Congenital Malformations
MYELOMENINGOCELE AND MYELOCELE
KEY FACTS
Myelomeningocele and myelocele are both midline bone defects through which meninges and/or neural placode (unfolded spinal cord) are visible; most discovered by in utero sonography or magnetic resonance imaging (MRI).
In a myelomeningocele (the most common type, 0.1% of live births), the neural placode and meninges protrude above the skin; it almost always is seen in the context of a Chiari 2 malformation and is generally sporadic but may affect subsequent siblings.
In a myelocele (less common), the neural placode is flush with the skin.
Both entities are untethered and closed at birth, and imaging is done for recurrent symptoms. Prenatal surgery is effective in closing it and minimizing intracranial findings of Chiari 2 and hydrocephalus.
For practical purposes, after repair of one of these defects, all spinal cords are retethered (due to scar), and imaging studies are mainly used to exclude other abnormalities, such as syringomyelia (30% to 75%), diastematomyelia (30%), lipomas, dermoids, and epidermoids.
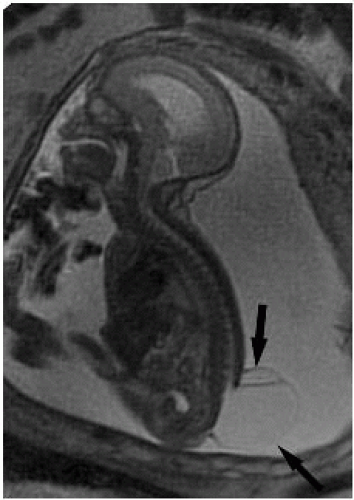 FIGURE 26-3. Sagittal in utero T2 shows large CSF-filled sac (arrows) containing nerve roots superiorly. The sac herniates through a spina bifida. Hydrocephalus and polyhydramnios are present. |
SUGGESTED READING
Aaronson OS, Hernanz-Schulman M, Bruner JP, Reed GW, Tulipan NB. Myelomeningocele: prenatal evaluation—comparison between transabdominal US and MR imaging. Radiology 2003;227:839-843.
LIPOMYELOMENINGOCELE AND LIPOMYELOCELE
KEY FACTS
Both lipomyelomeningocele and lipomyelocele refer to a midline bone spinal defect covered by skin that may have a dermal sinus, hairy patch, or hemangioma above the intergluteal fold.
In a lipomyelocele, meninges and neural placode are located at the level of a spina bifida but covered by a lipoma and skin.
In a lipomyelomeningocele, the meninges and neural placode protrude through a bone opening but are covered by a lipoma and skin; this lipoma is in direct contact with the surface of the neural placode, and the patients have a prominent mass in the low back.
Both lesions may be detected at birth or be mostly clinically silent and not found until adulthood.
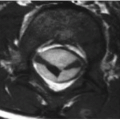
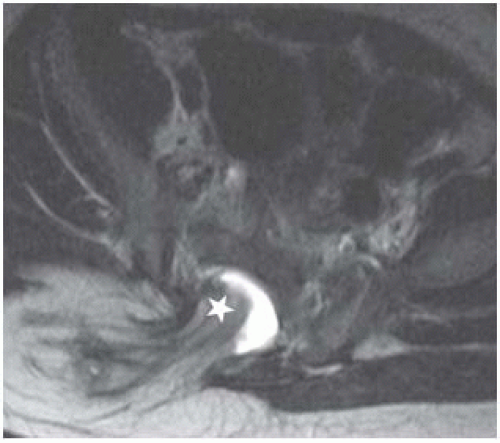 FIGURE 26-5. Axial T2, in the same patient, shows intraspinal extension (star) of subcutaneous lipoma. |
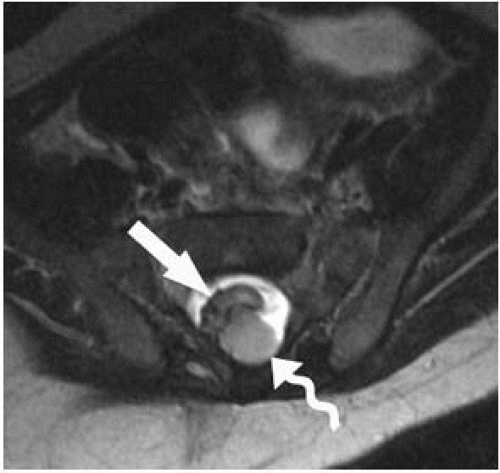 FIGURE 26-6. Axial T2 cephalad to 2 shows placode (arrow) and closely associated lipoma (wavy arrow) posteriorly. |
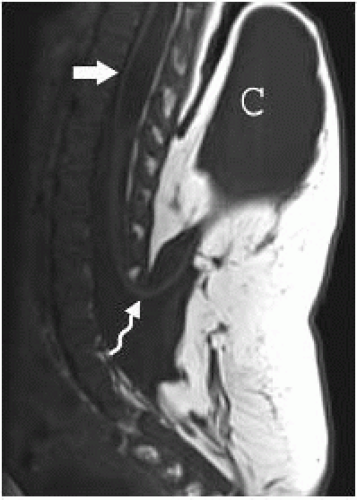 FIGURE 26-7. Midsagittal T1, in a different patient, shows cord (wavy arrow) extending into sac (C) as well as a syrinx (arrow). |
SUGGESTED READING
Medina S, Al-Orfali M, Zurakowski D, Poussaint TY, DiCanzio J, Barnes PD. Occult lumbosacral dysraphism in children and young adults: diagnostic performance of fast screening and conventional MR imaging. Radiology 1999;211:767-771.
LIPOMAS
KEY FACTS
A filar lipoma is the most common intraspinal lipoma; it occurs in 1% to 6% of the population and is generally an incidental and asymptomatic finding.
With a filar lipoma, the filum terminale is thickened (generally, its normal size should not exceed that of neighboring nerve roots) and has fat within it.
In the presence of a filar lipoma, if the conus medullaris is normal in position, then the findings are probably not clinically significant; however, if the conus medullaris is abnormally low, consider the diagnosis of the tight filum terminale syndrome.
Intradural lipomas are rare and are mostly found in the cervical region but may occur anywhere in the spine; most become symptomatic by 5 years of age and result in paresis, spasticity, sensory loss, weakness, and bowel/bladder dysfunction.
Main differential diagnosis: dermoid/epidermoid, teratoma.
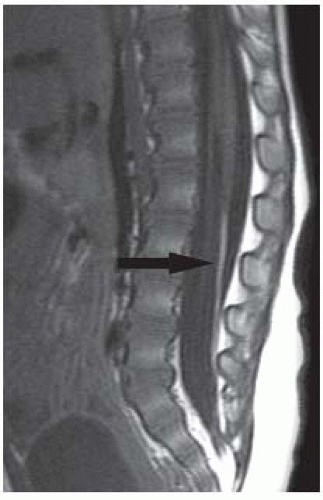 FIGURE 26-8. Midsagittal T1 shows bright fat (arrow) in the filum terminale, but the conus is located at a normal height. |
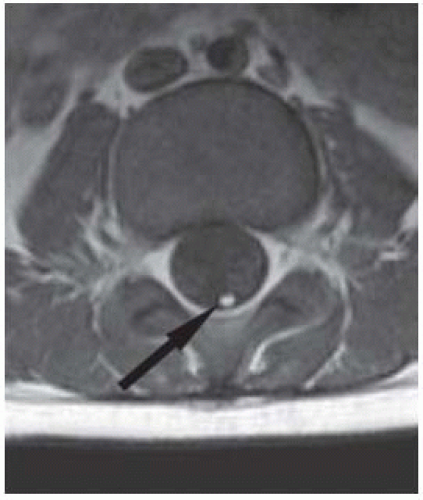 FIGURE 26-9. Axial T1, in the same patient, shows filar lipoma (arrow).
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|