Dialysis Fistulae
Aalpen A. Patel
Scott O. Trerotola
An estimated 2.5 million patients worldwide receive renal replacement therapy and 450,000 of those patients are from the United States. In the mid-1990s, the National Kidney Foundation began an effort to give evidence-based guidance to the teams caring for dialysis patients. The Disease Outcomes Quality Initiative (DOQI) recommendation document was published in 1997. In 2000, the scope was expanded to include chronic kidney disease even before the need for dialysis arises. This effort is now termed the Kidney Disease Outcomes Quality Initiative (NKF-KDOQI) (1). The Vascular Access section was last updated in 2006.
Long-term dialysis access is created via the surgical construction of an arteriovenous (AV) shunt. This connection between an artery and a vein may be created by using native conduits (native arteries and veins), artificial conduits (grafts), or hybrid conduits. This chapter will address native arteriovenous fistulae (AVF).
The NKF-KDOQI document recommends that when possible, the order of preference for site of AVF placement should be (a) radiocephalic (wrist), (b) brachiocephalic (elbow), and (c) transposed brachial-basilic. An arteriovenous graft (AVG) should only be considered if AVF creation is not possible.
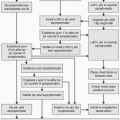
Regular assessment of AVF should be performed to detect hemodynamically significant stenosis because it has been proven in a randomized trial that treatment of hemodynamically significant anatomic stenoses in fistulae reduces the incidence of access thrombosis and improves patency (2). The following complementary methods may be used as part of a quality assurance program. Physical examination and evaluation for such findings as arm swelling, development of collateral veins, prolonged bleeding, change in flaccidity of fistula, and change in outflow vein should be performed by a qualified health care professional on a monthly basis, which is termed monitoring. If special instrumentation is used to perform evaluation of the AVF at periodic intervals, it is termed s urveillance. Direct flow measurements and duplex ultrasound are preferred methods of surveillance. A detailed discussion of each method is beyond the scope of this chapter, and readers requiring more information should refer to the NKF-KDOQI document. It is important to note that a single abnormal test result should not trigger a response; it is an abnormal trend or persistent abnormality that should result in further steps.
Indications
1. Failure of the AVF to mature. The first access evaluation should occur 6 weeks after creation.
a. Diagnostic fistulogram, if
(1) Flow <600 mL/min
(2) Draining vein <6 mm in diameter
b. Angioplasty of stenosis anywhere in circuit up to the central veins; there is no evidence that central venous stenosis affects maturation.
c. Embolization or ligation of “competing” veins. Th is is a controversial issue because there is little evidence that treatment of such vessels helps with maturation (3).
2. Failing AVF. An AVF is thought to be failing when there is inflow or outflow stenosis(es) greater than 50% associated with
a. Decreased flow (decreased clearance)
b. Increased static venous pressure
c. Pseudoaneurysm
d. Prolonged bleeding after needle removal
e. Arm swelling
f. Recirculation
g. Abnormal physical examination
3. Clotted AVF
Contraindications
Absolute
1. Uncorrectable coagulopathy
2. Fistula infection. Note: Fistula infection is very unusual. As opposed to AVGs, erythema and warmth over a clotted AVF nearly always represents thrombophlebitis and not an infection.
Relative
1. Right-to-left cardiopulmonary shunt (for declotting procedures due to the risk of paradoxical emboli)
2. History of contrast reaction
3. Significant cardiopulmonary disease. During declotting procedures, pulmonary emboli can occur. Most of the time, they are without clinical consequences; however, in patients with right ventricular failure, pulmonary hypertension, and cardiac dysrhythmias, fatal pulmonary emboli have been reported.
4. Ischemia distal to the AV anastomosis. Increasing the flow through a fistula may further divert blood from the ischemic area and result in worsening of the steal syndrome.
5. Systemic infection
Preprocedure Preparation
1. Informed consent. This encounter also helps establish a rapport with the patient and helps to ease anxiety.
2. Intravenous (IV) antibiotics should be administered prior to thrombectomy/thrombolysis (cefazolin 1 to 3 g IV [weight based] or vancomycin 0.5 to 1.5 g IV [weight based] because the contents of a clotted fistula may be colonized) (4).
3. Obtaining a history of the current fistula (along with physical examination) is one of the most crucial steps in preprocedure assessment. The following should be assessed and documented:
a. When the access was created
b. Type of access
c. If failure to mature (has there been any prior successful use)
d. When the dysfunction or clotting occurred
e. Presence of steal symptoms
f. Arm, face, or breast swelling
g. Fevers or chills
h. History of prior interventions
4. Regardless of the type of access, the following should be assessed by physical exam and documented:
a. Pulses: radial, ulnar, and brachial pulses (use Doppler if not palpable)
b. Capillary refill and warmth of the arm/hand
c. Chest wall collaterals
d. Cardiac and pulmonary examination: assessment of the patient’s ability to safely tolerate moderate sedation and the procedure. Those with pulmonary edema may require preprocedure dialysis via temporary catheter.
e. Physical evaluation of the AVF should be performed prior to each intervention.
(1) Type and condition of access (radiocephalic fistula, brachiocephalic fistula, or basilic or cephalic vein transposition), presence of aneurysms, pseudoaneurysms, or hematoma and the location of the anastomosis. This information helps in choice of fistula access site(s).
(2) Presence or absence of thrill/pulse
(3) Assessment whether the fistula is tense or flaccid (even with thrill)
5. Review of the images from prior interventions is critical (especially when there is early failure after a prior procedure). In particular, determine if the previous intervention was optimal. This is a critical step and should not be omitted.
Procedure
Interventions performed in AVFs include fistulography and angioplasty in nonmaturing or failing fistulae and clearing of clot from occluded fistulae (declotting procedures). Each will be described separately.
Fistulography and Percutaneous Transluminal (Balloon) Angioplasty for Nonmaturing Fistulae
1. Assemble the appropriate tools and equipment prior to the procedure:
a. For fistula access: 18-gauge Angiocath or a micropuncture set
b. Guidewires: Roadrunner (Cook Medical, Bloomington, IN) (preferred), Bentson wire, or long-tapered (8-cm taper) Glidewire.
c. Sheaths: high-flow 6 Fr. and/or 7 Fr. short sheaths (4 to 6 cm long) with sidearm
d. Balloons: Ultrahigh-pressure balloons: High pressures are often needed for percutaneous transluminal (balloon) angioplasty (PTA




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree