Abstract
Purpose
To assess the efficacy of the gelatin torpedoes embolization technique after lung neoplastic lesions percutaneous radiofrequency ablation (PRFA) to reduce chest tube placement rate and hospital length of stay, and the safety of this embolization technique.
Materials and methods
A total of 114 PRFA of lung neoplastic lesions performed in two centers between January 2017 and December 2022 were retrospectively reviewed. Two groups were compared, with 42 PRFA with gelatin torpedoes embolization technique (gelatin group) and 72 procedures without (control group). Procedures were performed by one of seven interventional radiologists using LeVeen CoAccess™ probe. Multivariate analyses were performed to identify risk factors for chest tube placement and hospital length of stay.
Results
There was a significantly lower chest tube placement rate in the gelatin group compared to the control group (3 [7.1 %] vs. 27 [37.5 %], p < 0,001). Multivariate analysis showed a significant association between chest tube placement and gelatin torpedoes embolization technique (OR: 0.09; 95 % CI: 0.02–0.32; p = 0.0006). No significant difference was found in hospital length of stay between the two groups. Multivariate analysis did not show a significant relationship between hospital length of stay and gelatin torpedoes embolization technique. No embolic complication occurred in the gelatin group.
Conclusion
Gelatin torpedoes embolization technique after PRFA of lung neoplastic lesions resulted in significantly reduced chest tube placement rate in our patient population. No significant reduction in hospital length of stay was observed. No major complication occurred in the gelatin group.
1
Introduction
Percutaneous radiofrequency ablation (PRFA) of lung malignancy is a minimally invasive interventional technique to destroy neoplastic lung lesions . Pneumothorax remains the most common complication after PRFA of neoplastic lung lesions, with an estimated incidence of 9–90 % . Chest tube placement is required to evacuate pneumothorax in 3.3 to 58 % of procedures . Chest tube placement secondary causes discomfort for the patient, increased duration of the procedure, increased risk of complications, prolonged hospital length of stay and costs for the health care system. Therefore, it is important to decrease chest tube placement incidence after PRFA of lung malignancies.
To reduce pneumothorax and chest tube placement incidence after computed tomography (CT) guided percutaneous lung biopsy, numerous studies have been performed to assess the efficacy of some embolization techniques, such as autologous blood patch, hydrogel plug, sodium chloride and gelatin sponge . Successful results have been observed in these various studies, including Renier et al. study who demonstrated the efficacy of a tract embolization technique with gelatin sponge slurry .
Only few studies are available regarding tract embolization technique after PRFA of lung lesions, especially using gelatin sponge [ , ]. Since 2017, the tract embolization technique using gelatin sponge torpedoes has been used at Nantes university dospital (CHU) and Institut de cancérologie de l’Ouest (ICO) in Saint-Herblain (France). The purpose of this study was to evaluate whether tract embolization technique with gelatin sponge torpedoes could reduce the incidence of chest tube placement and the hospital length of stay after PRFA of lung lesions. Moreover, the safety of this embolization technique has also been assessed.
2
Materials and methods
2.1
Study and population
An institutional review board agreement was obtained for a retrospective review of all patient aged of eighteen years old or older who underwent PRFA of lung neoplastic lesion with a multi-tined retractable probe between January 2017 and December 2022.
Exclusion criteria were as follows: no procedure report available, no use of coaxial needle, more than two lesions treated at the same time, use of a different embolization material than gelatin torpedo, embolization of only one needle pathway when two lesions were treated simultaneously. PRFA were performed by seven interventional radiologists, whom were separated into two groups: “experienced” and “not experienced”. The experienced radiologists performed at least fifteen PRFA of lung lesions per year.
2.2
Preoperative consultation and imaging
PRFA was approved by an interdisciplinary tumor board. In order to receive information about benefits and risks of the procedure, each patient underwent a preprocedural consultation. Informed consent of the patient was required before procedure.
Preprocedural thoracic CT scan was performed within two months before PRFA. If a patient required bilateral treatment, lungs were treated separately several weeks apart to avoid major complications.
2.3
PRFA procedure
All procedures were performed under general anesthesia, which allows better control of respiratory movements. Ventilation at very high speed and very low pressure in the airways (jet ventilation) was frequently used. This ventilation technique reduces amplitude of respiratory movements and consequently facilitates the targeting of neoplastic lesion.
Patients were placed in prone, lateral or dorsal decubitus, in order to provide the shortest and safest pathway with the radiofrequency probe through lung parenchyma. Grounding pads were placed on each of the patient’s thighs. Thoracic skin entry point was prepared with antiseptic solutions and surrounded by sterile drapes.
PRFA procedures were performed under CT (Somatom Definition AS 20, Siemens, Germany) or cone beam computed tomography (CBCT) guidance (Allura Xper FD20, Philips, Netherlands). Preliminary imaging was performed in order to determine the most appropriate path up to the lesion. An attempt was made to avoid crossing a vessel, bronchus, scissure or other critical structure. If necessary, biopsies and fiducial insertion were performed under CT guidance, using a coaxial needle, always before PRFA needle placement.
A RF3000™ radiofrequency generator (Boston Scientific Corporation, USA) was used. PRFA was performed with a radiofrequency multitined retractable 15 gauge probe, and 14 gauge coaxial needle (LeVeen CoAccess™, Boston Scientific Corporation, USA).
Coaxial needle was introduced into the lung parenchyma, with regular CT or CBCT imaging to control needle placement. Once needle was properly placed, the stylet was replaced by the radiofrequency probe. Then, the array of tines was deployed and heating process was performed.
2.4
Tract embolization technique
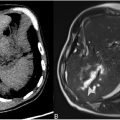
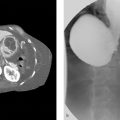
After the heating process was completed, probe was removed from the coaxial sheath. In the control group, the coaxial sheath was removed without any embolization technique. In the gelatin group, needle path was embolized with two gelatin sponge torpedoes of 1 mm large and 10–15 mm length each (CuraSpon® Standard, CuraMedical, Assendelft, Netherlands) ( Figs. 1 and 2 ).


Each torpedo was inserted into the coaxial sheath and pushed with 2 mL of sodium chloride, slowly, without excessive pressure. The first torpedo was placed into lung parenchyma upon contact with the treated area, where the risk of damaging a bronchus or bronchiola was highest with the heating process. The second torpedo was placed at the junction between lung parenchyma and visceral pleura ( Fig. 3 ). The aim was to plug the entire needle path and avoid any potential risk of communication between a bronchus or bronchiola and the visceral pleura.

In the gelatin group, when two lesions were treated at the same time, torpedoes were used for both needle tracks.
2.5
Pneumothorax management
Postprocedural imaging was performed 3 to 5 min after the coaxial sheath removal to assess technical success and look for complications, including pneumothorax. Pneumothorax was defined as presence of air in the pleural space between parietal and visceral pleura. On postprocedural imaging, pneumothorax thickness was classified as mild (< 2 cm), moderate (⩾ 2 and < 4 cm), and severe (⩾ 4 cm). A pneumothorax was considered complete when the pleura was detached over its entire height.
Decision to treat pneumothorax was made jointly by radiologist and anesthesiologist. Chest tube was places in the following situations: poor clinical tolerance after needle removal, great abundance pneumothorax, and rapid increase in size of the pneumothorax.
2.6
Hospitalization
All patients were hospitalized at least until the next day after the procedure. At day 1 or earlier in case of symptoms, a chest X-ray or a CT scan was also performed to look for complications. Upon discharge, patients received explanations of symptoms that should lead to an emergency consultation.
2.7
Safety
All post-PRFA complications were recorded for three months from the day of lung PRFA. The complication that can be caused by gelatin sponge torpedoes technique have been classified in two categories: major complications and minor complications. Major complications were ischemic stroke, myocardial infarction, other peripheral ischemia, pulmonary embolism associated with signs of hemodynamic failure, and death. Minor complications included pulmonary embolism without signs of hemodynamic failure, and bacterial pneumopathy.
2.8
Statistical analysis
Quantitative variables were summarized as means and standard deviations (SD), or medians and interquartile ranges (IQR) if not normally distributed. Categorical variables were presented as effectives and percentages. Tests used to compare the distributions between the two groups were: Student’s t -test for normally distributed continuous variable, Mann-Whitney-Wilcoxon test if not normally distributed and Fisher’s exact test for categorical variables. All statistical tests were two-sided with a type 1 error set at 5 %. Multiple logistic regression analyses were performed to determine whether chest tube placement and hospital length of stay could be independently associated with gelatin embolisation technique. Known or suspected confounders were identified by the clinician group from the literature and used as covariates in the model. We computed the odds ratios (OR) with the corresponding 95 % intervals to answer the study question. Analyses were performed using Rv.4.2.2.
3
Results
3.1
Population characteristics and procedural parameters
Among 157 patients eligible for inclusion, 43 were excluded for the following reasons: five patients had no report available in their medical file, no coaxial needle was used in eight procedures, two patients had more than two lesions treated at the same time, a different embolization material was used in 27 procedures, and only one of the two PRFA paths was embolized in one procedure. Therefore, a total of 114 patients were included, with 42 patients in the gelatin group and 72 patients in the control group ( Fig. 4 ). In our study, a same patient treated twice at two different times was considered as two different patients. Moreover, radiologists using the gelatin sponge torpedoes technique have used it for almost all of their patients.

A total of 126 lesions were treated during 114 procedures, because some patients had two lesions treated during the same procedure (five patients in the gelatin group and seven patients in the control group). Therefore, a comparative analysis of patient characteristics, procedural parameters, pneumothorax management, and hospitalization was performed ( Table 1 ), and a second comparative study of lesion characteristics and data related to lesion treatment was realized separately ( Table 2 ).
| Variable | Gelatin group ( n = 42) | Control group ( n = 72) | p -value |
|---|---|---|---|
| Sex, n (%) | 0.894 | ||
| Male | 22 (52.4 %) | 40 (55.6 %) | |
| Female | 20 (47.6 %) | 32 (44.4 %) | |
| Age, years (± SD) | 65.62 ± 12.62 | 67.62 ± 8.74 | 0.322 |
| Smoking history, n (%) | 21 (50.0 %) | 28 (38.9 %) | 0.337 |
| Emphysema, n (%) | 18 (42.9 %) | 24 (33.3 %) | 0.415 |
| Emphysema gradation, n (%) | 0.706 | ||
| Mild | 12/18 (66.7) | 13 (54.2) | |
| Moderate | 3/18 (16.7) | 6 (25.0) | |
| Confluent | 3/18 (16.7) | 5 (20.8) | |
| Destructive | 0 (0.0) | 0 (0.0) | |
| Homolateral chest surgery, n (%) | 5 (11.9 %) | 4 (5.6 %) | 0.394 |
| Diffuse interstitial lung disease, n (%) | 1 (2.4 %) | 0 (0.0) | 0.784 |
| Homolateral radiation pneumonitis, n (%) | 1 (2.4 %) | 2 (2.8 %) | 1 |
| Center, n (%) | <0.001 | ||
| Institut de cancérologie de l’Ouest | 6 (14.3) | 49 (68.1) | |
| CHU de Nantes | 36 (85.7) | 23 (31.9) | |
| Imaging guidance, n (%) | <0.001 | ||
| CT scan | 32 (76.2 %) | 22 (30.6 %) | |
| CBCT | 10 (23.8 %) | 50 (69.4 %) | |
| Experienced radiologist | 41 (97.6 %) | 52 (72.2 %) | 0.002 |
| Patient position, n (%) | 0.696 | ||
| Prone position | 15 (35.7 %) | 23 (31.9 %) | |
| Lateral decubitus | 1 (2.4 %) | 4 (5.6 %) | |
| Supine position | 26 (61.9 %) | 45 (62.5 %) | |
| Jet ventilation, n (%) | 31 (77.5 %) | 48 (67.6 %) | 0.375 |
| Biopsy during procedure, n (%) | 10 (23.8 %) | 19 (26.4 %) | 0.935 |
| Fiducial during procedure, n (%) | 2 (4.8 %) | 3 (4.2 %) | 1 |
| Pneumothorax, n (%) | 34 (80.9 %) | 51 (70.8 %) | 0.402 |
| Chest tubes, n (%) | 3 (7.1 %) | 27 (37.5 %) | 0.001 |
| Pneumothorax maximum thickness, mm [IQR] | 7.5 [4.00–12.75] | 13.00 [6.5–22.00] | 0.006 |
| Pneumothorax grade, n (%) | 0.028 | ||
| Mild | 31/34 (91.2 %) | 35/51 (68.6 %) | |
| Moderate | 3/34 (8.8 %) | 9/51 (17.6 %) | |
| Severe | 0/34 (0.0) | 7/51 (13.7 %) | |
| Complete pneumothorax | 5/34 (14.7 %) | 19/51 (37.3 %) | 0.05 |
| Chest tube duration, days [IQR] | 3.00 [3.00–5.50] | 1.50 [1.00–2.00] | 0.044 |
| Hospital length of stay, days [IQR] | 1.00 [1.00–2.00] | 1.00 [1.00–2.00] | 0.345 |
| Hospital length of stay > to 24 h, n (%) | 18 (42.9 %) | 24 (33.8 %) | 0.447 |
| Hospitalization within 3 months following PRFA, n (%) | 12 (29.3) | 13 (18.3) | 0.269 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree