Color Doppler and Duplex Ultrasound Imaging of Peripheral Arteries
Joseph F. Polak
Carotid Artery Disease
Indications
1. To detect the presence and degree of carotid artery stenosis in patients with neurologic symptoms
2. To evaluate individuals with carotid bruits
3. To detect recurrent stenosis following carotid endarterectomy and carotid stent placement
4. To monitor patients with known carotid stenosis for disease progression
5. To evaluate patients undergoing extensive cardiac procedures for significant asymptomatic carotid artery disease
Contraindications
Open wounds
Preprocedure Preparation
None
Procedure
1. Equipment: a 5 MHz or greater linear array transducer with color Doppler frequency of 3 MHz or more
2. The examination is performed with the patient supine, head rotated away from the side being evaluated.
3. The transducer is placed in the transverse plane and moved from the low common carotid artery to above the bifurcation of the internal and external carotid arteries. This is used to survey carotid artery anatomy and identify key landmarks.
4. The transducer is placed longitudinally, parallel to the artery. The color Doppler window is angled 20 degrees in either direction or vertically depending on the angle between the transducer surface and the artery. The color Doppler velocity scale is typically set at 20 to 30 cm per second. The transducer is sequentially moved to evaluate the full length of the common carotid and internal carotid arteries. The external carotid artery is evaluated in its proximal portion.
5. The examination begins at the common carotid artery and includes Doppler tracings from the low and upper common carotid artery; the external carotid artery; and the proximal, mid, and distal internal carotid arteries. Doppler velocity waveforms are obtained at sites of abnormal color signal (increased velocity). Doppler velocities are measured before, at, and just distal to the site of abnormal blood flow velocity. A velocity ratio is calculated from the peak systolic velocity (PSV) at the point of increased velocity in the internal carotid artery peak systolic velocity (ICA PSV) divided by the common carotid artery peak systolic velocity (CCA PSV) measured 2 to 4 cm proximal to the common carotid bulb.
6. Apparent absence of blood flow signals is confirmed with power Doppler imaging because it is more sensitive to low-velocity signals than color Doppler.
7. Following carotid endarterectomy or stent placement, imaging should include the artery segment below the site of intervention, a thorough sampling of the area of intervention, and the artery segment downstream from the site.
Postprocedure Management
None
Results
1. The degree of carotid narrowing is estimated using Doppler velocity values calibrated against the degree of stenosis measured on arteriography according to the North American Symptomatic Carotid Endarterectomy Trial (NASCET) method (residual lumen at the stenosis compared to the ICA diameter distal to the stenosis) (1). In the presence of plaque, a 50% to 69% (diameter) stenosis corresponds to a PSV of 125 cm per second or greater (2) but less than 230 cm per second, whereas a greater than 70% stenosis corresponds to a velocity above 230 cm per second (3). An ICA PSV/CCA PSV velocity ratio of 2 to 4 corresponds to a 50% to 69% stenosis and a ratio of more than 4 to a greater than 70% stenosis (4).
2. Very high-grade ICA stenoses can cause a decrease in velocities and a lowresistance pattern (tardus-parvus waveform) (5) distal to the lesion. Color Doppler and power Doppler imaging are then used to confirm the presence of a very narrow residual lumen (6) (Fig. e-67.1). Distinguishing between a subtotal occlusion and a total occlusion can be difficult (7) and may require confirmation by magnetic resonance angiography (8) or computed tomographic angiography (9).
3. Blood flow velocities can be moderately elevated for up to 1 year following standard carotid endarterectomy. Following patch endarterectomy, the lumen of the artery can be enlarged to the point that areas of blood flow stagnation can occur (10).
4. The presence of a carotid stent is often associated with an artificial increase in blood flow velocities. Grading of stent stenosis can be based on a velocity ratio greater than 2.7 or a PSV greater than 220 cm per second for a 50% stenosis and higher values such as a PSV of 340 cm per second for reintervention on a stenosis greater than 80% stenosis (11).
Complications
None
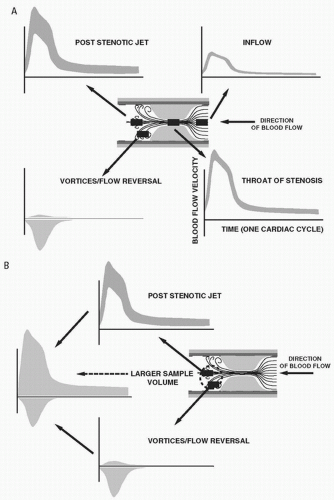 FIGURE e-67.1 • A: Blood flow proximal to a high-grade stenosis is laminar. At the stenosis proper, all the red cells tend to travel at the same velocity (blunt flow profile or plug flow). The spectrum is therefore narrower than that sampled in the artery proximal to the stenosis, and it has a larger amplitude because all of the red cells must pass through the orifice. Distal to the stenosis, a more distinct jet of increased velocities develops surrounded by a zone of flow reversal. The jet is often asymmetric, hitting one or the other of the arterial walls rather than being directed toward the center of the artery. The zone of flow reversal is seen as a site where eddy currents cause the blood to flow back on itself. The jet will continue to dissipate energy as its effective radius grows. At the appropriate velocity/effective radius, turbulence will occur. B: Distal to the stenosis, it is possible to obtain a combination of forward- and backward-moving red cells. If the sample gate is large enough and placed at the interface between the zone of flow reversal and the velocity jet, a complex blood flow pattern will be registered. (From Polak JF. Peripheral Vascular Sonography. 2nd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2004, with permission.) |
Renal Artery Disease
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





