Color Doppler and Ultrasound Imaging of Peripheral Veins
Joseph F. Polak
Veins of the Lower Extremity
Indications
1. To evaluate patients with acute onset of lower extremity swelling or pain, raising the clinical suspicion of acute deep vein thrombosis (DVT)
2. To monitor the veins of high-risk, asymptomatic patients. The definition of “high-risk” is extensive and includes elderly, bedridden, postsurgery (especially those who have had hip replacement or neurosurgical procedures) (1), or patients following trauma (2).
3. To establish a baseline study following the completion of anticoagulation. This will permit the detection of recurrent episodes of DVT or onset of venous reflux (3).
4. To evaluate patients with dyspnea and suspected pulmonary embolism (4), although the diagnostic yield is low
5. To monitor in-hospital quality control programs aimed at the prophylaxis of DVT, particularly in high-risk groups of patients (5)
6. Preoperative mapping of the great and small saphenous veins
7. Detection and segmental analysis of venous reflux in patients with
a. Varicose veins
b. Recurrent varicose veins after intervention
c. Cutaneous ulceration
d. Serious venous stasis complaints with or without subcutaneous induration
Contraindications
Relative
1. Difficulty of the examination is a function of body habitus and the transducer used (5.0 MHz or 7.5 MHz).
2. Recent surgical or skin wounds along sites to be surveyed
3. Painful extremity that does not permit adequate application of pressure to the skin surface overlying the vein segment that is being evaluated
Preprocedure Preparation
1. No patient preparation is needed.
2. Intensive care patients can be examined with portable units.
3. Equipment
a. Inferior to the inguinal ligament, high-resolution B-mode imaging is performed with a linear array transducer with color Doppler and duplex imaging capability. Transducer grayscale frequency is 5 MHz or above; Doppler frequency is 3 MHz or above. Pressure is applied by pushing the transducer down on the skin in order to compress the underlying vein. Color Doppler imaging and Doppler waveform analysis are used for evaluating blood flow patterns.
b. A sector or curved array transducer is used above the inguinal ligament, in the iliac veins, and inferior vena cava (IVC). The imaging and Doppler frequencies are lower. The gain is set so that the lumen of a normal vessel is free of internal echoes. The accompanying artery is used as a reference.
c. Color Doppler imaging is complementary to the compression maneuver and is useful in demonstrating blood flow and detects nonobstructive thrombus in the IVC, iliac, thigh, and calf veins. It is also used to detect venous reflux.
d. Tilt tables or reclining stretchers held in reverse Trendelenburg position (feet down) help to evaluate patients who have difficulty moving and to passively distend the veins during the evaluation of venous reflux.
Detection of Deep Vein Thrombosis
Procedure
1. Compressibility of the vein walls is the most important and reproducible criterion to exclude the presence of acute thrombus (Figs. e-69.1, e-69.2, e-69.3).
a. Interrogation of the veins should ideally begin at the level of the inguinal ligament, roughly at the groin crease, and continue to include the calf veins.
b. Examination of the femoral veins: The patient is positioned supine with the leg to be examined in slight external rotation. The patient’s head/torso may be elevated 15 to 20 degrees (reverse Trendelenburg) to facilitate venous filling. The examination includes Doppler interrogation of the common femoral and femoral veins, including the proximal portion of the great saphenous vein at the saphenofemoral junction just below the inguinal ligament.
c. The transducer is held transverse to the axis of the vein and centered on the vein segment as pressure is applied on the skin to compress the vein walls. The walls of a normal vein segment collapse and appose together with minimal pressure. The failure to coapt the vein walls with compression while the accompanying artery is deformed is regarded as a positive finding for intraluminal thrombus.
d. The compression maneuver is performed along the length of the vein by having the operator displace the transducer every 2 to 3 cm staying centered on the vein and then pressing on the skin.
e. The femoral vein may be difficult to compress because it passes through the adductor canal. This can be the site of a false-positive study; adjunctive imaging with color Doppler imaging can help evaluate the patency of the venous segment or confirm the presence of a thrombus.
f. The saphenofemoral junction may be difficult to compress. This area should be carefully examined because thrombus in the great saphenous vein near
the femoral junction may propagate into the common femoral vein, thereby becoming a deep vein thrombus.
the femoral junction may propagate into the common femoral vein, thereby becoming a deep vein thrombus.
