CNS Lymphomas
Overview
CNS lymphomas are extranodal, non-Hodgkin’s lymphomas confined to the brain and spine comprised of malignant lymph tissues. Vast majority (˜90%) are diffuse large B-cell lymphomas arising inside the central nervous system (CNS) without systemic disease, and the remaining 10% are a heterogeneous group made up of mucosa-associated lymphoid tissue (MALT) lymphoma of the dura, intravascular large B-cell lymphoma, anaplastic large cell lymphoma, and immunodeficiency-associated lymphoma.
|
Diffuse Large B-cell CNS Lymphoma
Definition: Malignant neoplasm comprised of mature large B-cell lymphocytes confined to the CNS at presentation and commonly referred to as primary CNS lymphoma (PCNSL) or diffuse large B-cell CNS lymphoma (DLBCL).
Epidemiology: Up to 3% of all brain tumors primarily affecting older adults with peak incidence during the fifth to seventh decades of life, median patient age of 56 years, and the female-to-male ratio of 2:3.
Molecular and genetic profile: The pathogenesis of PCNSL remains largely unclear, but aberrant somatic hypermutation has a major impact on the pathogenesis of PCNSL with the expression of the following genes—BCL6, BCL2, MYC, PIM1, PAX5, RHOH, KLHL14, OSBPL10, and SUSD2.
CSF markers: The presence of lymphoma cells in cerebrospinal fluid (CSF) is sufficient to diagnose PCNSL without the need for brain biopsy. Immunophenotyping using flow cytometric analysis and polymerase chain reaction (PCR) analysis of CSF can aid in distinguishing malignant and reactive lymphocytes in CSF.
Clinical features and standard therapy: Clinical presentation of PCNSL depends on the location of tumor, but patients most commonly present with signs and symptoms of mass effect or seizure. The current standard therapy for newly diagnosed PCSNL is high-dose intravenous methotrexate (antifolate and antimetabolite)-based chemotherapy with additional agents including temozolomide, rituximab, etoposide, and cytarabine.
Prognosis: With prompt diagnosis and treatment, there is a trend toward a survival increase in more recent years, especially in those patients enrolled in clinical trials with aggressive multidrug chemotherapy regimens. However, the prognosis of patients with PCNSL is guarded, with overall survival at 53%, 38%, and 26% at 1, 2, and 5 years after diagnosis, respectively.
Imaging of Primary CNS Lymphoma or Diffuse Large B-cell CNS Lymphoma
PCNSL usually presents as single or multiple solid, avidly enhancing, and homogeneously intraparenchymal masses with exuberant surrounding vasogenic edema and mass effect.
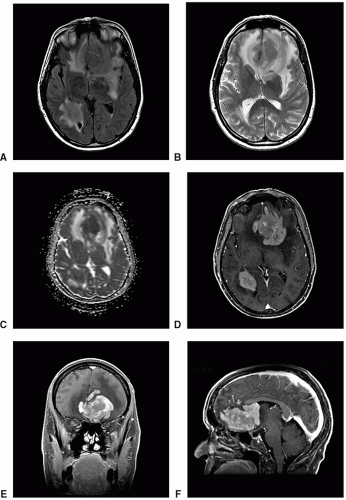
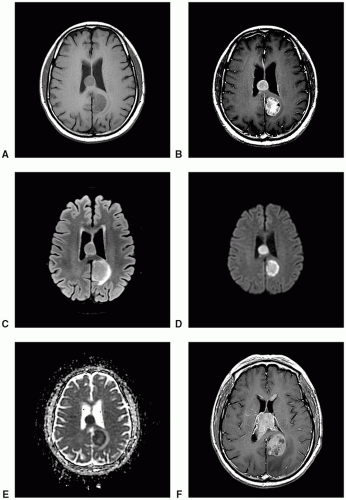
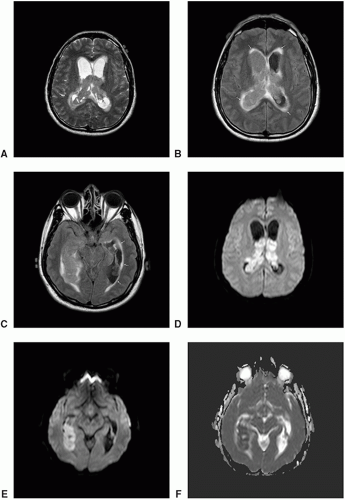
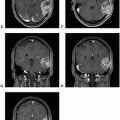
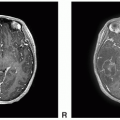
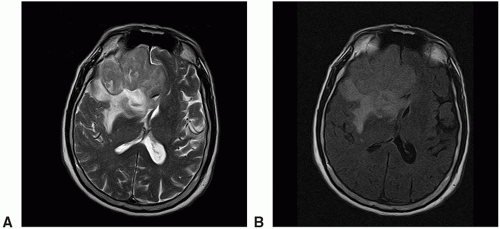 Figure 4.4. Imaging of CNS lymphoma. A. Axial T1 precontrast: Hypointense two solid masses. B. Axial T1 postcontrast: Avid but heterogeneous enhancement. |
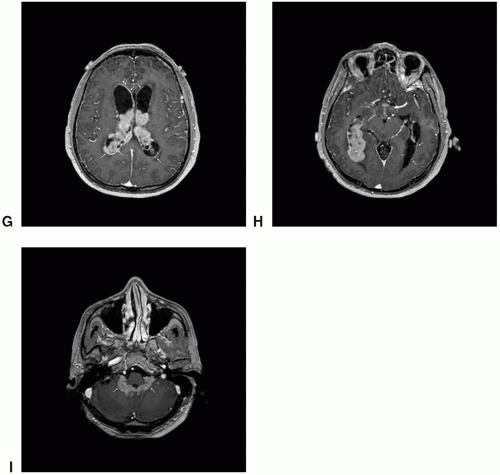
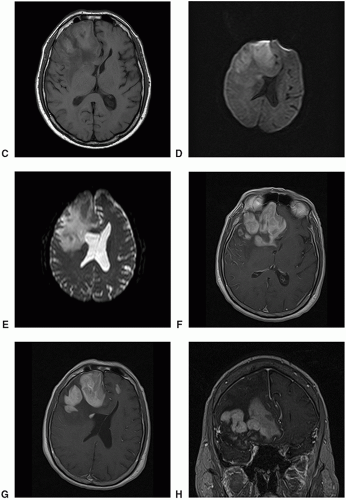 Figure 4.4. (continued) C. Axial FLAIR: Hypointense solid masses. D. DWI: Homogeneously high-signal intensity on DWI. E. ADC: Homogeneously reduced on ADC map. F. Axial T1 postcontrast (4 months follow-up): Growth of two solid masses and bifrontal subependymal spread of tumor. G-I. Axial T1 (G), coronal T1 (H), and sagittal T1 (I) postcontrast images: Bulky solid masses with avid enhancement; the largest conglomerate mass in the right inferior frontal gyrus and additional subependymal and left frontal tumor.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|