Clinical Examples and Scenarios
Kavitha M. Chinnaiyan
Laxmi S. Mehta
CASE 1: LAD Disease With Cardiac Catheterization Correlation
A 58-year-old woman with hyperlipidemia, hypertension, family history of premature coronary artery disease (CAD), and morbid obesity presents with chest pain of 3 weeks’ duration. This pain is described as a left-sided chest pressure radiating to the left arm, shoulder, and jaw of moderate intensity and associated with diaphoresis and shortness of breath. These episodes occur with minimal exertion and resolve with resting. She undergoes a dipyridamole-induced stress myocardial perfusion imaging test that does not reveal perfusion defects. She is referred for coronary CT angiography.
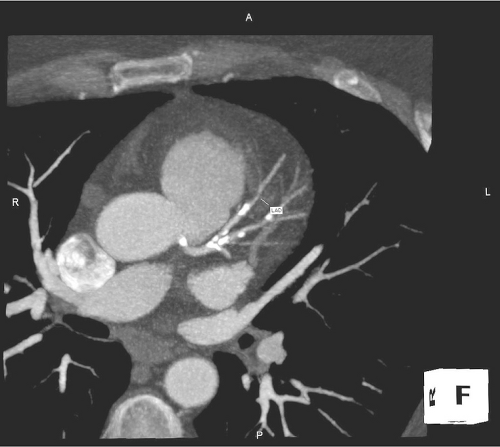
Coronary CT angiography (CTA) reveals a high calcium score (246 Agatston units). In the mid-segment of the LAD, severe (nearly 80%) stenosis is appreciated (Figures C1.1 and C1.2). The patient subsequently undergoes cardiac catheterization and coronary angiography.
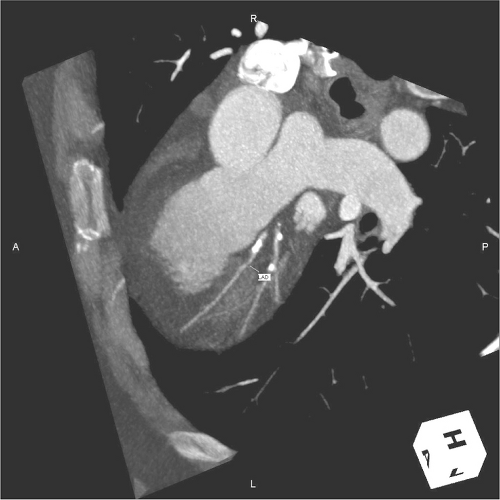 FIGURE C1.2 CT angiogram with LAD rotated anteriorly. The LAD lesion is visualized well. LAD, left anterior descending artery. |
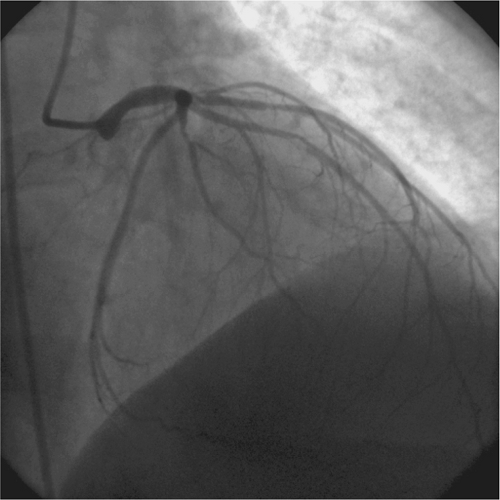
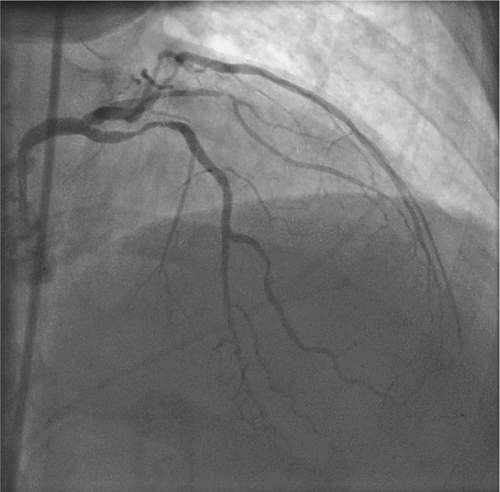
Coronary angiography (Figures C1.3 and C1.4) confirms severe concentric stenosis of the mid LAD (Cine C1.1 and C1.2). Percutaneous intervention is performed with placement of a drug-eluting stent and a decrease of the lesion from a severity of 80% to 0%, with excellent final anatomic results and no complications. She returns for follow-up 3 weeks later with a significant improvement in symptoms and resolution of chest pain.
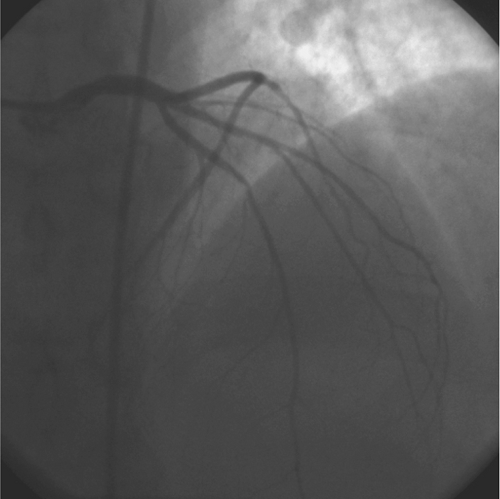 FIGURES C1.3 and C1.4 Coronary angiography of the left coronary system, right anterior oblique cranial view. |
Video Clips: C1.1 and C1.2 Coronary angiography of the left coronary system.
CASE 2: Effect of Overlying Calcium—Intravascular Ultrasound Correlation
A 69-year-old woman with hypertension and hyperlipidemia presents with palpitations of 2 months’ duration. She reports that these episodes occur with her regular water exercises and are associated with symptoms of dyspnea, lasting a few minutes each time. There are no episodes at rest. She undergoes an exercise myocardial perfusion imaging study. At stage II of the Bruce protocol, she is found to have multiple premature ventricular beats and a six-beat salvo of nonsustained ventricular tachycardia at a rate of 150 beats per minute. The test is terminated. The perfusion imaging study is negative at the low workload. She is referred for coronary CT angiography for evaluation of a possible ischemic substrate for the arrhythmia.
Calcium score on CTA is high, with dense calcification present in the LAD. The ostial LAD is obscured by calcified plaque, and luminal stenosis is thought to be 40%–50% in severity (Figures C2.1 and C2.2). However, because of difficulty in accurate interpretation, the patient undergoes coronary angiography and intravascular ultrasound (IVUS) for further characterization of the LAD lesion.
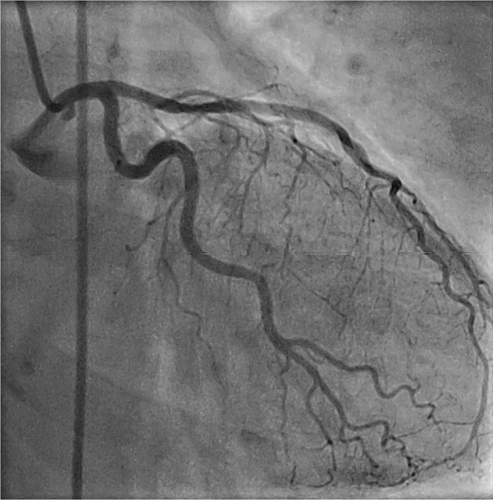 FIGURE C2.2 Coronary angiography, right anterior oblique caudal view reveals only mild disease in corresponding areas. |
Coronary angiography and intravascular ultrasound reveal mild disease in this segment. The patient is reassured and started on beta-blocker therapy for palpitations.
See Cine C2.1: Intravascular ultrasound of proximal left anterior descending artery.
CASE 3: Patent Intracoronary Stent
A 40-year-old male with hypertension and recent inferior myocardial infarction treated with primary angioplasty of the right coronary artery presents with recurrent chest pain radiating to the back. An urgent “triple-rule out” was ordered to evaluate for aortic dissection, an acute pulmonary embolism, or recurrent coronary artery disease. CT was negative for acute pulmonary embolism or aortic dissection.
Coronary CTA reveals a patent stent in the mid-right coronary artery (RCA). Distal to the stent, there is mild atherosclerotic disease with a severity of 20%–25% (Figures C3.1 and C3.2). The patient is medically treated and discharged in stable condition.
 FIGURE C3.1 CT angiogram, anterior view. This displays the stent in the mid-RCA. Contrast is seen within the stent, indicative of a patent stent. RCA, right coronary artery. |
CASE 4: Three-Vessel Disease With Cardiac Catheterization Correlation
A 60-year-old woman with hypertension and atypical chest pain undergoes a stress myocardial perfusion imaging study. The myocardial perfusion image (MPI) reveals inducible perfusion defect involving the apex and the inferoapical area. The patient then undergoes a CTA to delineate the underlying coronary anatomy.
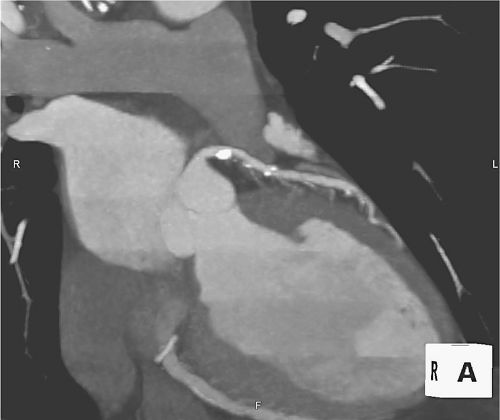
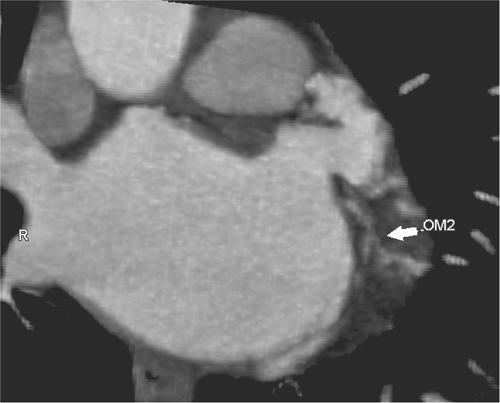
On CTA, calcium score is elevated at 117 Agatston units. Severe (greater than 70%) disease is appreciated in the proximal LAD, the first obtuse marginal branch of the left circumflex artery, and the distal right coronary artery (Figures C4.1 and C4.2).
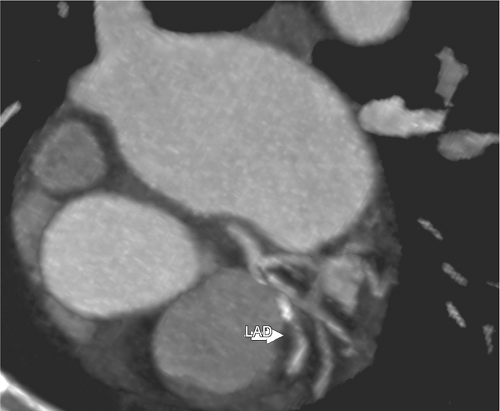 FIGURE C4.1 Left anterior oblique view of the LAD. Severe disease is noted in the proximal segment (arrow). LAD, left anterior desending artery. |
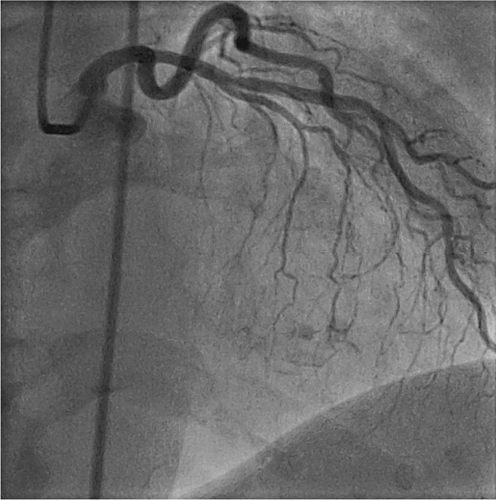
Cardiac catheterization is then performed based on the findings on CTA. The LAD has a proximal 80% stenosis and severe disease at the ostium and proximal segment of the ramus (Figures C4.3 and C4.4) (Cine C4.1 and C4.2). The proximal circumflex artery also reveals significant disease. Multiple views are obtained of the right PDA when the lesion described on CTA is not seen in the traditional right anterior oblique (RAO) view (Cine C4.3). In the left anterior oblique (LAO) projection, a long, severe stenosis is observed in the proximal segment of the PDA (Cine C4.4 and C4.5).
 FIGURE C4.4 Axial view of the distal right coronary artery, demonstrating severe disease (arrow). PLA, Posterolateral artery. |
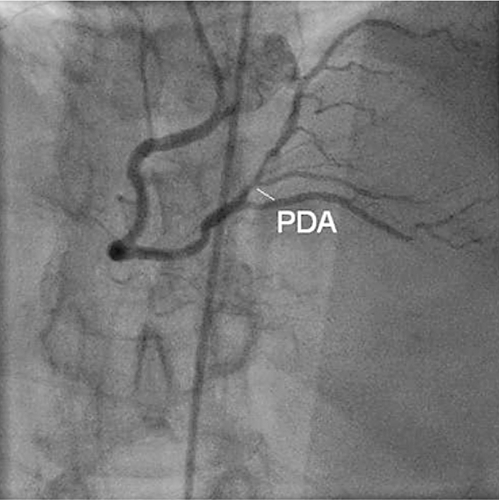 FIGURE C4.5 Coronary angiography of the right coronary artery, right anterior oblique cranial view. PDA, posterior descending artery. |
The patient is referred for coronary artery bypass surgery, and undergoes grafting of the LAD with a left internal mammary artery (LIMA) graft and saphenous vein grafts to the ramus, PDA, and distal RCA. She remains clinically stable and asymptomatic.
Video Clips: C4.1 Video of the left coronary system, left anterior oblique cranial view; C4.2 Video of the left coronary system, left anterior oblique caudal view; C4.3 Video of the right coronary artery, right anterior oblique caudal view; C4.4 Video of the right coronary artery, left anterior oblique caudal view; C4.5 Video of the right coronary artery, right anterior oblique cranial view.
CASE 5: Effect of High Calcium Score and Inaccuracy of Resultant Interpretation
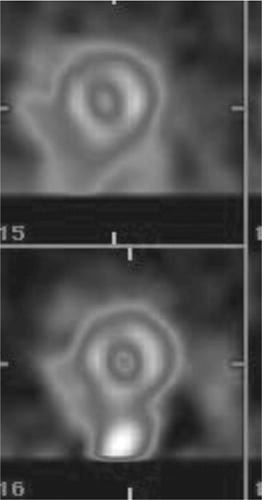
An 83-year-old woman presents with atypical chest pain for which she undergoes a stress myocardial perfusion imaging study. The perfusion images reveal an anteroapical fixed defect with some reversibility (Figures C5.1, C5.2 and C5.3). After much discussion, the patient refuses a cardiac catheterization for further evaluation and opts for coronary CT angiogram instead.
