This review focuses on the critical role of MR neurography (MRN) in diagnosing and managing peripheral nerve injuries (PNIs). It emphasizes the ability of imaging to differentiate injuries that may heal spontaneously from those requiring surgery, using classification systems like Neuropathy Score Reporting and Data System with imaging findings corresponding to established electrodiagnostic grading systems. MRN also evaluates skeletal muscle denervation and is useful for differentiating pre-ganglionic from post-ganglionic traumatic injuries. MRN is an integral component of optimizing care for patients with PNI.
Key points
- •
MR neurography (MRN) is key in diagnosing nerve injuries, evaluating severity, and guiding treatment.
- •
MRN detects acute (T2 hyperintensity) and chronic (fatty replacement) denervation, aiding prognosis.
- •
Classification on MRN utilizes imaging-based grading systems like the Neuropathy Score Reporting and Data System (NS-RADS), which correspond with electrodiagnostic grading systems (Seddon and Sunderland) to categorize the severity and guide management of nerve injuries.
- •
MRN plays a key role in the differentiation of pre-ganglionic from post-ganglionic injuries and informing surgical versus conservative treatment pathways.
Introduction
Peripheral nerve injuries (PNIs) encompass a wide range of pathology that can be broadly classified by mechanism, ranging from entrapment and compression-related injury to traumatic or iatrogenic injury. In addition to identifying the site of nerve injury and etiology, grading the severity of peripheral nerve injuries is vital to guide clinical management, as low-grade injuries may improve over time with expected nerve regeneration while high-grade injuries require prompt diagnosis and operative management for optimal functional recovery.
The prevalence of traumatic peripheral nerve injury has been reported in up to 3% of patients admitted to Level 1 trauma centers, and up to 5% when plexus and nerve root injuries are included. In a 2008 population-based analysis of insurance claims data mined using ICD-9 codes, PNIs were most frequently associated with crush injuries (⁓2%) and joint dislocations (∼1.5%). PNIs were observed with similar incidence between men and women (50.1% men vs 49.9% women) and occurred with similar frequency across all age groups (ranging from 16.6% to 24.2% in all age groups aside from patients over the age of 65 years who accounted for only 0.2% of injuries).
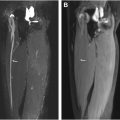
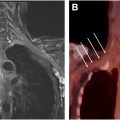
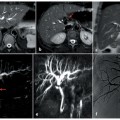
More broadly, traumatic PNI can occur with penetrating trauma, where nerve laceration is a concern, or with blunt trauma such as with motor vehicle collisions, in which case injuries occur due to a stretch/traction mechanism or compression by regional hematoma or fracture ( Figs. 1 and 2 ). Furthermore, in a more chronic setting, entrapment of a peripheral nerve can be observed at specific known anatomic locations, called tunnels, or be related to posttraumatic scar tethering or iatrogenic entrapment. Iatrogenic PNI may also be traction-related from patient positioning under anesthesia or over-enthusiastic retraction of a nerve in an effort to protect it from the surgical field; nerves may be inadvertently lacerated or sutured or may suffer postsurgical entrapment due to scar/fibrosis or regional hardware. Lastly, terminal nerve endings in amputated limbs may undergo disorganized regeneration and form painful end-bulb neuromas, the incidence of which can be minimized if the surgeon embeds the nerve stump within muscle. ,


Imaging of PNI may be performed by MR neurography (MRN) or ultrasound. These modalities are complementary and have shown similar diagnostic accuracy for many peripheral nerves, although there are cases where one modality may be superior to another. MRN is favored for deep-seated anatomy such as the lumbosacral plexus, while ultrasound may be preferred in the setting of hardware near the nerve of interest, which may cause susceptibility artifact and limit evaluation with MRN. In the perioperative setting, ultrasound may also be used to mark the site of abnormality on the skin, providing a landmark for the surgeon and optimizing the surgical approach, and intra-operative ultrasound can also be used for localizing pathology. Major limitations of ultrasound include its operator-dependence and difficulty or inability to image certain deep nerves due to lack of penetration or obscuration of the ultrasound beam by cortical bone.
Peripheral nerve anatomy and signs of injury
Peripheral nerves are composed of multiple individual axons (1–3 in small sensory nerves, up to 200 in large nerves), with each individual axon covered in a myelin sheath and organized into bundles termed (secondary) fascicles, which are surrounded by a thin layer of connective tissue termed perineurium, with endoneurial connective tissue and endoneurial fluid in between the individual axons. Multiple fascicles are bundled together to form the nerve proper, which is surrounded by a thicker layer of connective tissue called the epineurium. Between perineurium-covered fascicles, an inner epineurium containing sparse fat allows for small intra-neural vessels supplying the nerve, while the outer epineurium forms the outermost layer of the nerve ( Fig. 3 ). At MRN, current resolution allows visualization of the secondary fascicle, with the perineurium and the epineurium nearly imperceptible unless pathologically thickened, while individual axons, myelin sheath, and endoneurium are not discretely resolved.

