Diagnostic Venography
Rulon L. Hardman
Krishna Kandarpa
Diagnostic venography is performed only when noninvasive imaging is nondiagnostic or prior to a contemplated intervention. It is an infrequent first-line modality because of the accuracy of noninvasive imaging—both for peripheral (Doppler ultrasound) and central (computed tomography venography [CTV]/magnetic resonance venography [MRV]) veins. Preintervention venography is discussed in the appropriate chapters. The discussion here is restricted to the careful technique required for performing high-quality, diagnostic venography.
Indications
Lower Extremity Venography
1. Diagnosis of deep vein thrombosis (DVT) following nondiagnostic or incomplete ultrasound examination; also, when there is a high clinical suspicion for DVT but an extremity ultrasound study is negative
2. Planning for catheter-directed venous thrombolysis
3. Evaluation of venous malformations
4. Evaluation of venous encasement by tumor
5. Evaluation of venous reflux and valvular incompetency by descending lower extremity venography
Upper Extremity Venography
1. Diagnosis of superficial thrombosis or DVT following nondiagnostic or incomplete ultrasound examination
3. Evaluation for external compression of the axillary-subclavian vein secondary to clavicular fracture, thoracic outlet syndrome, or neoplastic compression
4. Presurgical mapping for hemodialysis access (2)
5. Planning for complicated central venous access or evaluation following a complication of central venous access
Contraindications
Relative
1. Previous contrast reaction (premedicate if necessary)
2. Renal insufficiency
3. Pregnancy—complement venography with duplex ultrasound and MRV to minimize radiation to the fetus. Use lead shielding over pelvis during fluoroscopy.
4. Severely compromised cardiopulmonary status
Preprocedure Preparation
1. Clarify the indication for the procedure.
2. Review all prior ultrasounds, venous plethysmography, and available crosssectional imaging.
3. Restrict oral intake to clear liquids; nil per os (NPO) if planning conscious sedation (as guided by hospital policy).
4. Evaluate recent creatinine and hydration status, especially in patients with diabetes.
a. If a large contrast volume is anticipated, intravenous (IV) hydration may be appropriate.
b. Hold metformin in patients with diabetes and/or compromised renal function; restart following creatinine evaluation in 48 hours.
5. Obtain informed consent.
Procedure
Of the several variations of ascending lower extremity venography reported, the two most commonly cited are the Greitz technique (as modified by Rabinov and Paulin) and the Thomas technique (5,6). A combination of these methods, which were developed with overhead filming incorporated for conventional fluoroscopic rooms, is described. Tilting fluoroscopic tables now have integrated digital subtraction imaging, which permits further modification of these techniques.
1. Patient is positioned on a fluoroscopic tilt table, preferable with integrated digital subtraction angiography (DSA) capability. A 6-in. or 12-in. footrest is used to support the contralateral leg. The knee of the extremity being studied can be supported in 30 degrees of flexion with a foam pad to improve flow through the popliteal vein. Avoid excessive external compression, which can obstruct the popliteal vein.
2. Access a peripheral vein on the dorsum of the foot with a 20-gauge or 21-gauge butterfly needle or small peripheral IV catheter. Direct the needle toward the toes if possible to aid in filling the deep veins. If extravasation is seen, leave the catheter in place and select another location for access.
a. A swollen foot can lead to compression of the superficial veins.
(1) Elevate the extremity for several hours prior to the procedure, and/or
(2) Wrap the foot in elastic bandage for 30 to 60 minutes or longer, as necessary.
b. Collapsed, poorly visible veins
(1) Keep the extremity in a dependent position, and/or
(2) Apply warm compresses to the dorsum of the foot.
(3) Ultrasound guidance is now routinely used to aid difficult access.
3. Infusion setup. Attach a three-way stopcock, with inputs for a contrast syringe and heparinized saline syringe or bag.
4. Venography is performed with nonionic, low-osmolar or iso-osmolar contrast with concentration between 200 mg per mL and 300 mg per mL. High concentration (350 mg per mL) contrast may not mix as well with blood as a lower concentration. Routine venography usually requires between 50 mL and 100 mL of contrast.
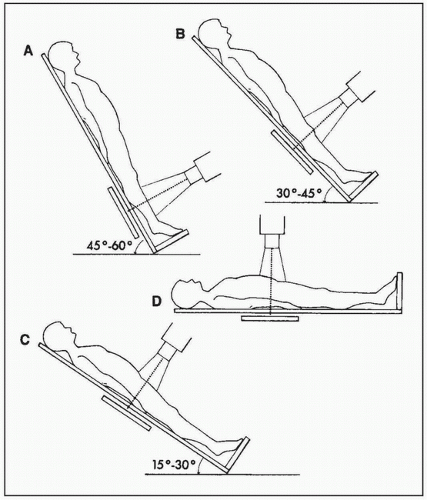 FIGURE 2.1 • Tilt table ascending leg venography. Spot images are obtained as follows. A: Below the knee with table tilted 45 to 60 degrees: AP and lateral projections. B: Over the knee with table tilted 30 to 45 degrees: AP and lateral projections. C: Over the thigh and groin with table tilted 15 to 30 degrees: AP projection. D: Supine frontal overhead image of pelvis and lower abdomen. A Valsalva maneuver, performed during elevation of the examined leg, facilitates opacification of the iliac veins and inferior vena cava. (From Kim DS, Orron DE. Peripheral Vascular Imaging and Intervention. St. Louis, MO: Mosby Year Book; 1992:284, with permission.) |
5. Standard views (Fig. 2.1)
a. With the table upright at 45 to 60 degrees, gently inject contrast by hand and periodically assess the vein puncture site for extravasation. Barring none, follow the IV contrast column intermittently with fluoroscopy until contrast reaches the popliteal vein (about 50 mL).
b. Obtain anteroposterior (AP) and lateral spot views of the lower leg (anterior tibial, posterior tibial, and peroneal veins) by manually rotating the extremity or the C-arm. Magnified views are obtained at any area of discontinuous or clot-filed vein.
c. AP spot views of the popliteal vein are obtained with the table at 30 to 45 degrees. Bilateral oblique views are recommended.
d. AP views of the thigh are obtained with a decrease tilt to 15 to 30 degrees. Flow may be brisk through the thigh and digital imaging at one or two frames per second may be required.