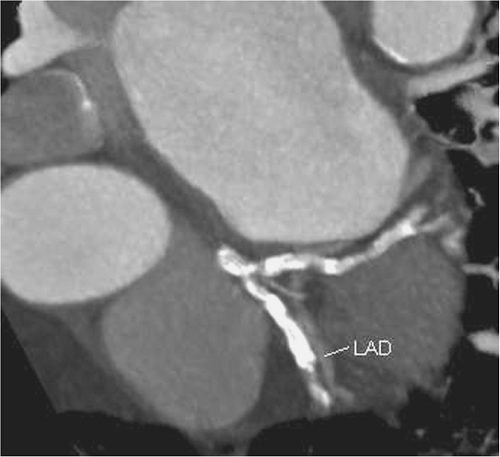 FIGURE C5.2 CT angiogram: In this left anterior oblique cranial view, severe disease is visualized in the LAD (arrow). LAD, left anterior descending artery. |
 FIGURE C5.3 CT angiogram, anterior view of the right coronary artery: calcification is observed throughout the course of the vessel. |
On CTA, the calcium score is elevated at 1922 units. Large, dense calcified plaques obscure the left main, LAD, and circumflex arteries (Figures C5.4 and C5.5). The distal LAD is thought to be sub-totally or totally occluded. The RCA also reveals moderate calcification (Figure C5.6). Accurate interpretation of underlying stenosis is not possible and the patient is referred for cardiac catheterization.
 FIGURE C5.4 Stress (top) and rest (bottom) myocardial perfusion imaging study, vertical long-axis view. This demonstrates a fixed apical defect with subtle reversibility. |
On coronary angiography, the lumen of the left main shows mild disease, and the disease in the proximal LAD and circumflex is 40%–50% in severity (Cine C5.1–C5.3). The distal LAD is occluded. The RCA demonstrates mild luminal irregularities (Cine C5.4). The patient is started on medical therapy.
Video Clips: C5.1 Cineangiography, left coronary system, left anterior oblique caudal view; C5.2 Cineangiography, left coronary system, right anterior oblique caudal view; C5.3 Cineangiography, left coronary system, right anterior oblique cranial view; C5.4 Cineangiography, right coronary artery, left anterior oblique cranial view.
CASE 6: Correlation Between Stress Test and Cardiac Catheterization
A 53-year-old woman, an avid runner, presents for self-referred CT angiography for “screening” for coronary artery disease. She denies cardiac symptoms at the time of the scan. On CT angiography, a complex atherosclerotic plaque is visualized in the proximal LAD, resulting in a luminal stenosis of 60%–70% (Figure C6.1, C6.2 and C6.3). The patient is referred to a cardiologist.
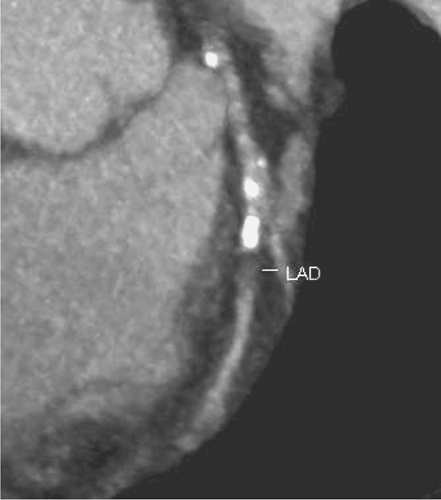 FIGURE C6.1 CT angiogram, anterior view. This displays the mixed plaque and severe disease in the LAD. LAD, left anterior descending artery. |
 FIGURE C6.3 CT angiogram, right anterior oblique cranial view. LAD, left anterior descending artery. |
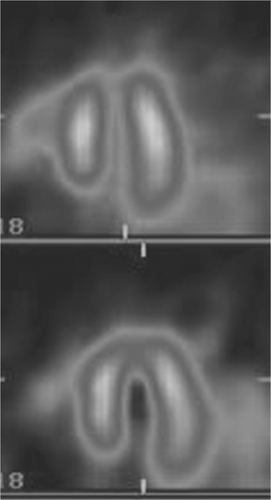
A detailed history reveals mild “chest pressure” while running, never occurring at rest. A stress myocardial perfusion study is ordered, which reveals a moderate sized reversible defect in the anterior wall (Figure C6.4, C6.5 and C6.6).
 FIGURE C6.4 Stress (top) and rest (bottom) myocardial perfusion imaging study, horizontal long axis view. |
 Get Clinical Tree app for offline access 
|