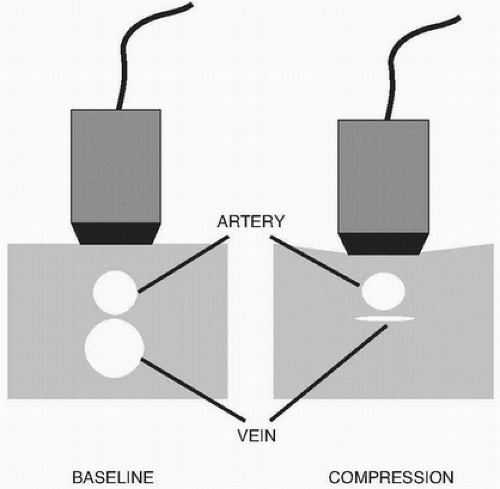 FIGURE e-69.1 • The compression maneuver is performed with the transducer held transverse to the vein. Pressure is applied to the surface of the skin through the transducer. This is transmitted to the deeper structures and causes the vein walls to collapse. On real-time imaging, repeating this maneuver causes the vein to wink. The maneuver shown here was applied to the femoral vein, which lies deep to the artery. The artery should not deform before the vein. On rare occasions, we have seen the artery collapse before the vein in patients with a prominent sartorius muscle. Reorienting the transducer more medially on the inside of the leg and repeating the compression maneuver then led to a normal response. (From Polak JF. Peripheral Vascular Sonography. 2nd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2004, with permission.) |
g. The popliteal vein is examined with the leg slightly flexed. Alternatively, the patient can be imaged prone with the calf elevated approximately 30 degrees, with a towel or pillow beneath the shin to prevent spontaneous collapse of the vein. The patient can also be examined in the decubitus position.
h. The popliteal vein is compressed from the adductor hiatus to the level of the calf veins.
i. The transducer is occasionally placed over the anterior compartment between the tibia and fibula in order to evaluate the paired anterior tibial veins. Isolated thrombosis of the anterior tibial veins is very rare.
j. The paired posterior tibial and peroneal veins are in the posterior compartment and can be found by displacing the transducer medially and posterior to the tibia. The posterior tibial artery and accompanying paired veins lie medial and posterior to the tibia. The peroneal artery and accompanying veins are located deeper on top of the fibula.
k. The paired gastrocnemius veins accompany the gastrocnemius artery in the gastrocnemius muscle. Compressibility is mainly used for the diagnosis of thrombosis.
l. The muscular (mostly soleal) veins lie within the deep muscles of the calf and typically communicate with the peroneal and posterior tibial veins. Compressibility is mainly used for the diagnosis of thrombosis.
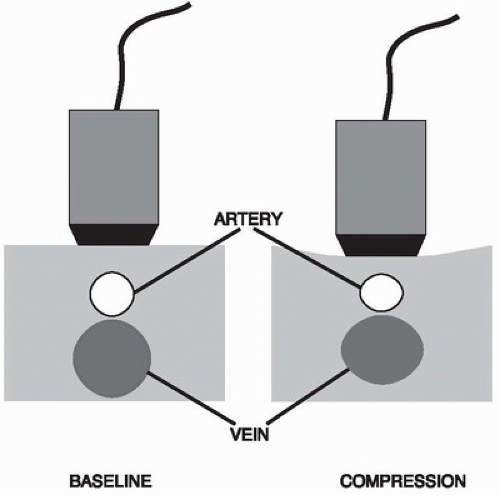 FIGURE e-69.2 • Abnormal compression ultrasonography is defined as a failure to appose the walls of the deep vein while pressure is applied onto the skin through the transducer. Sufficient pressure is exerted to the extent that the artery wall deforms slightly. An ancillary finding to the presence of DVT is distension of the vein. The additional presence of echogenic material in the vein lumen reinforces the diagnosis. (From Polak JF. Peripheral Vascular Sonography. 2nd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2004, with permission.) |
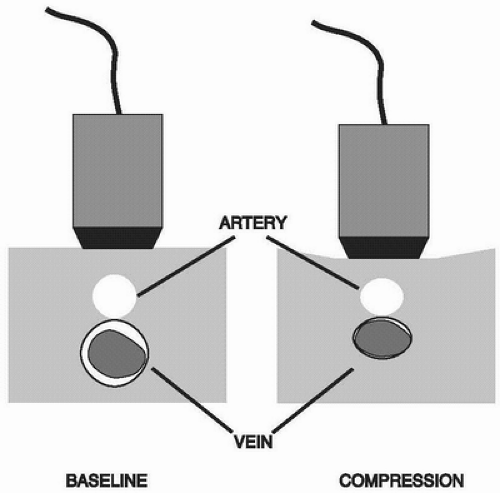 FIGURE e-69.3 • Compression ultrasonography will also detect the presence of partly obstructing thrombus. There is failure for the walls of the vein to completely oppose during the compression maneuver. The vein is not distended. An echogenic structure need not be visualized in the vein lumen. (From Polak JF. Peripheral Vascular Sonography. 2nd ed. Philadelphia, PA
Get Clinical Tree app for offline access
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree


|


