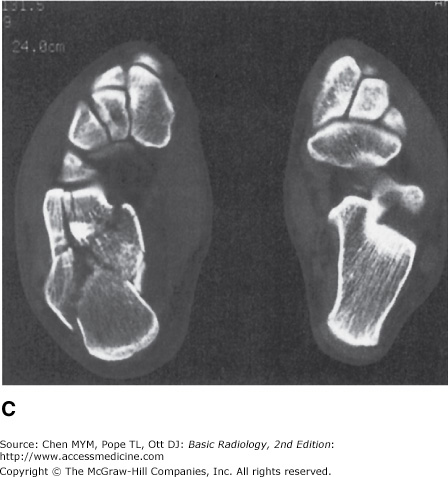
Figure 6-5.
Calcaneal fracture. (A) Lateral radiograph of the foot. The calcaneus of this 27-year-old man has a comminuted fracture that can easily be diagnosed with this conventional radiograph, but the degree of involvement of the articular surfaces is difficult to appreciate. (B) Direct coronal CT image through the posterior and middle subtalar joints demonstrates obliquely oriented fracture lines entering the posterior facet (arrows). There is a gap of approximately 8 mm between the fracture margins, and the lateral fragment has been rotated outward. (C) Axial CT image demonstrates a comminuted fracture of the inferior aspect of the calcaneocuboid joint.
Three-dimensional reconstruction is available with many CT scanners. There is usually an extra charge. This may be justified if it helps the orthopedic surgeon to plan operative intervention and thus decrease the time required for surgery. Three-dimensional images are also useful for teaching purposes, as they can often be understood by less experienced individuals. They do not, however, contain information beyond that available in tomographic images.
The second major use of CT is in evaluation of bone tumors or tumor-like diseases. For this purpose, magnetic resonance (MR) imaging is the principal competing technique. CT is more sensitive than MRI in demonstrating small amounts of calcium and can show early periosteal new bone formation or small amounts of matrix calcification before they may be seen with conventional radiography. This finding can be helpful in narrowing the differential diagnosis of a tumor. MRI can easily obtain images in sagittal and coronal planes, which was once an advantage this technique had over CT. Multislice CT scanners have negated this advantage (Figure 6-6). Before MRI was developed, CT was also used widely for determining the extent of soft-tissue tumors, including osseous tumors that have spread into the soft tissues. MRI, however, is now more often used for staging. Its superior contrast resolution greatly eases the task of determining tumor extent within bone marrow and muscle or other soft tissues (Figure 6-7).
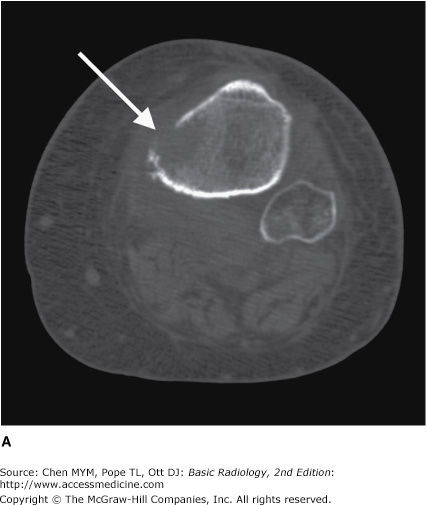
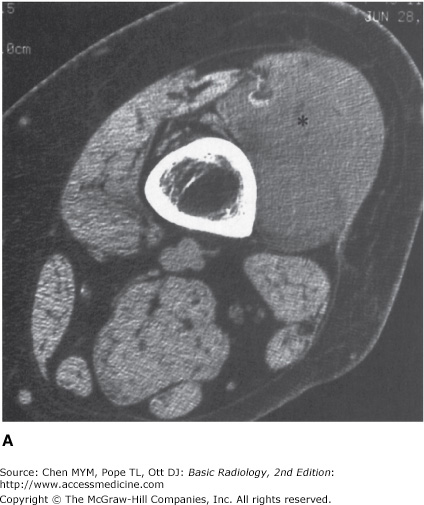
Figure 6-6.
(A) Axial coronal CT image of the left proximal tibia and fibula. The axial image demonstrates destruction of a portion of the medial cortex (arrow), due to an underlying intramedullary lesion of multiple myeloma. (B) Coronal CT image was obtained with a multislice scanner using helical technique. Reconstruction in the coronal plane clearly demonstrates the same area of cortical destruction (arrow). There is also a more distal area of abnormal cortex (short arrow) adjacent to an intramedullary lesion evident by replacement of the marrow fat by soft-tissue density similar to that of the muscles. The reconstruction is quite smooth, differing from the axial image primarily in the presence of tiny stair-step artifacts along curved edges (arrowheads).
