Dialysis Grafts
Aalpen A. Patel
Scott O. Trerotola
Long-term dialysis access is created via the surgical construction of a connection between an artery and a vein using only the native vessels, or non-native conduits. Non-native conduits include synthetic grafts (polytetrafluoroethylene or polyurethane), biological grafts (bovine heterograft, bovine mesenteric vein, cryopreserved femoral vein, or human umbilical cord vein), or hybrid grafts (with self-sealing composite material or cryopreserved vein). Th is chapter will address the endovascular management of non-native arteriovenous grafts (AVGs).
The Kidney Diseases Outcomes Quality Initiative (NKF-KDOQI) recommendations state that construction of an AVG should only be considered if making a
fistula is not possible (1). The preferred order for AVG creation is a forearm graft (loop graft preferred over straight graft), upper arm graft, and chest wall prosthetic graft (“necklace graft”). Lower extremity AVG is an access of last resort.
fistula is not possible (1). The preferred order for AVG creation is a forearm graft (loop graft preferred over straight graft), upper arm graft, and chest wall prosthetic graft (“necklace graft”). Lower extremity AVG is an access of last resort.
The rationale for monitoring and methods of surveillance are the same as for dialysis fistulae and are discussed in Chapter 31.
Indications
1. Failing AVG. Clinical or hemodynamic abnormality and associated vessel/graft stenosis of greater than 50%, leading to
a. Decreased flow (decreased clearance)
b. Increased venous pressure
c. Pseudoaneurysm
d. Prolonged bleeding after needle removal
e. Arm swelling
f. Recirculation
g. Abnormal physical examination
2. Clotted AVG
Contraindications
Absolute
1. Uncorrectable coagulopathy
2. Graft infection
Relative
1. Right-to-left cardiopulmonary shunt (for declotting procedures due to risk of paradoxical emboli)
2. History of contrast reaction
3. Systemic infection
4. Significant cardiopulmonary disease. During declotting procedures, pulmonary emboli can occur. Most of the time, they are without clinical consequences; however, in patients with right ventricular failure, pulmonary hypertension, or cardiac dysrhythmias, fatal pulmonary emboli have been reported.
5. Ischemia distal to the arteriovenous (AV) anastomosis. Increasing the flow through a graft may further divert blood from the ischemic area and result in worsening of the steal syndrome.
6. AVGs inserted less than 30 days prior to intervention have not formed sufficient perigraft scar tissue and may bleed when punctured. The resulting hematoma may lead to loss of the hemodialysis access altogether or local infection. Patency associated with declotting in this situation is exceedingly poor.
Preprocedure Preparation
1. A physician (preferably the one performing the procedure) or an advanced practitioner (depending on hospital policy or state law) must obtain informed consent. This encounter also helps establish a rapport with the patient and helps to ease anxiety.
2. Intravenous (IV) antibiotics should be administered prior to thrombectomy (cefazolin or vancomycin, based on weight) because the contents of a clotted graft are often colonized (2).
3. Obtaining a history of the current AVG (along with physical examination) is one of the most crucial steps in preprocedure assessment. The following should be assessed and documented:
a. When the access was created
b. Type of access
c. When the dysfunction or clotting occurred
d. Presence of steal symptoms
e. Arm, face, or breast swelling
f. Warmth or erythema of the access site
g. Fevers or chills
h. History of prior interventions
4. Regardless of the type of access, the following should be assessed by physical exam and documented:
a. Pulses: radial, ulnar, and brachial pulses (dorsalis pedis, posterior tibial, popliteal, and femoral pulses for lower extremity grafts). Use Doppler if the pulses are not palpable.
b. Capillary refill and warmth of the arm/hand
c. Chest wall collaterals
d. Cardiac and pulmonary examination. Assessment of the patient’s ability to safely tolerate moderate sedation and the procedure. Patients with pulmonary edema may require preprocedure dialysis via a temporary catheter.
e. Physical evaluation of the graft should be performed prior to each intervention.
(1) Graft site: for warmth and erythema that might indicate graft infection or cellulitis. A graft infection is an absolute contraindication to percutaneous intervention.
(2) Type of access: straight or loop, direction of inflow and outflow, presence of aneurysmal graft degeneration, and the location of anastomoses. Th is information helps in the determination of access site(s).
(3) Presence or absence of a thrill or pulse. Rarely, a patient may be referred with a “clotted graft” that is actually not clotted but has very low flow. In these cases, an inflow lesion should be sought and corrected.
5. Review of the images from prior interventions is critical (especially when there is early failure after a prior procedure). In particular, determine whether the outcome of the previous intervention was optimal.
Procedure
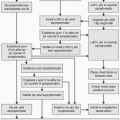
Interventions performed in AVGs include fistulography and angioplasty in failing grafts and clearing of clot from occluded grafts (“declotting procedures”).
Fistulography and Angioplasty for Failing AVGs
1. Assemble the appropriate equipment.
a. For access: 18-gauge Angiocath or micropuncture set