Normal peripheral nerves on high-field strength MR demonstrate signal that is iso-intense to slightly hyperintense to skeletal muscle on fluid-sensitive, T2 weighted fat suppressed sequences, and hypo-intense on T1 or intermediate-weighted/proton-density (PD) sequences. They have a fascicular architecture that is visible at MRN with the exception of smaller branch nerves that may appear as a single “fascicle”. Normal peripheral nerves are accompanied by arteries and veins in many locations and are surrounded by thin perineural fat which forms a “fat plane” in which the nerve can be found with good reliability ( Fig. 4 ). Nerve caliber is normally similar to the neighboring artery, and tapers from proximal to distal (with the exception of the dorsal root ganglion and short segments within the brachial and lumbosacral plexi where nerve contributions converge before separating into their discrete branches).

PNIs are identified at MRN by the presence of primary nerve signs that include abnormal increased signal, increased caliber (nerve enlargement or “thickening”), loss of fascicular architecture, abrupt course deviation, effacement and/or scarring with hypointense signal of perineural fat, and with loss of continuity in nerve transection. , There are also secondary effects of PNI that involve the innervated muscles.
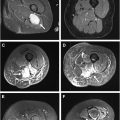
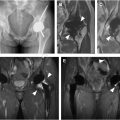
Skeletal muscle denervation is an important secondary finding at MRN, which can aid in assessing the severity of PNI. Normal skeletal muscles are hypointense to fat on T1 and intermediate-weighted or PD images, and slightly hyperintense to fat on fat-suppressed T2-weighted sequences, with feathery interspersed fat within the muscle belly. Acute denervation will manifest as signal hyperintensity diffusely throughout the muscle belly (except in the case of muscles with dual innervation, where only the involved portion of the muscle will be hyperintense). Over time, as denervation becomes chronic, loss of muscle bulk and replacement of normal muscle tissue by fat will be seen. Chronically denervated muscle will demonstrate increasing signal hyperintensity on T1/PD-weighted sequences and hypointensity on fat-suppressed T2 sequences due to increasing fat content. Acute and chronic denervation changes may be seen together, where T2 fat-suppressed sequences will continue to demonstrate diffuse signal hyperintensity with decreased muscle size related to loss of bulk.
As denervation progresses from acute to chronic, muscle tissue undergoes changes in discrete stages ultimately leading to loss of function. In the acute stage of denervation, the fibers undergo immediate loss of function accompanied by weight loss and atrophy of muscle fibers. The second stage consists of further muscle atrophy and loss of organization in the sarcomeres, and the third stage, typically lasting much longer than the initial stages, includes replacement of muscle fibers by fibrotic and fatty tissue. While denervated muscle is still capable of regeneration and restoration of function in the acute and subacute phases, corresponding to the first 2 physiologic stages, once muscle tissue is fatty replaced, there is minimal ability to regenerate.
Classification of peripheral nerve injury
Peripheral nerve injury is classically graded by electrodiagnostic tests using the Seddon and Sunderland classification systems. , Seddon’s classification originally separated PNI into neurapraxia, axonotmesis, and neurotmesis, with Sunderland further classifying neurapraxia as grade I, separating axonotmesis into several grades (II–IV) depending on the anatomic level of involvement, and neurotmesis classified as grade V. A recent MR imaging scoring system Neuropathy Score Reporting and Data System (NS-RADS) was introduced in 2022 and includes a scoring system for PNI (NS-RADS Injury, or NS-RADS I) which parallels the Sunderland Classification. NS-RADS was found to have high inter-reader agreement (k 0.96) as well as high diagnostic accuracy for separating mild from severe categories of nerve abnormality (88%–97%), although these statistics also included other nerve lesions in the scoring system such as entrapment, diffuse neuropathy, and neoplasm and assessment was made by musculoskeletal fellowship-trained radiologists with several years of experience interpreting MRN. NS-RADS has yet to be validated on a broader scale. ,
NS-RADS-I classes, their corresponding Seddon/Sunderland Classification and pathophysiology as well as brief notes on electrodiagnostic examination findings and healing potential are described in greater detail later, according to whether nerve injuries require operative management or monitoring for signs of nerve regeneration, a key distinction for radiologists to make.
Non-operative Management (Spontaneous Recovery Occurring Within 12 Weeks)
Sunderland Grade I injury corresponds to neurapraxia and is equivalent to NS-RADS-I-1. In this grade of injury, there will be a conduction block on electrodiagnostic examinations; neural injury involves the myelin sheath and is transient. At MRN, the radiologist may see focal signal hyperintensity within the nerve, without corresponding muscle denervation ( Fig. 5 ). Occasionally, Sunderland Grade I injuries may have a normal appearing nerve at MRN.