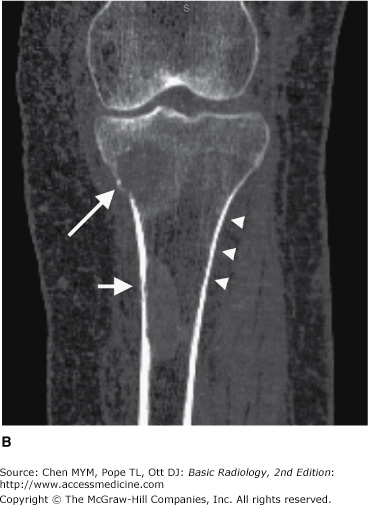
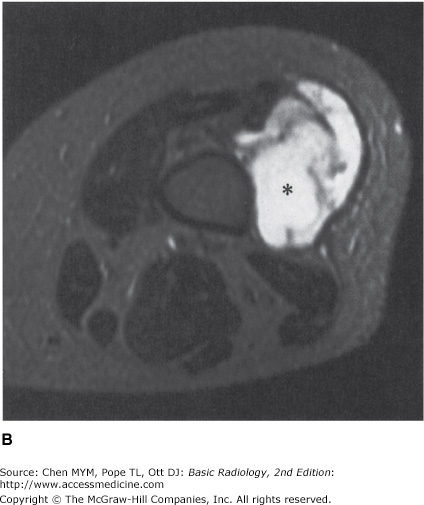
Figure 6-7.
(A) Axial CT image of the distal thigh. This 49-year-old woman complained of a palpable mass in her thigh. It had been present for a year and was painless. The internal architecture of the vastus lateralis muscle (*) is disrupted. The interdigitated fat and muscle tissues evident in the patient’s other muscles have been replaced with a more homogenous mass of decreased attenuation. There is no apparent associated calcification. The mass closely approximates the femur but is not causing osseous destruction. (B) T2-weighted (2500/80) MR image of the thigh at approximately the same level. Although this tumor (*) could be seen on the CT scan, on the MR image it is far more obvious and more easily distinguished from normal tissue. The superiority of MR imaging in detecting soft-tissue neoplasms makes it excellent for determining the extent of primary soft-tissue tumors like this myxoid liposarcoma as well as for evaluating the spread of primary bone tumors into the adjacent soft tissues.
The exquisite contrast of MRI makes it ideal for evaluation of soft tissues. Its most frequent use in skeletal imaging, therefore, is for diagnosis of injuries to muscles, tendons, or ligaments about joints. This superb contrast resolution also makes it very useful for evaluating disorders of the bone marrow including neoplasm, marrow-packing diseases such as Gaucher’s disease, osteomyelitis, fractures that are occult on conventional radiographs, and avascular necrosis. Unfortunately, although MRI is very sensitive to these abnormalities, it is also very nonspecific. Many diseases of marrow cause similar signal alteration. One must then narrow the differential diagnosis based on the distribution of the abnormalities together, the radiographic appearance, and the clinical history. Diffusion-weighted MR imaging may be used to identify areas of an organ that have recently been damaged or injured. Diffusion-weighted MR imaging of the vertebral body may differentiate benign from malignant fracture, although its usefulness is still controversial.
Several nuclear medicine studies are used for skeletal disease. The two most common are the technetium bone scan and fused positron emission tomography and computed tomography (PET-CT). One of several phosphate compounds of technetium-99m is selected for use in bone scan. Methylene diphosphonate (MDP) is used most frequently. If there is a specific anatomic area of interest, images may be acquired over that area at the time the radionuclide is injected, as well as 3 to 4 hours later. The immediate images reflect the amount of blood flow to the area; the delayed images reflect the amount of bone remodeling occurring there.
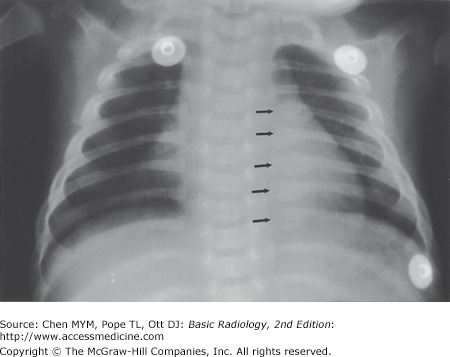
Bone scintigraphy is a sensitive but not very specific technique. Most osseous abnormalities of clinical significance will cause an increase in radionuclide accumulation. Exceptions are destructive lesions that incite little reparative reaction in the host bone or that destroy bone so quickly that it cannot remodel.
Because of their sensitivity and because they provide physiologic rather than anatomic information, bone scans can be used to find abnormalities before they are detectable by conventional radiography. In particular, they are often used for screening for bone metastases in patients with known malignancy. Both multiple myeloma in adults and Langerhans cell histiocytosis in children, however, are notorious for causing no increased accumulation on bone scans. Therefore, in these diseases conventional radiographs or skeletal surveys are better than bone scans for screening for osseous involvement. MR imaging is sometimes also used for screening for myeloma or metastatic disease.
Fused positron emission tomography–computed tomography (PET/CT) combines in a single gantry system both PET scanner and CT scanner, so that images acquired from both techniques can be taken sequentially in the same session and combined into a single superimposed image. Thus, functional imaging obtained by PET, which depicts the spatial distribution of metabolic or biochemical activity in the body, can be more precisely aligned or correlated with anatomic imaging obtained by CT scanning. Other imaging studies may also be fused to combine metabolic information of a nuclear study with anatomic information. For example, a SPECT bone scan may be combined with CT or a PET scan may be combined with MRI.
When tumor or infection is suspected, it is often useful to obtain a tissue sample for cytologic or histologic analysis or for culture. This may be accomplished by means of an “open” procedure in the operating room or a percutaneous needle puncture of the lesion to obtain a cellular aspirate or slender core of tissue. Needle biopsies of palpable lesions do not necessarily need radiologic intervention. When the lesion is not palpable, however, biopsy may be accomplished under fluoroscopic, CT, ultrasound, or MRI guidance.
When skeletal lesions should be biopsied and by whom are important questions that can have a tremendous impact on the patient’s outcome. For example, sarcomas have been reported to grow along the surgical or needle tracks after diagnostic biopsies. Therefore, when planning biopsies of suspected musculoskeletal sarcomas, care must be taken to approach the lesion through a track that can be resected en bloc with the tumor at the time of ultimate excision. These biopsies should always be carried out in close consultation with the surgeon who will be performing the definitive surgery.
When systemic disease such as metastatic carcinoma is the primary consideration, percutaneous needle biopsy is the most efficacious means of making a diagnosis if the lesion is amenable to this procedure. In this setting, the yield of needle biopsy is very good (90% or more of such biopsies yield a positive diagnosis when tumor is truly present) and a negative result is less likely to lead to open biopsy than it would in some suspected primary tumors. Nonetheless, biopsy should still be performed in consultation with the oncologist or other physician giving overall care.
Technique Selection
In general, as in most other organ systems, the radiograph is the initial imaging test after history and physical examination. The selection of subsequent (often more expensive) imaging tests depends not only on medical need but also on a variety of other factors, including availability, expense, and the preferences of the radiologist, clinician, and patient.
Rely on conventional radiography. When a strongly suspected fracture is not identified, you may choose among repetition of conventional radiograph in 7 to 10 days, nuclear medicine bone scanning, and MRI. CT may be substituted for MRI if the latter is unavailable or there are contraindications to its use. If a fracture is noticed and more information is needed concerning the location of fragments, CT is useful.
For local staging of both bone and soft-tissue neoplasms, MRI is the best technique. When a bone tumor is suspected but is not discovered with conventional radiographs, MRI is a useful secondary screening tool.
Symptomatic sites suspected of being involved by metastatic neoplasm are best evaluated initially with radiographs. An overall survey for osseous metastases may be performed by nuclear medicine bone scan or by MRI. Conventional radiography is then used to evaluate sites of possible tumor involvement. Suspected soft-tissue metastases are best evaluated by MRI. PET/CT scans are also useful in staging of many tumors.
Conventional radiographs should be obtained first for suspected osteomyelitis. If these are normal or inconclusive, then MRI, nuclear medicine bone scan, or white blood cell scanning may be helpful. MRI is also useful for detecting the soft-tissue extent of infection and for finding complications including abscesses or necrotic tissue.
Exercise 6-1. Trauma
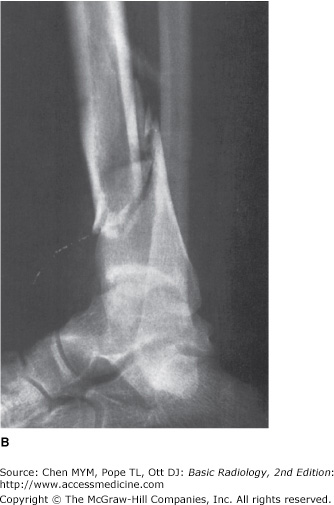
6-1. You are supposed to look at the radiographs for Case 6-1 (Figure 6-8) and call your colleagues in the operating room to describe the fracture. Which of the following statements concerning the fracture would you wish to make?
The distal tibial fragment is displaced 1 cm anteriorly.
There is no comminution of the tibial fracture.
There is slight valgus angulation of the distal tibial fragment.
This is an open or compound fracture.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree